Australia Indonesia Partnership for Health Systems Strengthening is managed by Coffey on behalf of the Australian Department of Foreign Affairs and Trade
Australia Indonesia Partnership for Health
Systems Strengthening (AIPHSS)
Fifth Six Monthly Progress Report
Table of contents
Executive Summary ... i
1 Introduction ... 1
1.1 Background to AIPHSS ... 1
1.2 The AIPHSS Reform Agenda for Health System Strengthening ... 2
1.3 Program Framework ... 4
2 Relevance of AIPHSS ... 8
2.1 Contextual Analysis ... 8
3 Progress towards End of Program Outcomes (EOPOs) ... 10
3.1 An Effective National Health Insurance System ... 10
3.2 Minimum Service Standards (MSS) to support Primary Health Care Delivery ... 12
3.3 Accreditation of Local Health Service Centres ... 14
3.4 Equitable Allocation of Health Resources ... 16
3.5 Governance and Supervision of the Health System ... 19
3.6 Summary of Investment against EOPOs and Building Blocks ... 22
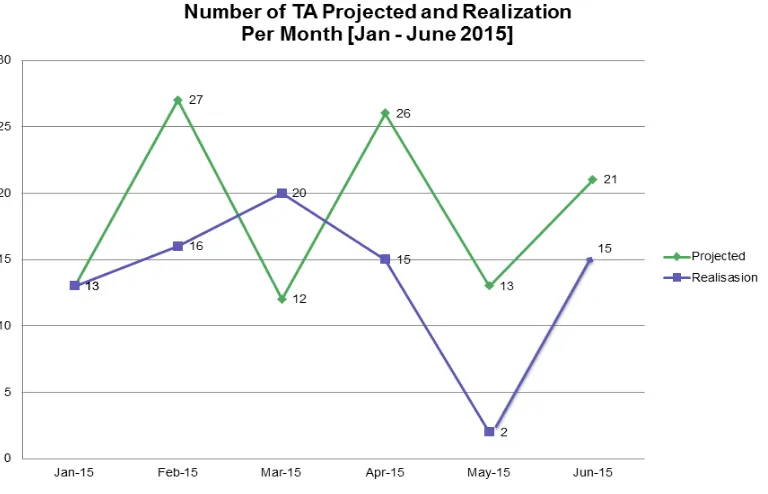
4 Implementation of the 2015 Work Plan ... 23
4.1 Management and Operational Systems ... 23
4.2 Implementation Progress against the Annual Plan ... 28
4.3 Challenges and Emerging Risks ... 32
5 Evaluative Summary ... 33
6 Priorities and Recommendations for the next reporting period ... 34
Annexes
Annex 1 Status of Implementation of Activities (Jan 2015 – June 2015)
Part A – Progress of each AIPHSS intervention (June 2015)
Part B – Actual versus expected expenditure for each AIPHSS intervention (June 2015)
Annex 2 Interventions and their contributions to end of program outcomes (EOPOs)
Annex 3 Status of AIPHSS Policy Notes including their dissemination, use and attributable changes
Annex 4 Policies, Regulations and Guidelines produced during the reporting period and their current status
Annex 5 Risk Matrix
Annex 6 Knowledge Management Strategy – Executive Summary
Annex 7 Technical Assistance and Staff Mobilisation (Jan 2015 – June 2015)
Annex 8 Draft Exit Strategy Outline
Abbreviations
ADINKES Association of Health Office (Asosiasi Dinas Kesehatan)
APBN Indonesian State Budget (Anggaran Pendapatan dan Belanja Negara)
AIPHSS Australia Indonesia Partnership for Health Systems Strengthening
AIPMNH Australia Indonesia Partnership for Maternal and Neonatal Health
ARF Adviser Remuneration Framework
BAPPENAS State Ministry of National Development Planning (Kementerian Perencanaan
Pembangunan Nasional/Badan Perencanaan Pembangunan Nasional (Bappenas)
BAST Record of Transfer (Berita Acara Serah Terima)
BOK Health Operational Funding (Biaya Operational Kesehatan)
BPJS Agency for the Organisation of Social Insurance (Badan Penyelenggara
Jaminan Social)
BUKD Directorate of Basic health Services (Direktorat Jenderal Bina Upaya
Kesehatan)
CPMU Central Program Management Unit
CBG Case Based Group
DFAT Department of Foreign Affairs and Trade
DHA District Health Account
DHO District Health Office
DTPK Special Program for Remote and low Resource Areas (Daerah Tertinggal,
Perbatasan, dan Kepulauan)
EDP Executive Development Program
EOPO End of Program Outcomes
Flotim Flores Timur (East Flores)
GFTAM Global Fund to Fight Tuberculosis, AIDS and Malaria
GIS Geographical Information Systems
GoA Government of Australia
GoI Government of Indonesia
HIV Human Immunodeficiency Virus
HPN Health Policy Network
HPU Health Policy Unit
HRH Human Resources for Health
HRMIS Human Resources Management Information System
HSR Health Sector Review
HSSCU Health System Strengthening Coordination Unit
HTA Health Technology Assessments
IPR Independent Progress Review
ISP Implementing Service Provider
IT Information Technology
IU Implementing Unit
Jamkesda Jaminan Kesehatan Daerah
JATIM East Java (Jawa Timur)
JKN National Health Insurance (Jaminan Kesehatan Nasional)
Kepmenkes Decree of the Health Minister (Keputusan Menteri Kesehatan)
KSI Knowledge Systems Initiative
M&E Monitoring and Evaluation
MEP M&E Plan
MNCH Maternal Neonatal Child Health
MoH Ministry of Health
MoHA Ministry of Home Affairs
MSS Minimum Service Standards
NIHRD National Institute for Health Research and Development
NCDs Non Communicable Diseases
NHA National Health Accounts
NSPK Norms Standards Procedures and Criteria (Norma, Standar, Prosedur, dan
Kriteria)
NTT East Nusa Tenggara (Nusa Tenggara Timur)
PBI Payment Premium for Poor
PERMATA Primary Health Care Strengthening and Maternal and Newborn Health
PF Performance Framework
PHA Provincial Health Account
PHC Primary Health Care
PJJ Distance Education Program (Pendidikan Jarak Jauh)
PMU Program Management Unit (PMU staff at province and district level)
Poskesdes Village Health Post (Pos Kesehatan Desa)
PPJK Centre for Health Financing and Insurance (Pusat Pembiayaan dan Jaminan
Kesehatan)
PPSDMK Centre for Human Resource Development in Health (Pusat Pengembangan
Sumber Daya Manusia Kesehatan)
PD Project Director
PS (AIPHSS) Program Secretary (Roren)
PSC Program Steering Committee
PTS Program Technical Specialist
Pusdatin Data Centre of MoH (Pusat Data dan Sistem Informasi)
Pusdiklat Centre for in Service Education and Training of Human Resources (Pusat Pendidikan dan Pelatihan)
Puskesmas Community Health Centre (Pusat Kesehatan Masyarakat)
PusRengun Centre for Workforce Planning (Pusat Perencanaan Dan Pendayagunaan)
Pustanser Centre for Standardisation, Certification of Human Resources (Pusat Standardisasi, Sertifikasi dan Pendidikan)
RA Reform Agenda
Renstra Strategic Plan (Rencana Strategis)
RJPMD Regional Mid Term Development Plans (Rencana Jangka Menengah
Pembangunan Daerah)
RJPMN National Mid Term Five Year Development Plan (Rencana Jangka Menengah
Pembangunan Nasional)
Roren Ministry of Health, Bureau of Planning and Budgeting (Biro Perencanaan dan
Peranggaraan)
SBD South West Sumba (Sumba Barat Daya)
SG Secretary General
SIKDA District Health Information System (Sistem Informasi Kesehatan Daerah)
SKN National Health System (Sistem Kesehatan Nasional)
SLO Senior Liaison Officer
SOP Standard Operating Procedures
SP2TP Strengthening Information System for Primary Care
TA Technical Assistance
TNP2K The National Team for The Acceleration of Poverty Reduction (Tim Nasional
ToR Terms of Reference
TTU North Central Timor (Timor Tengah Utara)
UHC Universal Health Coverage
UI University of Indonesia
UU Law or Act (Undang-Undang)
VFM Value for Money
Executive Summary
The Australia Indonesia Partnership for Health System Strengthening (AIPHSS) provides the Government of Indonesia (GoI) with a funding facility to address critical gaps in the health system at all levels of government. It addresses key reform issues including revitalisation of the primary health system; technical support for the national insurance scheme; strengthening health legislation under decentralisation of government; and the implementation of new minimum service standards. These make a significant contribution to improving access to better quality health care for poor and disadvantaged people in Indonesia. It is well recognised that investment in health outcomes contributes to thriving stable and economically productive communities.
