Chronic endothelial dysfunction after oversized coronary balloon
angioplasty in pigs: a 12-week follow-up of coronary vasoreactivity
in vivo and in vitro
Francisco A.H. Fonseca
a,b, Maria C.O. Izar
a,b, Valentin Fuster
a,b, Richard Gallo
a,b,
Adrian Padurean
a,b, John T. Fallon
a,c, E. Neil Schachter
d, James H. Chesebro
a,b,
Juan J. Badimon
a,b,*
aCardio6ascular Biology Research Laboratory,Cardio6ascular Institute(Box1030),Annenberg Building24,Mount Sinai School of Medicine,
One Gusta6e Le6y Place,New York,NY10029,USA
bThe Zena and Michael A.Wiener Cardio6ascular Institute,Mount Sinai School of Medicine,New York,NY,USA cDepartment of Pathology,Mount Sinai School of Medicine,New York,NY,USA
dPulmonary Di6ision,Mount Sinai School of Medicine,New York,NY,USA
Received 7 June 1999; received in revised form 14 February 2000; accepted 2 March 2000
Abstract
Previous studies have reported the development of vasoconstriction immediately after invasive coronary interventions. Other studies in animals have demonstrated that using oversized balloon angioplasty, vasospasm can be suppressed, even in the presence of endothelial denudation due to important structural alteration in vascular smooth muscle. The regenerated endothelium also appears to be impaired chronically by selective attenuation of in vitro endothelial dependent relaxation related to pertussis toxin-sensitive G proteins. The purpose of this investigation was to verify in vivo and in vitro vasoreactivity to bradykinin (BK) and serotonin (5-hydroxytryptamine; 5-HT) (endothelial dependent agonists) as well as to nitroglycerin (NTG) (exogenous nitric oxide donor) at different times after oversized balloon angioplasty intervention ranging from 1 h to 12 weeks, in normal porcine coronary arteries. BK-induced vasodilatation in vivo was impaired acutely, but it was restored after 4 weeks. Serotonin caused vasoconstriction in vivo that was significantly augmented after 12 weeks. Conversely, endothelium-dependent vasodilatation in vitro to BK and 5-HT remained attenuated during the whole period of follow-up. Finally, relaxation elicited by NTG was reduced in the in vivo experiment until the first week after the procedure. Histological analysis showed severe arterial injury, and complete recovery of endothelial coverage after 4 weeks. In conclusion, this experiment supports evidence for the occurrence of the acute attenuation of vasoresponsiveness and chronic endothelial dysfunction following overstretching coronary balloon angioplasty. Abnormal remodeling associated with the severity of injury may contribute to chronic endothelial dysfunction. Differences found between in vivo and in vitro studies also suggest that multiple endogenous influences present in the former can attenuate the greater endothelial dysfunction demonstrated by endothelial assessment in vitro. © 2001 Elsevier Science Ireland Ltd. All rights reserved.
Keywords:Vasoconstriction; Invasive coronary inteerventions; Balloon angioplasty
www.elsevier.com/locate/atherosclerosis
1. Introduction
Abnormal vasoreactivity has been observed in the presence of impaired endothelial function [1 – 3]. Vascu-lar interventions such as coronary balloon angioplasty
promote a cascade of cellular injuries that include wide endothelial denudation and damage to the underlying vascular tissue as well [4,5]. Early in vitro experiments examining the recovery of endothelial function showed that regenerated endothelial cells selectively lose some G protein-coupled responses [6,7]. The lack of the protective role of the endothelium against vasoconstric-tor products released from platelets may contribute to vasospasm and thrombosis [8]. The importance of
en-* Corresponding author. Tel.: +1-212-2418483; fax: + 1-212-4266962.
E-mail address:[email protected] (J.J. Badimon).
dothelial integrity also includes the inhibitory effects on cells and molecule adhesion, smooth muscle cell prolif-eration, and matrix synthesis which appear to be crucial during vascular repair and restenosis [9 – 11]. Some in vivo human studies have also demonstrated endothelial dysfunction following vascular interventions, however, the presence of concomitant atherosclerosis, hyperten-sion, dyslipidemia, tobacco or diabetes are variables that can lead to paradoxical vasoresponses [12 – 15].
The aim of this study was the simultaneous assess-ment of vasoreactivity in vivo and in vitro using two different pathways for the endothelium-dependent va-sodilatation after oversized balloon angioplasty in nor-mal porcine coronary arteries.