AIPHSS has reached the point at which it is most relevant and demonstrating high levels of
sustainability for the majority of activities being implemented. The reforms being implemented align with national priorities and there is sustained and close interaction with senior policy makers in the Ministry of Health (MoH). The program has gained momentum and is delivering technical assistance that would otherwise be unavailable while providing models and tools for health system improvements at district and national levels and information to support evidence based decision making for policy development and allocative efficiency.
The partnership with the MoH remains strong, where AIPHSS continues to be a highly valued program. The most important factor which may affect this relationship is the impending budget cuts and the potential loss of impact on end of program outcomes due to the reduction in activities.
During this reporting period (January – June 2015) adequate progress has been made in a number of critical areas and the level of activity expenditure has increased compared to the previous six months. There have been a number of factors contributing to the improvement in overall performance and effectiveness. These include:
The development of the Health Systems Reform Agenda (RA), based on the Health Sector Review (HSR), the release of the new National Development Plan and the Ministry of Health’s Strategic Plan to guide investment priorities; and a clearer articulation of end of program outcomes to provide overall direction.
Significant ownership of interventions under AIPHSS by implementing partners and a greater level of participation in work plan development and implementation activities under the guidance of a Technical Director (TD) and Program Technical Specialist (PTS) and support from the Implementing Service Provider (ISP).
A reorganisation and consolidation of the ISP and Central Program Management Unit (CPMU) program delivery model to streamline management and operational processes. This has reduced transaction time and enabled the development of a more effective management system.
Strengthening the monitoring and evaluation system to improve accountability and tracking of activity progress and relevance to outcomes.
Despite improvement in overall performance and strategic direction, many activities are still falling behind planned schedules; in particular progress at the national level has been slow. This is especially the case for the Bureau of Budgeting and Planning (Roren)1 and Bappenas (Ministry of National Development Planning). This is in part due to implementing units underestimating the technical complexity of many activities and the time required to develop and agree terms of reference (ToRs). There is also varying availability of staff in implementing units (IUs) to lead implementation. At the sub national level, East Java (JATIM) is on track with implementation while East Nusa Tenggara (NTT) is behind schedule by several months due to a lack of response from the District Health Office (DHO) regarding taking responsibility for AIPHSS initiatives and revision of work plans.
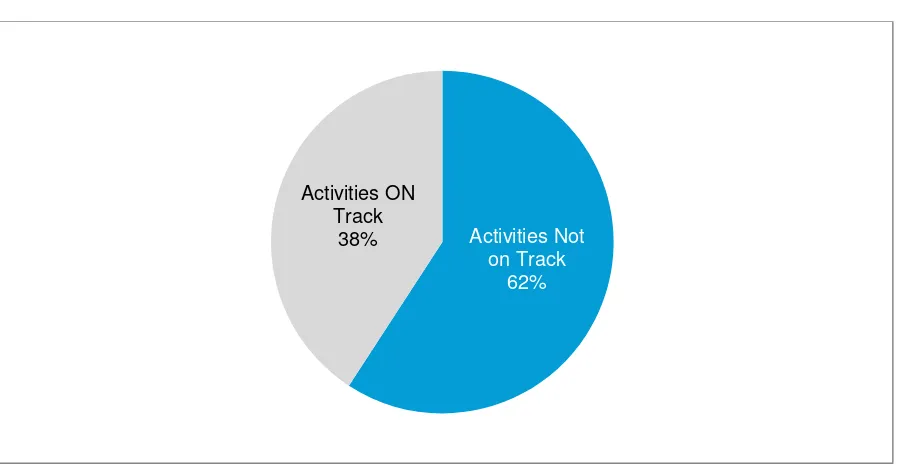
While only 36 per cent of the expected funding allocation has been spent for this period, over 62 per cent of activities are deemed to still be on track for completion as planned. The remaining 38 per cent are behind schedule, cancelled or have not commenced. Given the impending aid program budget cut
many of these activities will need to be re-assessed or postponed until other funding sources are available. 2
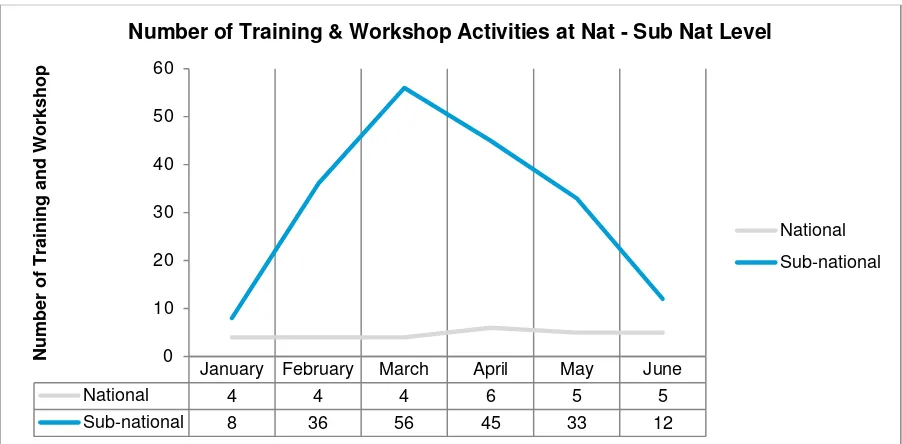
During the reporting period there have been over 8,000 (4016 males: 4345 females) participants engaged in training sessions and workshops. 3 The program has a significant reach across many different areas of the health sector and across different levels of government.
Progress and Achievements towards End of Program Outcomes (EOPOs)
General progress towards each of the EOPOs has been adequate, with the greatest progress being made towards achieving policies and procedures to improve the equitable allocation of health resources, followed by governance and supervision of the health system. These areas also have the highest level of program investment.
An Effective National Health Insurance Scheme
The Organisation of Social Insurance (BPJS) began operations in January 2014. Membership to the scheme has increased to nearly 140 million over this time (out of a population of 250 million) and demand is increasing. The scheme is designed to provide improved access to health care services and financial protection for individuals and families. However, by November 2014 the annual allocation was depleted and the fund required a government bailout. This is consistent with global experience.
To improve the effectiveness of the scheme, AIPHSS has been providing technical assistance and policy advice to BPJS with a focus on strategic purchasing including elements of cost containment and quality assurance. Further technical and financial support has been provided on National Health Accounts (NHA), Hospital Provider Payment System (INA-CBGs) and Health Technology Assessment (HTA) implementation for cost effective health care treatments. District Health Accounts (DHA) and Provincial Health Accounts (PHA) are also being produced to strengthen local financial planning and decision making.
Initial results indicate the scheme is on track to being more effective. The aim is to achieve improved quality and cost control, closer stakeholder collaboration to manage the hospital payment system and the institutionalisation of HTA in Indonesia.
Minimum Service Standards (MSS) to support Primary Health Care Delivery
New MSS were finalised during this reporting period. The delivery of MSS must be underpinned by legislation to ensure local governments allocate adequate resources to meet standards. This includes ensuring there are qualified staff, supervised correctly and provided with resources, guidelines and technical procedures.
During 2013-14 AIPHSS funded the revision of the MSS and health section of the decentralisation law. This revision is now encapsulated in Law-23/2014 which was enacted September 30th 2014. It is one of the most important achievements of the AIPHSS program which will have a major impact on the national service delivery system over time. The major activity in this reporting period was the preparation of the Norms, Standards, Procedures and Criteria (NSPK) which act as the implementing rules and regulations for the MSS.
The new law and MSS will impose a performance based planning and budgeting system for health programs at the district level. A model for this will be developed in the next reporting period. AIPHSS is now preparing a strategic approach to implementing the new legislation which places new functions and responsibilities on the DHO and Puskesmas. All of the AIPHSS districts are currently in the planning phase of providing technical assistance for restructuring to meet the new policies.
AIPHSS has also been instrumental in developing and supporting a Distance Education Program (PJJ) for midwives and nurses. This program is in its second semester with 87 students. So far the system has proven to be a cost effective way to facilitate training and there are already plans to scale
2 The overall aid program was cut by 40%. The actual reduction in budget for AIPHSS is currently under discussion.
3 Since the beginning of the program there have been over 26,000 participants involved in training and workshops comprising 13,049
up access with an estimated 116,000 nurses and midwives required to meet the new standards across Indonesia. The advantage is that students do not have to leave their place of work to undergo training and health services are not disrupted. As with most online education programs the main issues revolve around adequate bandwidth to ensure learning functionality, such as video
conferencing, and a requirement to be familiar with the technology or ensuring adequate technology support is available. A number of these constraints have been identified and actions taken to mitigate or minimise negative impacts (for example provision of hard copy materials up front). An evaluation of this training delivery mechanism was undertaken during this reporting period. The preliminary report
indicating that despite constraints, it is an effective method of delivering training and the ‘best solution’
to improving the qualifications of health personnel (particularly women) in Indonesia.
Accreditation of Local Health Service Centres
AIPHSS is providing technical assistance to develop an accreditation system for primary health services that has the potential to improve the quality of frontline services nationally. The objectives for Puskesmas accreditation are to achieve:
1. Formal recognition by government that the Puskesmas has the right competencies to serve a community to the required standard providing 155 medical and referral services
2. A credentialing system for the BPJS to contract Puskesmas as the first level health service
3. Self-evaluation to enable continuous improvement to meet customer needs.
AIPHSS has been providing technical assistance to develop the accreditation system since October 2014.
Overall the accreditation system has been implemented well. It is a high priority and a strategic investment by AIPHSS. It is expected that all activities related to the accreditation system will be completed in the next reporting period.
A future national roll out of the system will be a significant achievement attributable to the groundwork established by AIPHSS.
Equitable Allocation of Health Resources
AIPHSS has promoted evidence based policies and decision making to achieve a more equitable allocation of health resources. It has done this by supporting the Health Sector Review (HSR), completed in 2014, which identifies emerging health needs and gaps; revising legislation to clarify roles and responsibilities of health functions at all levels of government to ensure efficient use of resources; developing policies for human resource management for efficient allocation based on demand for services; and providing technical assistance to the national health insurance scheme which provides greater access to the poor. In addition, AIPHSS has provided technical assistance to support the efficient allocation of financial and human resources by supporting the development of district health accounts (DHAs) and workforce planning tools and guidelines.
All of these initiatives are considered sustainable because they are embedded in national and local policy processes and systems. There is a strong sense of ownership by partners. The uptake of policies and targets from the HSR indicate that AIPHSS has been able to help shape national health policy.
The HSR was developed using a government led process with technical assistance provided by a range of international and national experts who were closely engaged in the government policy process. This led to a higher level of uptake of the HSR recommendations and targets in the governments five year mid-term development plan (RJPMN) and the MoH Strategic Plan. AIPHSS has been providing technical assistance to also promulgate these policies and strategies to regional and local level strategic plans to influence the allocation of health resources at the local level, and ensure a focus on public health and prevention.
To further strengthen evidence-based policy development, a Health Policy Unit (HPU) was established on April 1 in the MoH during this reporting period. The intention is to provide senior advisers with current information on emerging health policy priorities and to channel research
provincial-level stewardship guidelines for North Sulawesi; a policy brief on stunting; and guidelines for integrated Monitoring and Evaluation (M&E) for Roren.
Building a human resource information system at the national level is a major ongoing activity. This is complemented by technical assistance to develop needs-based workforce planning approaches. In addition AIPHSS has assisted in formalising the tools to ensure all Human Resources (HR) planners have approved guidelines in planning HR requirements in health facilities. Together these initiatives will lead to a more efficient and effective approach to the allocation of human resources for health as well as strengthened capacity. These initiatives have commenced during this reporting period and are on target for completion in 2016.
A revision of health data collected by Puskesmas (SP2TP) has been an ongoing activity. The current extensive data collection requirements are creating a significant burden with limited utility. The purpose is to streamline collection so that data can be better used for planning and decision making, particularly in the allocation of health resources. The activity is going through a technical review due to problems with the technical team not conducting adequate coordination with the district levels. This process should be completed in the next reporting period.
Governance and Supervision of the Health System
A wide range of AIPHSS interventions contribute to improving the governance and supervision of the health system. In this reporting period the focus has been on the implementation of an Executive Development Program (EDP) for strategic management of human resources. Forty senior staff from MoH have participated in the first part of the program and another 40 are being trained in workforce planning techniques and tools.
At the local level, the focus has been on getting technical assistance to support restructuring and organisational development to meet the new legislative requirements and roles and responsibilities under MSS implementation. This initiative is currently underway but once completed will provide a new organisational model that can be potentially be used in other provinces and districts.
Communication and coordination within the MoH and across levels of government is a key strength of the program and is an ongoing process, which is contributing to good governance. Specific initiatives
undertaken during this reporting period include: conducting quarterly technical coordination meetings; holding policy dialogues or discussion forums on key policy issues; implementing the Health Policy Unit (HPU); and implementing the Health Systems Strengthening Coordination Unit (HSSCU). All of the initiatives have the support of the Secretary General and will be important in transitioning program interventions to counterpart operations towards the end of AIPHSS. The HSSCU was established at the request of the Secretary General to coordinate all donor funded activities. This Unit could be instrumental in helping AIPHSS initiatives gain ongoing support from other donors towards program completion.
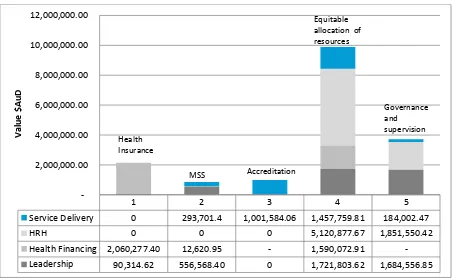
Distribution of Investment
Challenges and Emerging Risks
Without sustained investments in some key areas the program is in jeopardy of not achieving all desired outcomes. This impact can be mitigated through the development of an AIPHSS exit strategy that focuses on transitioning key activities to other funding sources and prioritising those that will provide the most benefits to stakeholders.
The proposed 40 per cent budget cut4 during the last phase of the program will have a significant impact on many parts of the program that have begun to gain ownership and momentum. The key risks and challenges are:
Cutting existing programs risks losing the full investment in the activity: Many activities are only partially completed and may not be sustainable if cut prematurely. Careful consideration will need to be given to how activities will be transitioned.