2. Material and methods
2.1. Animals
This project was approved by the Mount Sinai School of Medicine animal management program which is accredited by the American Association for the Accreditation of Laboratory Animal Care (AAALAC) and meets NIH standards as set forth in the ‘Guide for the Care and Use of Laboratory Animals’. Thirty-two Yorkshire albino pigs of both sexes, 9 – 12 weeks of age, weighing 23 – 29 kg, were used. The animals were housed individually and fed a regular chow. During the coronary interventions, the animals were initially sedated with ketamine hydrochloride (15 mg/kg, i.m.) and then deeply anesthetized with sodium pentobarbital (25 mg/kg, i.v.). They were intubated and ventilated. Additional intermittent boluses of pentobarbital were intravenously administered to avoid any unnecessary discomfort during the procedure.
2.2. Coronary angioplasty
Coronary angioplasty was performed as previously described [16]. Briefly, arterial access was obtained via either right or left femoral artery. All the animals received a 100 IU/kg of initial heparin bolus followed
by another bolus of 50 IU/kg per h after 1 h of
experiment. Under fluoroscopic guidance, coronary bal-loon angioplasty was performed in two of the three major epicardial coronary arteries using a 0.014 angio-plasty guide wire (Advanced Cardiovascular System, CA) and the balloon catheter (20 mm length and 4 mm maximal diameter, Cordis) was placed at the proximal site of the respective coronary artery. Angioplasty was performed by three inflations, the first at 8 atm for 15 s, and the second and third at 10 atm for 20 s, with 60-s rest periods between inflations. Angiograms were taken before, during and after balloon angioplasty. Bal-loon:vessel ratio was measured and was comparable
among these coronaries (1.2690.03). After the angio-plasty procedure, the arterial sheath was removed and the skin wound closed with sutures. The animals were allowed to recover, returned to their pens and were then reanesthetized at 1, 2, 4, 8 or 12 weeks post-PTCA for vasoreactivity studies.
2.3. Coronary 6asoreacti6ity in6i6o
A 3F infusion catheter was placed at the proximal site of the coronary artery and angiograms were ob-tained using nonionic contrast medium (Omnipaque) before and after each drug infusion. The protocol of drugs included in sequence: dextrose 5%, bradykinin (BK) (10−9– 10−7 M), serotonin (10−8– 10−6 M) and
nitroglycerin (NTG) (10−6 M). Each drug was infused
by a Harvard syringe pump with 4 ml of total volume at a rate of 2 ml/min, and there was a 15-min interval between each class of drug infusion. Pictures were taken at the same phase of cardiac cycle and changes in vessel diameter (compared to baseline angiogram) at the site of coronary angioplasty were measured blindly by two independent observers using an electronic digi-tal caliper [17,18].
2.4. Coronary 6asoreacti6ity in6itro
The animals were euthanized by an overdose of Sleepway (Fort Dodge Laboratories, NJ). The heart was removed and the ascending aorta was immediately cannulated. The heart was flushed with one liter of cold Krebs – Henseleit solution. The coronary arteries were carefully dissected with the heart immersed in the same solution and the region of injury was macroscopically identified and cut into four sections of 4 mm length. The same anatomic portion of untouched coronary arteries served as control. Therefore, twelve coronary rings obtained from the three major coronaries were studied simultaneously. Four coronary rings were tested for each agonist. The coronary rings were suspended horizontally between two stainless steel stirrups, in organ chambers filled with 20 ml Krebs – Henseleit solu-tion of the following composisolu-tion (mM): NaCl 110.0, KCl 4.8, CaCl22.3, KsPO41.2, MgSO41.2, NaHCO3
25, and glucose 11.0 at pH 7.4, 37°C, and gassed with 95% O2 and 5% CO2. Isometric tension was
simulta-neously recorded on a 12-channel polygraph (Model 7E, Grass Instrument Co, MA). Injured and control coronary rings were studied simultaneously. The tissues were allowed to equilibrate for 60 min under a tension of 5 g that had been determined previously to be the optimal tension for contraction of the porcine coronary arteries in our model. After this period the tension was readjusted and the tissues were incubated for 1 h with indomethacin (10−5
determine relaxations by 5-HT, the rings were also incubated with ketanserin (3×10−6 M) to avoid the
direct activation of 5-HT2receptors on vascular smooth
muscle. To examine vascular relaxations, the rings were precontracted with prostaglandin F2a (6×10−6 M).