Expectations will need to be managed. During the first quarter of 2015 IUs were strongly encouraged to progress rapidly with their work plans in order to disburse funds. The potential budget cuts will now mean many activities will need to be scaled back rapidly.
Developing an Exit Strategy: Each activity will need to be examined in terms of strategic importance, level of investment, time to completion and funding required for ensuring sustainable outcomes. The exit strategy will need to identify how existing investment can be preserved and what can be transitioned to other government programs.
The other significant challenges will be staff retention and knowledge management. As the program nears completion, there is a likelihood that staff will seek other opportunities. Knowledge management therefore becomes critical during this period. A knowledge management strategy has been developed and it will be critical that it is implemented successfully in the next 12 months to ensure ongoing initiatives developed by AIPHSS can be continued by partners and the program is used as a foundation for future health system strengthening.
4 This is the overall budget cut to the aid program. The specific budget cut to AIPHSS is currently under negotiation.
1 2 3 4 5
Service Delivery 0 293,701.4 1,001,584.06 1,457,759.81 184,002.47
HRH 0 0 0 5,120,877.67 1,851,550.42
Health Financing 2,060,277.40 12,620.95 - 1,590,072.91
-Leadership 90,314.62 556,568.40 0 1,721,803.62 1,684,556.85
2,000,000.00 4,000,000.00 6,000,000.00 8,000,000.00 10,000,000.00 12,000,000.00
V
a
lu
e
$
Au
D
Health Insurance
MSS Accreditation
Equitable allocation of resources
Evaluative Summary
Relevance: The AIPHSS is at its most relevant phase. The Reform Agenda has ensured that the program is aligned with the Ministry of Health’s strategy and highly relevant in addressing the underperformance and equity problems related to health systems development. The program is valued by partners as a mechanism which provides national and international technical assistance and financial resources which is difficult for them to access at short notice. The program is also
strongly aligned with DFAT’s Health for Development Strategy (2015-2020) with investment in xxx ? strengthened, resilient public health systems being the highest priority.
Effectiveness: The AIPHSS program is now mainly focused on national level policy development and systems change, guided by the new Reform Agenda but also includes testing and piloting policy implementation at the sub national level. The success of the HSR, changes to the decentralisation laws and MSS demonstrate effectiveness of the program at a policy and sectoral reform level. This has the potential to influence organisational changes of district health offices and the quality of health care at a much broader scale than just AIPHSS provinces. With the addition of the TD and changes to the management structure, the program has a more effective delivery system. Access to senior management has improved, which facilitates more effective uptake and ownership. Interventions are now aligned with end of program outcomes so their effectiveness in contributing to end of program outcomes can be evaluated for priority setting.
Efficiency: A clearer and more efficient management model is now in place with increased activity over the current reporting period. There is now a more efficient flow of information and decision making with one management and operations unit. The rate of implementation and disbursement was slow in the first half of this reporting period, nevertheless by June 2015 almost 62% of the work plan activities have commenced to the planning and or implementation stage; 36% of overall funds have been disbursed against planned expenditure. However, activity expenditure by IUs is still low at just over 10% of budget indicating either inefficient government systems or poor planning and internal resourcing.
Monitoring and Evaluation: The monitoring and evaluation system continues to respond to changes in the program and is now aligned with new EOPOs. The M&E Plan was updated and three
independent evaluations have been completed with another eight planned. The M&E system has restructured around the new program logic model and monitors progress against EOPOs as well as health system building blocks.
Sustainability: The AIPHSS is embedded in the national systems, where all key decisions about activities are made by partners. Outputs and outcomes have a higher probability of being sustained. The majority of AIPHSS activities are part of larger GoI policy development and program
implementation. The program provides resources which accelerates implementation of GoI initiatives and targets system bottlenecks.
Gender equality: An internal review of gender and social inclusioncommenced during this reporting period. The report will highlight any key areas of focus for the remainder of the program. . Based on available sex disaggregated data collected during meetings, workshops and training for the reporting period, there is a high level of participation of both sexes across all intervention areas.
Risk Management and Safeguards: Risks are carefully monitored and managed as part of the programs management. The risk register is updated monthly and distributed to partners. Any critical areas are escalated immediately when they become apparent. The most significant risk at this juncture is the cut to budgets at a point when the program has gained significant momentum.
1
Introduction
This report is the fifth Six Monthly Report for the Australian Indonesia Partnership for Health System Strengthening (AIPHSS). It covers the period from the beginning of January 2015 until the end of June 2015.
The structure of reporting has changed during this period to provide a focus on End of Program Outcomes (EOPOs)5 and contributing intermediate outcomes. A revised program logic model was developed by key stakeholders in February 2015 and five revised end-of-program outcomes were agreed with the Department of Foreign Affairs and Trade (DFAT) Health team. This led to a revision of the interim Monitoring and Evaluation Plan (April, 2015) and changes to the performance
framework. The program reporting now reports progress against these revised end-of-program outcomes which is discussed in Section 3.
This period also reflects the implementation of the new “Reform Agenda for Health System Strengthening” finalised during the last reporting period and emanating from the Independent
Progress Review (IPR) conducted in the first quarter of 2014. This process adopts a systemic
approach to health systems reform focussing on four components or “health system building blocks”:
(1) Leadership and Governance; (2) Health Financing; (3) Human Resources for Health; and (4) Service Delivery. Work plans implemented by Implementing Units (IUs) for this period use this building block structure for reporting on activities and outputs.
Given these recent changes, the introduction section of this report provides an updated summary on the background to AIPHSS, the Reform Agenda (RA), and the current Program Framework. This illustrates how the implementation framework, which is based on the Reform Agenda and health system building blocks, is used to deliver the end-of-program outcomes in support of the broader program goals (see program conceptual framework p.6 below).
Section 2 provides a more detailed analysis of the relevance of the program in relation to the current Australian government aid policy. It explores the political economy, key contextual factors and the expected benefits of the investment.
Section 3 provides a summary of progress towards end-of-program outcomes. This is a synthesis of
the program’s contribution to each of the outcomes through an analysis of major activities and outputs facilitated by AIPHSS.
Section 4 describes current implementation processes, challenges and emerging risks, as well as progress against the Annual Implementation Plan including planned versus actual expenditure.
Section 5 provides an evaluative summary of the program against the Aid Quality Criteria, including cross cutting issues such as gender and social inclusion.
Section 6 outlines priorities for the next period and recommended improvements to program implementation.
1.1 Background to AIPHSS
AIPHSS commenced in December 2012 and is jointly undertaken by the Governments of Indonesia (GoI) and Australia (GoA) to support the development and implementation of health sector reforms and health systems strengthening.
The ultimate goal of the program is “to improve the health status of poor and disadvantaged people of
Indonesia”. The program focuses on improving access to better quality health care services, including
public health. It does this by reducing financial barriers to accessing quality health care and
strengthening governance and systems that facilitate improved local health service delivery. Across the health system it focuses on four areas: (1) governance, with a specific focus on improving health
policy, influencing behavioural change through the development and implementation of regulation, and the use of information for evidence based decisions; (2) financing and equitable access and distribution of resources; (3) improving the skills and distribution of the health workforce; and (4) providing quality health service delivery to obligatory minimum standards.
AIPHSS approach to health system strengthening. is guided by the GoI Ministry of Health (MoH)) which has identified interventions that are designed to strengthen institutional, organisational and individual performance, and address bottlenecks in health policy , system weaknesses in human resources, health financing , governance and health service delivery. Interventions are selected from an analysis of health system gaps which have been identified in the Reform Agenda and the Health Sector Review (HSR). This approach involves multiple stakeholders, including, ministries, departments and professionals to identify gaps and to reach agreement on interventions and priorities.