After the maximal prostaglandin F2a-induced
contrac-tion was achieved, relaxacontrac-tion responses were deter-mined to increasing doses of BK (10−10– 10−7 M),
5-HT (10−9– 10−6 M), and NTG (10−9– 10−6 M)
given in log increments. Relaxations were expressed as the percent of the maximal tension of contracted tissue by prostaglandin F2a. Concentration-response curves
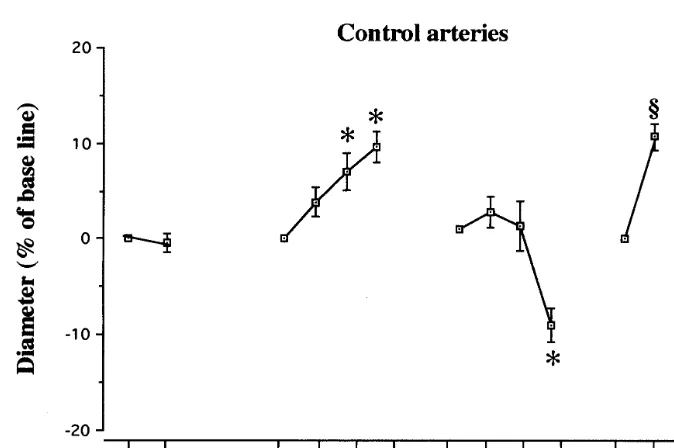
Fig. 1. Plot of percent lumen diameter change from base line (mean9SEM) at the proximal site of the control coronary arteries after intracoronary administration of dextrose 5%, increasing concentrations of BK and serotonin, and after NTG. §, PB0.05 versus base line (Wilcoxon signed rank sum test); *,PB0.05 vs base line (Friedman test)
Table 1
Assessment of coronary diameter changes after the infusion of 5% dextrose, BK, serotonin, and NTG at the site of intervention (mean9SEM)a,b
2 weeks 4 weeks 8 weeks 12 weeks 1 h
Drugs Control 1 week
1.891.1 0.691.0 1.291.2 0.590.8 D 5% −0.490.9 0.191.6 −2.593.8
4.992.3 3.794.5
0.491.6 −0.391.3
BK10−9M 3.991.5 1.091.8 0.390.4
−3.392.7* 3.293.4 6.592.3 10.792.6 BK10−8M 7.192.0 0.992.6 0.992.5*
9.791.6 −1.491.5** 2.490.6**
BK10−7M 3.292.2** 8.392.6 6.393.7 13.492.0
−0.893.3 −1.891.4
0.493.2 −1.692.3
5-HT10−8M 1.891.6 0.692.0 −3.794.5
−4.694.4 −1.092.6
0.492.6 −5.493.7
5-HT10−7M −1.292.7 −3.292.3 −7.793.2
−15.393.8 −18.993.0*** 5-HT10−6M −10.091.8 −0.890.9 −11.895.0 −13.093.1 −11.292.2
10.791.4 16.592.1
NTG10−6M 2.091.0**** 8.293.4**** 13.492.8 19.492.8 10.292.8
15 5
10 5
14 9 8
n
aValues are percent changes from base line and n refers to the number of arteries.
bLower mean rank *,P=0.023; **,P=0.0001; ***, P=0.0017; ****, P=0.0002 (Kruskal–Wallis test for comparison of the same drug
concentration between time-points).
Table 2
Assessment of heart rate, systolic (SBP) and diastolic blood pressure (DBP) changes after the infusion of 5% dextrose, BK, serotonin, and NTG, (mean9SD)
5-HT before
Group Dextrose before Dextrose after BK before BK after 5-HT after NTG before NTG after
117924 125927* 117928 125930* 115924 118928 Heart rate 115925 115925
156921 159921 148927* 155927 152925 156922 156922
SBP 158923
87922 80922* 85923 82923 88919 87920
88918 89919
DBP
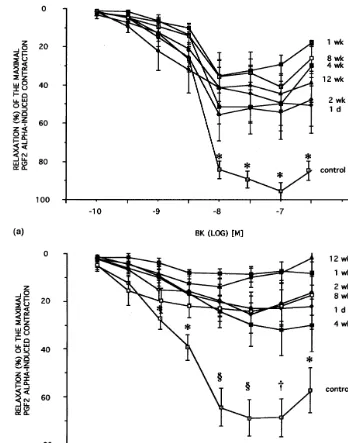
Fig. 2. (a): dose-response curve to BK in rings precontracted by PGF2a(6×10−6 M). Vasorelaxation to BK was impaired after injury (*,
PB0.05 control vs. all time-points, Kruskal – Wallis test). (b): endothelium-dependent vasodilatation elicited by 5-HT was also attenuated after injury. (PB0.05, * control vs. all time-points, § control vs. 1 week, 12 week, † control weeks 1 day, 1 week, 2 weeks, 8 weeks, 12 weeks).