AIPHSS has adopted a flexible and adaptive management approach. Some AIPHSS interventions are modified to adapt to changing circumstances or to the local provincial and district environment. Interventions are also added at any time to the program when perceived gaps or needs are identified by partners. This responsive approach provides the MoH with rapid access to technical and financial resources during shifts in policy which planning and budgeting GoI systems do not permit. This approach is a key factor in strengthening the partnership between the Government of Australia and the Government of Indonesia.
The Implementing Service Provider (ISP), Coffey International Development (Coffey), sources technical expertise for the MoH and provides management support for the implementation of partner selected interventions. These technical experts work in partnership with the MoH to identify and respond to key health policy and systems gaps. Interventions are selected by partners based on partner experience of the health system weaknesses and the changes required alongside available evidence. These technical experts also assist with the development of evidence, advocacy and implementation of policy and strategic plans.
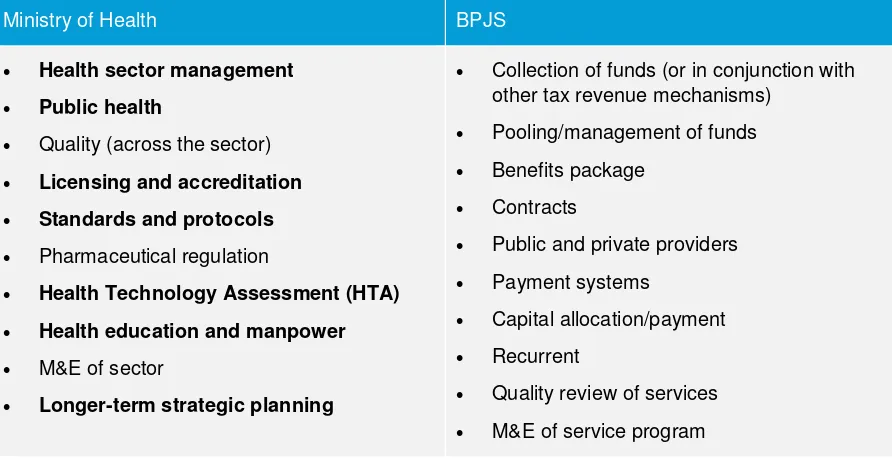
The main MoH Departments supported by AIPHSS include:
1. Bureau of Planning and Budgeting (Roren) for governance;
2. The Pusat Pembiyaan dan Jaminan Kesehatan (PPJK) for health financing;
3. The Centre for Human Resource Development (PPSDMK);
4. MoH Directorate for Development Standards (BUKD); and
5. Bureau of Law and Organisation
AIPHSS is also supporting activities implemented through the Ministry of Planning and Development’s (BAPPENAS) Health and Nutrition Department.
The program also collaborates with the other DFAT funded program such as the, Australian Indonesian Partnership for Maternal Neonatal and Child Health (AIPMNH), the Knowledge Sector Initiative (KSI) and the health team from the Poverty Reduction and Social Protection Program (TNP2K) as well as the Governance Reform Partnership (Reform the Reformers).
AIPHSS works with eight district level governments in two provinces which have a high poverty incidence as well areas that have been socially excluded due to ethnicity. These are: Situbondo, Bondowoso, Sampang and Bangkalan in East Java Province; and Timor Tengah Utara (TTU), Flores Timur (Flotim), Ngada and Sumba Barat Daya (SBD) in East Nusa Tenggara Province (NTT).
AIPHSS is scheduled to end on 30 June 2016.
1.2 The AIPHSS Reform Agenda for Health System Strengthening
The Reform Agenda acts as a guiding framework for the MoH partners in the selection and
Key policy directions from the National Five Year Mid Term Development Plan (RJPMN)
Analysis conducted as part of the Health Sector Review (HSR)
Decentralisation legislation for health functions
Minimum Service Standards (MSS) for primary health care.
The implementation of the Reform Agenda through the AIPHSS program aims to strengthen the health system at the national and subnational levels while contributing to the implementation of RPJMN and the new five year MoH National Health Strategic Plan (RENSTRA).
The Reform Agenda identified the following weakness in health policy related to the four AIPHSS focus areas:
Governance and Decentralisation
Decentralisation laws and regulations between the different tiers of government (central, provincial and district) require revision for the following reasons:
The current functional distribution is not consistent with the health system functions as stated in the Perpres-72/2012 on the National Health System (SKN);
The functions do not meet the needs of all population segments;
The Minimum Services Standard, as listed in the Minister of Health Decree-741, does not provide comprehensively cover for essential health needs of communities;
In many districts the recruitment of the District Health Officer by the local government (Bupati/Walikota) is not competency or merit based.
Human Resources
The human resource policy direction provided RPJMN 2015–2019 and the MoH Strategic Plan 2015–
2019 is “improving the availability, distribution and quality of human resources for health”. The
rationale for seeling significant improvement in this area is based on the following:
There is no strategic plan on the number, competencies and production of health workers, the quality and production of the health workforce is not in aligned with the changing demand for services.
There is no strategy on how to produce “primary health care physicians” as stated in the Law on Medical Education (UU Pendidikan Kedokteran (Medical Education)).
Mal-distribution of the health workforce, and insufficient availability, quality and low productivity of public health workers.
Lack of accessible and up-to-date information on human resources for health.
The quality of graduates in many cases does not meet the standard criteria, especially for midwives, and there is a general mismatch in the recruitment and placement of health workers.
There is no career development pattern for the health workforce. Health Financing
The Health Sector Review identified a range of important policy and systems challenges in health financing which informed the RA. These include amongst others a severe underfunding of public health services, which in the long term will have a negative impact on the National Health Insurance Scheme (JKN) financial burden by not addressing prevention and promotion services to address risk behaviour. In addition, there is a need to find innovative and alternative sources of health financing to ensure public health programs are funded.
The RA highlighted other areas that need addressing:
JKN membership to include non-PBI6 participants, especially workers in the informal sector
Guidelines for a benefit package/clinical pathway and procedures of use
Cost sharing by participants at service points
Development of cost control and quality control systems
Efficiency and effectiveness of payment of health services provider (provider payment).
Defining the basic package of public health and clinical services and ensuring it is costed
Strengthening planning and performance-based budgeting
Strengthening MoH capacity in health financing policy analysis. Primary Health Care
The RA follows the GoI definition of the main task of a Puskesmas which is "improving area
wide/sub-district health status" through: (1) promoting community participation and empowerment; (2) implementing public health programs; (3) providing individual clinical health care services; and (4) encouraging health oriented development (healthy public policy). Since 1 January 2014, the
Puskesmas has a new function as the primary health care provider for the national health insurance members and now must be equipped to respond to the treatment of 150 different categories of health conditions which focus the Puskesmas on curative care. This requires Puskesmas reforms related to human resources, management, equipment, financing, information systems, accreditation, referral and reporting systems. These all need to be tested at the district level requiring collaboration between government at the provincial and national levels.
1.3 Program Framework
A revised program logic model was developed with key stakeholders in February 2015. This was based on lessons learnt through implementing the original program design. It now ensures priorities of the partners are aligned towards a common goal and agreed end-of-program outcomes (EOPOs). This guides investments of AIPHSS taking into account synergies with future donor funded programs such as the Primary Health Care Strengthening and Maternal and Newborn Health Program
(PERMATA).
The goal of AIPHSS is to contribute to “improving the health status of poor and disadvantaged people
in Indonesia”. The focus is on improving access to better quality health care by removing financial barriers to accessing health care services; and by improving local health service delivery including providing effective public health care and promotion.