were plotted using the Kaleidograph software (version 3.04) for the Power Macintosh 8200 (Cupertino, CA). Data points were fitted by iteration to the logistic function: E=Emax/1+(IC50/[A]n), where E, observed
muscle tension (grams above baseline); [A], the concen-tration of the agonist; IC50, the [A] eliciting one half of
the maximal response;n, slope of the curve.
2.5. Morphometric analysis
Injured and control coronary rings were fixed by immersion in 4% paraformaldehyde in 0.1 M PBS at
pH 7.4. Coronary segments were cross-sectioned at 2-mm intervals, paraffin embedded, sectioned (5 mm),
and stained with combined Masson elastin (CME). Immunohistochemical staining using biotinylated Doli-chos Biflorus Agglutinin (DBA, B-1035, Vector
Labo-ratories, Barlingame, CA) was used to identify
2.6. Drugs
Bradykinin acetate, and 5-HT creatine sulfate, in-domethacin and prostaglandin F2awere obtained from
Sigma Chemical Co (St Louis, MO); ketanserin bitar-trate from Janssen Pharmaceutica, Beerse, Belgium; and NTG from Abbott Laboratories, IL. Bradykinin,
5-HT, NTG and prostaglandin F2a were dissolved in
distilled water, indomethacin in supersatured TRIS-base, and ketanserin in dimethyl sulfoxide (DMSO, Sigma). All agonists are reported as molar concentra-tion present in the organ chamber. For in6i6o studies the drugs were infused diluted in 5% dextrose, and the final molar concentration reported was estimated on basis of a 80 ml/min coronary blood flow.
2.7. Statistical analysis
The data were expressed as mean9SEM. Unless
otherwise stated, n refers to the number of arteries. As a normal distribution cannot be assumed for both morphologic parameters and percent changes in
vasore-activity, the Kruskal – Wallis, and Friedman or
Wilcoxon signed rank sum tests were used to compare mean group values (StatView 512™). For comparison of heart rate and blood pressure changes after drug infusion, t-test (correlated groups) was used. AP value less than 0.05 was considered significant.
3. Results
3.1. Vasoreacti6ity in 6i6o
3.1.1. Dextrose
Vasoresponses to 5% dextrose (D5%), a control vehi-cle, observed in either normal or injured coronary arteries, were not significantly altered during the entire period of this study (Fig. 1).
3.1.2. Bradykinin
Following the infusion of bradykinin in noninjured coronary arteries, a significant increase in vessel diame-ter was observed (Fig. 1).
After balloon injury, vasodilatation to this agent was significantly attenuated during the first 2 weeks remain-ing comparable to control arteries after this period (Table 1).
3.1.3. Serotonin
The highest dose of 5-HT caused significant vasocon-striction in control arteries (Fig. 1). Vasoresponses to 5-HT after coronary angioplasty did not show signifi-cant changes except at 12 weeks, when the vasoconstric-tion elicited by this agent was significantly higher (Table 1).
3.1.4. Nitroglycerin
The NO-donor NTG induced significant vasodilation in normal coronary arteries (Fig. 1). However, after coronary balloon angioplasty, vasoresponse to this en-dothelium-independent agent was impaired until the first week. After this period, vasodilatation following NTG was comparable to that obtained in control arter-ies (Table 1).
During in vivo experiments there was a significant increase in heart rate only after BK and 5-HT. Mea-surements of systolic and diastolic blood pressure showed a significant decrease after BK (Table 2).
3.2. Vasoreacti6ity in 6itro
3.2.1. Bradykinin
The values for vasorelaxation obtained to BK in noninjured rings showed the classical dose-response curve (Fig. 2).