There are five EOPOs that AIPHSS is expected to make a contribution toward in support of the broader goal:
1. Effective national health insurance policy, rules and regulations implemented
2. Minimum service standards (MSS) are adhered to at all levels of health service delivery
3. Local health service centres achieve accreditation
4. Health resources equitably allocated at all levels of government
5. Good governance and supervision practiced at all levels of government
The implementation framework is based on the four health system building blocks outlined in the Reform Agenda. These are functional areas that guide investment aligned to Implementing Unit (IU) work plans at the national and sub-national levels. These health system building blocks are:
1. Governance and Leadership, including health sector decentralisation
2. Health Financing
3. Human Resources for Health
4. Service Delivery
The program framework ensures that the interventions funded by AIPHSS under the RA contribute to achieving the end-of-program outcomes (EOPOs). Each intervention is mapped against its
guidelines, standards and regulations etc.) and how each of these are implemented by the GoI to achieve intermediate outcomes such as the extent to which:
An adequate, capable and supervised workforce is in place
Health legislation is enacted to implement the minimum service standards
Polices and decision making are based on evidence and accurate information
Good governance is practiced at all levels of government supported by improved communication and coordination
Strategic planning is improved and there is an improved ability to identify health system needs based on evidence
A key indicator of future success will be the percentage of AIPHSS activities that are funded in the national and regional budgets (2016-2017) for roll out at the national and regional levels. The source of data for this indicator will be from national and regional budgets. For many activities this may not be measurable until 2017 due to budgetary planning cycles, however, the next 6 monthly progress report and end of program report will use this as an indicator of sustainability and impact.
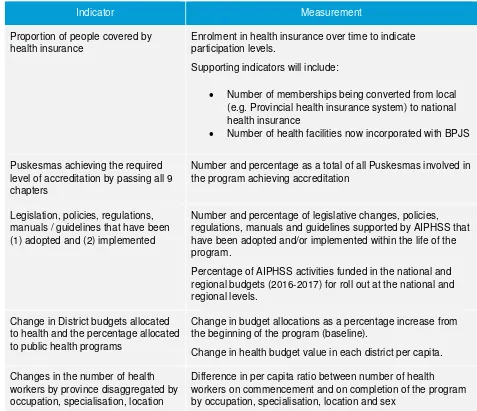
Other headline indicators (key performance indicators or aggregated development results (ADRs)) to be reported in the next report period and at the end of the program are given in Table 1 (as outlined in the revised M&E Plan, June 2015).
[image:17.595.62.539.368.779.2]The overall conceptual framework is illustrated in Figure 1.
Table 1. Key Performance Indicators
Indicator Measurement
Proportion of people covered by health insurance
Enrolment in health insurance over time to indicate participation levels.
Supporting indicators will include:
Number of memberships being converted from local (e.g. Provincial health insurance system) to national health insurance
Number of health facilities now incorporated with BPJS
Puskesmas achieving the required level of accreditation by passing all 9 chapters
Number and percentage as a total of all Puskesmas involved in the program achieving accreditation
Legislation, policies, regulations, manuals / guidelines that have been (1) adopted and (2) implemented
Number and percentage of legislative changes, policies, regulations, manuals and guidelines supported by AIPHSS that have been adopted and/or implemented within the life of the program.
Percentage of AIPHSS activities funded in the national and regional budgets (2016-2017) for roll out at the national and regional levels.
Change in District budgets allocated to health and the percentage allocated to public health programs
Change in budget allocations as a percentage increase from the beginning of the program (baseline).
Change in health budget value in each district per capita.
Changes in the number of health workers by province disaggregated by occupation, specialisation, location
Indicator Measurement
and sex
Technical assistance delivered as planned by building block and contribution to end of program outcome and level of result achieved
Number and dollar value of TA delivered as planned and per cent achieving intended results by building block and end of program outcome.
TA scored as less than satisfactory (limited results achieved); satisfactory (meets most requirements); highly satisfactory (meets all requirements, exceeding some)
Number of Training
programs/workshops and participants (sex disaggregated) by building block and implementing units – totalled every six months
Total male/female participants totalled every 6 months attending workshops, meetings and training sessions
Figure 1 Conceptual Program Framework
Improved health status of poor and disadvantaged people
in Indonesia
More people have improved access to better
quality health care and benefit from effective
public health and promotion services
Local health service deliver inclusive of public health is
improved (AIPHSS/PERMATA) Financial barriers to
accessing health services are removed for the
poor Broader Goals End of Program Outcomes Immediate Outcomes Minimum service standards are adhered to at all
levels of health service delivery
Health resources equitably allocated at
all levels of government
Good governance and supervision practiced at all levels
of government
Enabling Outcomes
Adequate, capable, well supervised and monitored workforce
in place
Health legislation to enforce minimum service standards is
enacted
Evidence based policies promote equitable allocations
Improved quality of strategic planning
Improved ability to identify health system
needs
Improved communication and
coordination
Service Delivery
Puskesmas Primary Health Care
Governance and Leadership
Decentralisation Policy and Planning
Human Resources for Health
Strategy and Policy Information Systems Health Financing National Insurance Health Accounts Effective monitoring evaluation and learning systems implemented in all levels of government
Implementing the Reform Agenda
Outputs and Activities of Implementing Units
(National and Sub national)
Health System Building Blocks
Appropriate, relevant and accurate information
provided in a timely manner Evidence based decision making between key stakeholders Effective national health insurance policy, rules and
regulations implemented
Local health service centres achieve
accreditation
Box 1. Economic Growth and Health Outcomes
The recent UK Lancet Commission on Investing in Health (Jamison, et al., 2013) estimates that:
Up to 24% of economic
growth in low- and middle-income countries was due to better health outcomes.
Increasing life expectancy by one year can increase gross domestic product (GDP) by 4 per cent.
Reductions in mortality account for about 11 per cent of recent economic growth in low-income and middle-income countries.
Investing in health yields a 9 to 20-fold return on
investment.
2
Relevance of AIPHSS
It is recognised that investment in health outcomes contributes to thriving stable and economically productive communities. For example increasing life expectancy by one year can increase gross domestic product (GDP) by 4 per cent. Reductions in mortality account for about 11 per cent of recent economic growth in low-income and middle-income countries as measured in their national income accounts7. Australia’s investment in health will contribute to building economically productive
communities in Indonesia. This leads to growing markets and trade within the region where Indonesia is a key market and trading partner. Indonesia is approaching a middle class of 100 million by 2020.
The World Health Report (2000) demonstrated the importance of investing in health systems strengthening as an essential aspect of improving health
outcomes for communities. Without sustained investments in health systems strengthening the investments in vertical programs such as MNCH; Malaria, Tuberculosis and HIV cannot be sustained if the backbone of the health system is not strengthened and maintained.
AIPHSS has reached a point where it is at its most relevant. This is evidenced by the alignment through the Reform Agenda with national policy priorities and a close interaction with senior policy making levels in the MoH which ensures the program has the potential to influence policy and adapt to policy change. The focus on revitalisation of primary health care models, technical support for the national insurance scheme, changes to health legislation under decentralisation, and the implementation of a new minimum services standards are key reform issues for the government partners placing the AIPHSS at the centre of the health policy environment.
The program is also strongly aligned with DFAT’s new Health for Development Strategy (2015-2020) with
investment in strengthened, resilient public health systems being the highest priority. The AIPHSS program achieves this through providing the GoI with access to flexible small scale funding which can be used for innovation and catalytic activities which GoI systems cannot deliver quickly. The
program is also valued for delivering rapid technical assistance and the provision of information and evidence to inform the implementation of priority areas.
Currently the AIPHSS program is leading the way in how other development partners now want to address health systems strengthening to improve delivery of essential services. This is evidenced by the senior staff from the USAID and the Global Fund for AIDS, TB and Malaria regularly consulting AIPHSS senior management on how to invest in and implement health systems strengthening at the national level.