Vasoreactivity studies performed in ballooned rings showed endothelial dysfunction in response to BK dur-ing the whole period of follow-up (Fig. 2). Emaxvalues
obtained were also reduced during the same time-points (Table 3).
3.2.2. Serotonin
As observed for BK, the vasoresponses to the en-dothelium-dependent 5-HT in control rings showed the classical dose-response curve (Fig. 2).
The endothelium-dependent relaxation to 5-HT was reduced in the injured rings up to 12 weeks after the coronary intervention when compared to control rings. Emax values for this drug remained reduced after
bal-loon angioplasty (Table 3).
3.2.3. Nitroglycerin
This endothelium-independent agent also promoted the classical dose-response curve in noninjured rings, andEmaxvalues for this agent did not differ from those
observed for control rings (Table 3).
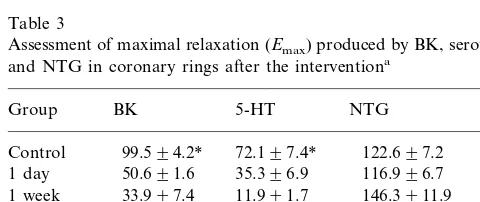
Table 3
Assessment of maximal relaxation (Emax) produced by BK, serotonin,
and NTG in coronary rings after the interventiona
Group BK 5-HT NTG n
aValues are percent changes after maximal PGF2
a-induced
con-traction plotted in the Kaleidograph software (mean9SEM) andn refers to number of arteries.
* Higher Emax value *,P=0.0001 (Kruskal–Wallis test forEmax
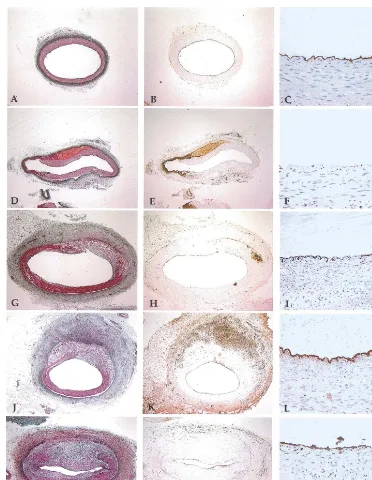
Fig. 3. Cross-sections of porcine coronary arteries. A, B, and C are control specimens showing integrity of vessel layers and complete endothelial coverage. D, E, and F are 2-week specimens showing intimal thickening and partial endothelial coverage. G, H, and I are 4-week specimens showing complete endothelial regeneration. J, K, and L are 12-week specimens showing important intimal proliferation at the site of IEL rupture. A, D, G, and J are CME (×40); B, E, H, and K are DBA (×40); C, F, I, and L are DBA magnifications (×400).
3.3. Morphology
Oversized coronary balloon angioplasty caused deep vascular injury characterized by an extensive endothe-lial denudation, disruption of the internal elastic lamina (IEL), and thrombus formation. After 2 weeks large luminal areas remained without endothelium, thrombi were still present, and areas of intimal thickening were observed, specially at the site of IEL rupture (Fig. 3). Histomorphometric analysis showed reduced presence of endothelium-positive staining by DBA at 1 day, and
at 1 and 2 weeks after balloon angioplasty when
com-pared to control, noninjured segments (1 day 28.49
9.9%; 1 week 44.895.8%; 2 weeks, 53.394.7%; 4
weeks 93.495.4%; 8 weeks 92.893.4%; 12 weeks
89.894.5%). Largely complete regeneration of the en-dothelial layer was observed 4 weeks after balloon injury (Fig. 4).
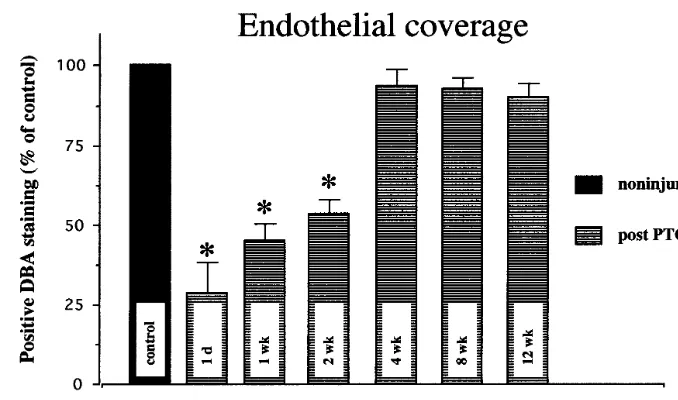
Intima, media and intima/media ratios were also
Fig. 4. Endothelial coverage. Data were obtained from percentages of DBA-labelled luminal perimeters obtained in control specimens. Coronary specimens were examined in a blinded fashion (controln=19, 1 dayn=9, 1 weekn=10, 2 weekn=19, 4 weekn=13, 8 weekn=13, 12 week n=20). The amount of endothelium present was reduced in the short-term follow-up. (* lower endothelial coverage, Kruskal – Wallis test).