2.1 Contextual Analysis
A number of recent changes at the political and partnership level have occurred which affects the future of the AIPHSS program.
The most important development is the 40 per cent budget cut to the Australian Aid budget in Indonesia8. At this stage it is uncertain which health programs will be affected but it is clear there will be a substantial reduction in resources. This creates high levels of uncertainty amongst the partners and AIPHSS staff about the future of the program. AIPHSS senior managers have commenced the preparation for an exit strategy.
There has been only one major announcement in the health policy environment. The newly appointed Minister of Health has announced a policy priority titled
“Nusantara Sehat” which is a healthy Indonesia
initiative. There are no major implications for the AIPHSS program as it is already supporting health systems strengthening at a national level as well as having a provincial focus in NTT and East Java.
A number of AIPHSS activities are high on the policy agenda for the MoH. These are capacity building for the provider payment system for the national health insurance scheme; the accreditation of the primary health care centres; the next stages of implementing the Minimum Service Standards including costing.
The program has also commenced the implementation of the policy dialogue series led by the Technical Director (TD) and the Secretary General of the MoH. The first of these took place in May 2015 focusing on Pharmaceutical Policy in the era of JKN. The initial feedback from participants and MoH is that this was a successful event which has led to cross sectoral follow up on specific recommendations on pharmaceutical policy. Consequently there is now a further demand for policy dialogue from the MoH in areas such as
strengthening the roles and functions of Puskesmas; improving the quality and distribution of health workers; and synchronising MoH regulations.
The partnership remains strong with the MoH and AIPHSS continues to be a highly valued program. The most important factor which may affect this relationship is the differing priorities between the Australian and Indonesian governments in terms of health sector investment. A message emerging
from the Secretary General’s office is that if the health programs are to be cut then there is a preference for the continuation of AIPHSS over introducing new initiatives.
Another emerging factor which may affect the partnership is the extension of the program to 2017. The current subsidiary agreement has been amended to extend the AIPHSS program to 2017, however, if budget cuts result in AIPHSS ending in June 2016 there is the potential that the
partnership will be negatively affected with a possible impact on the acceptance of the PERMATA and Papua programs. This will require careful management in the next reporting period.
8 This is the overall budget cut to the aid program. The specific budget cut to AIPHSS is currently under negotiation.
Box 2. A Growing Market: Changing Demand
Indonesia is a rapidly growing market for health services. Demand for health care is expected to rise significantly in the next few years due to a combination of factors:
A population growing at a rate of 5 million per year. The middle class is estimated to reach 100 million by 2020.
An ageing population: The majority of the population growth is expected in the over 45 age group. By 2025, the elderly population will almost double to 23 million
The changing burden of disease. Non-communicable chronic
diseases are rising significantly and, unless detected early, are
expensive to treat.
New and expensive treatments becoming available and a growing middle class with higher
expectations.
3
Progress towards End of Program Outcomes
(EOPOs)
General progress against each of the new EOPOs is adequate. The greatest progress is being made in achieving the equitable allocation of resources, followed by governance and supervision. This is associated to the higher level of activity investment being allocated to these EOPOs.
All activities under accreditation will be completed in the next reporting period and will mean that a high level of progress against this EOPO will be accomplished. All other EOPOs require sustained implementation and investment in order to be successfully accomplished.
Progress at the national level is slow and behind schedule for the majority of activities. This is especially the case for the Bureau of Budgeting and Planning (Roren)9 and Bappenas. This is due to the technical complexity of many activities and time taken to develop and agree terms of reference (ToRs) and the varying availability of IU staff to lead implementation. At the sub national level East Java is on track with implementation while NTT is behind schedule by several months due to a complete revision of the work plans following inputs from the PTS in the second quarter of this reporting period. These delays may inevitably result in the roll-over of activities to 2016, however, in order to accelerate technical aspects, the ISP is facilitating regular meetings on TA coordination to ensure local staff manage AIPHSS activities and local budgets are allocated to meet future requirements.
3.1 An Effective National Health Insurance System
Progress under this EOPO is measured against the intermediate outcomes and effectiveness of the technical assistance provided to the government counterparts by an international health financing expert; the contribution of the PTS to a BPJS expert group on quality control and health financing; the institutionalisation of Health Technology Assessments (HTA); and the strengthening of the hospital provider payment systems based on Case Based Groups (CBGs).
In January 2014, the new Agency for the Organisation of Social Insurance (BPJS) began operations. Membership to the scheme has increased by 114 million people to nearly 140 million out of a population of over 250 million and the demand for coverage is increasing. Overall global experience shows that an increase in coverage for health care leads to better health outcomes10 by providing; improved access to care and medicines; higher quality of services; and improved financial protection for individuals and families.
A primary objective of the scheme was to ensure claims for care services were reimbursed within 15 days which was successful, however, by November 2014 its annual allocation had depleted and the fund was out of money requiring a bailout by the new government. Nevertheless the experience of year one is consistent with global experience. In discussions with the AIPHSS senior management, it
was agreed that the BPJS must focus more closely on “strategic purchasing” that includes elements
of cost containment and quality assurance.
An international financing expert commenced in February 2015 and four policy notes have been produced during the reporting period (see Annex 3 for a full list of policy notes and their contributions to achieving EOPOs). AIPHSS has provided advice to BPJS on their policies such as: 1) increasing the premium for the poor; 2) tools for cost containment, and 3) improving quality by using the Health Insurance Fund. In addition a health financing policy research and assessment agenda has been
developed in collaboration with the Vice President’s office (TNP2K team). Technical and financial support has also been provided on National Health Accounts (NHA), Hospital Provider Payment System (INA-CBGs) and Health Technology Assessment (HTA) implementation. District Health
9 In Roren no staff were available to work on AIPHSS and two short term technical staff were recruited to specifically manage AIPHSS activities, this places Roren six months behind schedule for most of their work plan
Accounts (DHA) and Provincial Health Accounts (PHA) are also being produced to strengthen local financial planning and decision making.
The monitoring and evaluation of the national health insurance scheme by implementing partners in NTT and JATIM has not yet started.
Technical Support for Cost Containment and Quality Control
BPJS has created a strategic purchasing expert group, and appointed the Program Technical Specialist (PTS) of the AIPHSS program as the chairperson. This has resulted in weekly meetings taking place and the BPJS is identifying new opportunities and investments in policy across several areas:
Improved primary care
An improved referral system to higher levels of care, with indicators and tracking mechanisms
Reduction in unnecessary hospital admissions and instead provision of services in more cost-effective settings such as outpatient care
Improved quality during hospital admissions
More appropriate and timely discharges from hospitals and fewer re-admissions
Improved pharmaceutical policy for more appropriate use of drugs11.
Strengthening Provider Payment Systems
Australia is a global leader in new ways to pay providers (physicians and hospitals) that encourage improved quality and efficiency in the delivery of services. The program brought in an Australian global expert, Dr Ric Marshall, to discuss these new systems. Seminars involving over 50
stakeholders from BPJS, MoH, Ministry of Finance, and other agencies were conducted during this reporting period. The technical inputs generated intense interest because of challenges now facing BPJS the JKN scheme. There was a groundswell of demand for capacity building to enable Indonesia to develop and model their new systems under BPJS in a way similar to Australia. The next steps will involve prioritising the most useful training requirements emanating from the seminars in line with budget expectations. The Secretary General has appointed 10 people as a team to work with Ric Marshall. The training required will most likely focus on costing development support and team capacity building in areas such as case grouping (CBG specification and design), tariff setting (pricing) and claims management.