4. Discussion
This study demonstrates that vasoreactivity after oversized balloon angioplasty is acutely impaired due to losses of endothelial integrity and severe damage to vascular structure. Despite endothelial regeneration and the functional recovery of smooth muscle cells, altered in vitro vasoresponses to BK and 5-HT were still observed 12 weeks after the intervention. Conversely, in vivo vasodilatation induced by BK was apparently restored after 4 weeks, suggesting differences in the endothelial function assessment between these two methods. Interestingly, progressive impairment of va-sodilatation was seen during the long-term follow-up supporting that the arterial remodeling, including inti-mal thickness, may be associated with a barrier to the complete expression of endothelium-dependent vasodi-latation. Simultaneous assessment of endothelial func-tion in vivo and in vitro was important to show some differences between these two methods.
The porcine model of coronary balloon angioplasty was chosen due to morphologic similarities between human and porcine coronary arteries after balloon angioplasty, and use of identical technical approaches [4,19]. Human balloon angioplasty induces deep vascu-lar damage through vessel stretching as well as endothe-lial injury. Therefore, the data collected from the overstretched balloon injury model provide more rele-vant information regarding endothelial function and the healing process than those extrapolated from the endothelial denudation models [20]. In addition, this study was performed in normal coronary arteries to assess the endothelial function after injury indepen-dently of other variables such as hyperlipidemia or
atherosclerosis. The site of internal elastic lamina rup-ture in our specimens represented the region of the major arterial injury, where thrombus, submedial he-matoma and media rupture were associated later to the highest intimal thickness, showing the importance of these morphologic findings in regard to neointima hy-perplasia. Previous experiments have demonstrated that the smooth muscle cell migration and proliferation occurs early during the neointima formation and lack of the internal elastic membrane integrity should be an important step in this process.
In our study, vasoreactivity was markedly and acutely impaired after oversized balloon angioplasty. This finding is in agreement with previous reports [20 – 22] that suggest attenuation of vasoreactivity as a result of mechanical impairment of smooth muscle cells. In support of this hypothesis, stretching, straightening, and necrosis of smooth muscle cells were described in histological studies after balloon angioplasty [21,23]. These reports can explain the impaired vasoresponses
Table 4
Histomorphometric analysis of intima, media and intima/media ratio (I/M) performed at 4, 8 and 12 weeks after coronary balloon angioplastya
Media (mm2) n
Intima (mm2)
Time-point I/M
0.3590.06 11 4 weeks 0.7390.17 1.8990.35
0.3890.06
2.0090.15 12
0.8190.15 8 weeks
28 1.2190.16 0.4390.03
12 weeks 2.6390.16*
aValues are mean9SEM andnrefers to the specimens obtained
from coronary rings used in the in-vitro experiment.
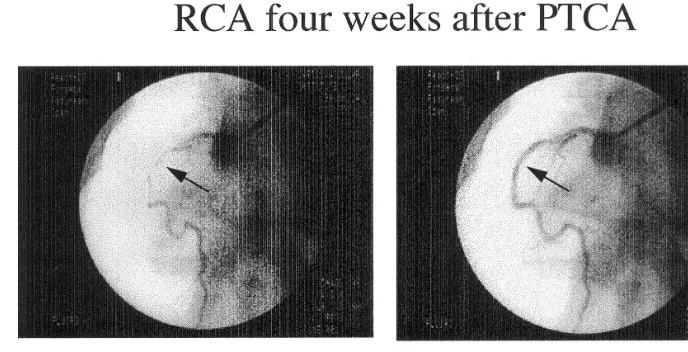
Fig. 5. Coronary arteriogram 4 weeks after balloon angioplasty. Panel at left shows vasoconstriction induced by 5-HT (10−6M) at the site of
angioplasty (arrows) and the panel at right shows dilatation of the same segment of the right coronary artery in response to NTG (10−6 M).
not only to the endothelium-dependent agonists 5-HT and BK but also to the NO donor NTG. Furthermore, they provide an attractive hypothesis for the elastic recoil occurrence, where the initial luminal gain is lost in hours or a few days. As in vitro vasoreactivity was performed one day after the in vivo experiment, when vasodilatation after NTG was restored, there was evi-dence that the acute impairment observed in vivo at 1 h should be transient. However, even using the same drugs, in vivo and in vitro studies may differ substan-tially. Firstly, in vivo studies have potential endogenous mechanisms to increase or decrease vasoresponses, e.g. free radicals, endothelin, constrictor prostanoids, and also endothelium-derived dilator products (NO, PGI2,
EDHF) yielded by endothelium cells adjacent to the injured area. On the other hand, in vitro studies were performed in precontracted rings, blocked against prostanoid influences.
Experimental studies using the balloon denudation plus high cholesterol diet model showed selective lack of some G protein-coupled responses from the regener-ated endothelium [6,7,24]. Endothelium-dependent
re-laxation to BK is mediated by B2 receptors that
stimulate the release of endothelium-derived relaxing factor (NO), prostacyclin and endothelium-dependent hyperpolarizing factor [24,25]. In our experiment, BK-induced vasodilatation was restored in vivo 4 weeks after angioplasty, showing that the regenerated en-dothelium is capable of responding properly at least to some agonists [5,11,14,19 – 21]. However, the vasore-sponses to this agent remain impaired during in vitro studies in the long-term follow-up and a greater sensi-tivity for endothelial evaluation provided by in vitro studies is one possibility. In regard to endothelium-de-pendent vasodilatation promoted by 5-HT, both in vivo and in vitro studies showed chronic impairment. Sero-tonin promotes vasodilatation through the activation of
5-HT1 receptors present on endothelial cells. However,
5-HT can also activate 5-HT2 receptors which are
re-sponsible for the vasoconstrictor response [26] (Fig. 5). Therefore, the exaggerated vasoconstrictor responses to 5-HT observed at 12 weeks suggest the predominance of 5-HT2 receptor activation, and this response can be
increased through the profound morphologic changes in the vessel wall after 12 weeks. In fact, the increased amount of matrix in the long-term follow-up can con-tribute to the endothelial dysfunction either as a barrier to NO or impairing the vasodilatation (Fig. 3, Table 4). Summarizing, our study provides evidence that fol-lowing an oversized balloon angioplasty, vascular re-sponsiveness is acutely attenuated due to deep vascular damage. In addition, even after complete recovery of endothelial coverage and vascular smooth muscle in-tegrity, an abnormal remodeling associated with a criti-cal amount of intimal mass may contribute to chronic endothelial dysfunction. Finally, simultaneous assess-ment of in vivo and in vitro vasoreactivity showed minor and interesting differences in responses to all agents used, suggesting that the release of endogenous substances in vivo and other particular conditions of in vitro studies can modify the magnitude of vasore-sponses during the endothelial assessment.
Acknowledgements
This study was supported in part by FAPESP (Fun-dac¸a˜o de Amparo a` Pesquisa do Estado de Sa˜o Paulo)
grant 95/2778-9. The authors acknowledge Veronica
References
[1] Furchgott RF, Zawadzki JV. The obligatory role of endothelial cells in the relaxation of smooth muscle by acetylcholine. Nature 1980;288:373 – 6.
[2] Mc Fadden EP, Bauters C, Lablanche JM, et al. Response of human coronary arteries to serotonin after injury by coronary angioplasty. Circulation 1993;88:2076 – 85.
[3] Fonseca FAH, Paiva TB, Silva E, et al. Dietary magnesium improves vasoreactivity of injured vessels. Atherosclerosis 1998;139:237 – 42.
[4] Bonan R, Paiement P, Leung TK. Swine model of restenosis: effect of a second injury. Cathet Cardiovasc Diagn 1996;38:44 – 9.