Developing Health Technology Assessment (HTA) for evidence based decision making and policy
Systems for HTA improve standards, quality of care, and appropriateness of care. The development of evidence through HTA will be increasingly used by the BPJS for decision making on cost effective health care treatments. This is an essential system’s development component which in the long term will affect cost containment as the demand for sophisticated medical technologies increases and evidence based decisions are required for rationing health care. HTA will improve transparency, and create a more level playing field for international firms in medical equipment and pharmaceutical products.
In this reporting period AIPHSS has supported the development of technical guidelines for the National HTA Committee. In addition a number of high level workshops and seminars were held with the Government and the BPJS insurance fund to discuss HTA studies. Two policy notes were drafted on a policy framework for HTA and global best practices and disseminated to almost 300
stakeholders and key policymakers in Indonesia. In addition the AIPHSS program has worked closely with the MoH to establish the HTA secretariat which is now a core unit for coordinating all HTA activities. AIPHSS is also providing technical assistance to the government to develop an HTA “Road
Map” to build capacity and help policymakers build policies and develop effective institutions in the
next few years. Three people have been recruited to develop institutional guidelines, economic evaluations and technical reviews. Although this development is in its infancy, the impact of HTA in the long term will be a more cost effective health system.
3.1.1 Summary
The primary inputs to achieve this EOPO are technical advice from an international health financing expert; an international training program to improve the hospital payment system which is based on Case Based Groups (CBG) (both of these are high cost activities); and policy advice from the PTS. The effectiveness of the international expert has been limited due to the poor engagement with the BPJS which has not been open to receiving international expert advice. A number of meetings took place between DFAT and BPJS in this reporting period to negotiate this but it did not result in any further engagement. On the other hand the PTS is accepted as a lead adviser on the key expert group, bringing into question the value of a full time expert. The training program for the hospital provider payment system CBGs is likely to have a larger impact on the management of the hospital payment system and cost control once the training is implemented in the next reporting period. The scoping mission conducted in April received a strong interest from many stakeholders across government, the hospital sector and BPJS. There is clear high demand for this type of knowledge.
The results or changes from the activities being implemented require more time; however, emergent results are improved advisory for quality and cost control; closer stakeholder collaboration to manage the hospital payment system; an emerging collaboration; and the early stages of institutionalisation of HTA in Indonesia.
Adequacy of Inputs: The input of the international expert has been limited by poor access to BPJS. Measuring the uptake of advice is difficult at this early stage.
Progress: Adequate overall. Policy advice and uptake does not work according to clear schedules but technical and policy advice has been provided, and policy notes have been produced and disseminated.
Sustainability: Difficult to assess the sustainability of international TA, but advice has been taken up by some government authorities and the advice from the PTS has a higher probability of
sustainability. This is evidenced through the policies adopted and decisions made under his guidance. HTA activities are highly sustainable as they will be included in national budget plans.
Next Steps: Implementation of the training program for hospital provider payment; continuation of HTA activities; PTS to continue to provide guidance and the HTA activities are ongoing.
Gender Social Inclusion and Disabilities: The main emphasis of the intervention is on providing improved access to affordable and adequate health care for disadvantaged groups.
3.2 Minimum Service Standards (MSS) to support Primary Health
Care Delivery
The delivery of the MSS must be underpinned by legislation which legally binds local governments to allocate adequate health resources to meet the standards. This includes the right type of staff supervised correctly with adequate resources and competencies to deliver the MSS. These staff will need to be provided with the technical guidelines and procedures that outline how the standards are to be delivered. These steps are articulated and measured in the intermediate outcomes below and provide a pathway to measuring progress towards the EOPO.
Intermediate Outcome: Adequate, Capable and Supervised staff in Place
The Distance Education Program (PJJ) is a response to national policy to improve equitable access to better quality human resources for health. The program is especially designed for nurses and
midwives to meet the minimum qualification of Diploma III. This system allows nurses and midwives to be trained without leaving their work place at the Puskesmas, clinics, hospitals and other health care facilities. This means that public services are not disrupted, especially in disadvantaged areas, hard to reach areas (DTPK), and regions with poor health outcomes such as NTT.
systems; the development of over 400 training modules; training of trainers and supervisors as well as establishing management, scholarship payment and administrative systems.
The model developed through AIPHSS has been evaluated to inform government policy for scale up to other regions. This evaluation is summarised in Annex 9. The main limitation of the system has been the limited Internet access in some areas due to poor infrastructure and reduced bandwidth. This hampers overall performance of the system and is a disadvantage for some students in remote areas. To overcome infrastructure restrictions the ISP has provided all modules in hardcopy form in advance. Students can also get the materials on CD or USB flash drive from the administrators.
In terms of overall content, the PJJ modules need strengthening in the area of gender quality and social inclusion, and consolidation to ensure they are focussed more on workplace issues with a reduction in the amount of time spent on generic subjects. An initial evaluation during the reporting period identified the need for modules to counteract the tendency of some local service providers to stereotype patients and deny access to critical services or information. For examples nurses and midwives need to ensure that their moral judgement is not dictating the level of medical treatment they are willing to provide, for instance, ensuring that unmarried pregnant females receive the same treatment as married pregnant females without judgement.
The first batches of trainees in SBD and Flotim commenced in July 2014 and are now in the second semester. The new batches of students are being prepared in Ngada and TTU.
What has emerged from this investment is a model of how distance based learning system can be established. The estimation is that 115,000 nurse and midwives need to reach the new standard of Diploma III. The contribution of this investment is a model for government which can now be scaled up. Evidence of this is now emerging where new districts in NTT are requesting the implementation of PJJ and are ready to fund this through local government funds.
Intermediate Outcome: Health legislation to Implement Minimum Services Standards is enacted
During 2013- 2014, AIPHSS contracted the Asosiasi Dinas Kesehatan (ADINKES) to undertake a revision of the MSS and health section of the decentralisation law (UU-32/2004). The revision is now formulated in Law-23/2014 which was enacted in October 2014. The combination of the new law together with the MSS will impose a performance based planning and budgeting system for health programs at the district level. The model for this will be developed by AIPHSS in the next reporting period. In addition the quantitative targets of MSS, and the sanctions imposed on districts failing to achieve the targets, will contribute to greater local accountability and improved governance for health development. Furthermore, the new MSS cover services based on the essential needs of all
segments of a district population, including family planning which has been neglected over the last decade.
Health System changes due to Law UU23/20014 and MSS
AIPHSS is now preparing a strategic approach for the implementation of the new legislation and MSS in AIPHSS districts. The implementation of the law places new functions and responsibilities on the District Health Office (DHO) as well as the Puskesmas. For example the DHO has a new function in coordinating local hospitals and other health facilities at the district level. This is in accordance with district level obligatory function to licensing class C and D hospital and health facilities. This type of functional change will require a new organisational structure and technical capacities in a DHO.
Equally important is the need to improve DHO capacity to plan and implement its new role in performance based planning and budgeting. All of the AIPHSS districts in NTT and JATIM are currently planning the provision of technical assistance to assist in the development of restructuring and organisational standards and governance of DHO to facilitate the implementation of the new policies. This will lead to a model of policy implementation that may be used by other provinces and districts as an approach to implementing the new polices and standards.
deliver improved health services and a better quality of care through Puskesmas. A workshop will be held in September 2015 with all key stakeholders (Bappeda, BKD, BPJS and hospitals) to begin to develop the model, including financing mechanisms. It is expected that the cost of implementing the model can be supported by local government. However, many of the recommended changes do not require funding but changes in process and instructions to embed good practices and new
regulations.
Intermediate Outcome: Guidelines on activity implementation standards and procedures
The major activity commencing in this reporting period was the preparation of the Norms, Standards, Procedures and Criteria (N