[5] Groves PH, Banning AP, Penny WJ, et al. Kinetics of smooth muscle cell proliferation and intimal thickening in a pig carotid model of balloon injury. Atherosclerosis 1995;117:83 – 96. [6] Shimokawa H, Flavahan NA, Vanhoutte PM. Natural course of
the impairment of endothelium-dependent relaxations after bal-loon endothelial removal in porcine coronary arteries: possible dysfunction of a pertussis toxin-sensitive G protein. Circ Res 1989;65:740 – 53.
[7] Shimokawa H, Flavahan NA, Vanhoutte PM. Loss of endothe-lial pertussis toxin-sensitive G protein function in atherosclerotic porcine coronary arteries. Circulation 1991;83:652 – 60. [8] Lam JYT, Chesebro JH, Steele PM, et al. Deep arterial injury
during experimental angioplasty: relation to a positive indium-111, labeled platelet scintigram, quantitative platelet deposition and mural thrombosis. J Am Coll Cardiol 1986;8:1380 – 6. [9] Badimon L, Badimon JJ, Penny W, et al. Endothelium and
atherosclerosis. J Hyperten 1992;10(2):43 – 50.
[10] Asahara T, Chen D, Tsurumi Y, et al. Accelerated restitution of endothelial integrity and endothelium-dependent function after phVEGF165 gene transfer. Circulation 1996;94:3291 – 302. [11] VanBeusekon HMM, Whelan DM, Hofma SH, et al. Long-term
endothelial dysfunction is more pronounced after stenting than after balloon angioplasty in porcine coronary arteries. J Am Coll Cardiol 1998;32:1109 – 17.
[12] El-Tamimi H, Davies GJ, Crea F, et al. Response of human coronary arteries to acetylcholine after injury by coronary angio-plasty. J Am Coll Cardiol 1993;21:1152 – 7.
[13] Tousoulis D, Davies G, Tentolouris C, et al. Effects of ke-tanserin on epicardial coronary arteries after coronary angio-plasty in patients with stable angina. Eur Heart J 1994;15:922 – 7.
[14] Hamon M, Bauters C, McFadden EP, et al. Hypersensitivity of human coronary segments to ergonovine 6 months after injury by coronary angioplasty: a quantitative angiographic study in consecutive patients undergoing single-vessel angioplasty. Eur Heart J 1996;17:890 – 915.
[15] Wever RMF, Luscher TF. Atherosclerosis and the two faces of endothelial nitric oxide synthase. Circulation 1998;97:108 – 12. [16] Gallo R, Padurean A, Toshi V, et al. Prolonged thrombin
inhibition reduces restenosis after balloon angioplasty in porcine coronary arteries. Circulation 1998;97:581 – 8.
[17] Schwarzacher SP, Lim TT, Wang B. Local intramural delivery of L-arginine enhances nitric oxide generation and inhibits lesion formation after balloon angioplasty. Circulation 1997;95:1863 – 9.
[18] Schwartz RS, Edwards WD, Bailey KR, et al. Differential neointimal response to coronary artery injury in pigs and dogs. Arterioscler Thromb 1994;14:395 – 400.
[19] Roussel F, Dalion J. Lectins as markers of endothelial cells: comparative study between human and animal cells. Lab Anim 1988;22:135.
[20] Hata H, Ohara Y, Kuga T, et al. Vasoreactivity and restenosis after coronary angioplasty in the atherosclerotic pig model. Cor Art Dis 1995;6:503 – 11.
[21] Chan PDS, Findlay JM, Vollrath B, et al. Pharmacological and morphological effects of in vitro transluminal balloon angio-plasty on normal and vasospastic canine basilar arteries. J Neurosurg 1995;83:522 – 30.
[22] Uren NG, Crake T, Lefroy DC, et al. Altered resistive vessel function after coronary angioplasty is not due to reduced pro-duction of nitric oxide. Cardiovasc Res 1995;32:1108 – 14. [23] Megyesi JF, Findlay JM, Vollrath B, et al. In vivo angioplasty
prevents the development of vasospasm in canine carotid arter-ies. Pharmacological and morphological analyses. Stroke 1997;28:1216 – 24.
[24] Nakashima M, Mombouli J, Taylor A, et al. Endothelium-de-pendent hyperpolarization caused by bradykinin in human coro-nary arteries. J Clin Invest 1993;92:2867 – 71.
[25] Ishida T, Hirata K, Sakoda T, et al. Identification of mRNA for 5-HT1 and 5-HT2 receptors subtypes in human coronary arter-ies. Cardiovasc Res 1999;41:267 – 74.