1
Recent guidelines in the management of non-variceal bleeding
I Dewa Nyoman Wibawa
Div.Gastroentero-hepatology,Dept.of Internal Medicine UdayanaUniv.;School of Medicine/Sanglah General Hospital.
Extended abstract
In recent years there are several novel developments in the management of non-variceal bleeding has been growing very rapidly. Some novel guidelines emerged as the latest guidelines on the management of non-variceal bleeding.
There are small differences between the new guideline with the previous one.One of the latest guideline is issued by ESGE 2015.
As we know acute upper gastrointestinal hemorrhage (UGIH) is a common condition worldwide that has an estimated annual incidence of40−150 cases per 100 000 populations, frequently leads tohospital admission, and has significant associated morbidity and mortality, especially in the elderly. The most common causes of acute UGIH are non-variceal. This includes peptic ulcers, 28%–59% (duodenal ulcer 17%–37% and gastric ulcer 11%–24%); mucosal erosive disease of the esophagus/stomach/duodenum, 1%–47%; Mallory–Weiss syndrome, 4%–7%; upper GI tract malignancy,2%– 4%; other diagnosis, 2%–7%; or no exact cause identified 7%–25%. Moreover, in 16%–20% of acute UGIH cases, more than one endoscopic diagnosis may be identified as the cause of bleeding.1
Based on several guideline available, endoscopic and PPI therapies are cornerstones to management of non-variceal bleeding. The current debated issues are; whether early endoscopy improves clinical outcomes and the paradoxical effect of blood transfusion to recurrent bleeding. The management of patients on antithrombotic drugs is complex.2
2 resumed early. A low dose PPI should beadded for secondary prophylaxis. In those who continue to require an analgesic, co-therapy of PPI with traditional non-steroidal anti-inflammatory agentand the use of COX-II inhibitor alone are associated with a small risk of recurrent bleeding. A combination of COX-II inhibitor and PPI is preferred in thosewith very high risk of gastrointestinal events. In patients on dual antiplatelet agents, PPI appears to reduce gastrointestinal events without increasingcardiovascular events.2,3,4
Guideline consensuses for the management of non-variceal bleeding still present some uncertainties. With regards to initiating blood products, some evidence suggests that liberal transfusion could exacerbate bleeding severity, although there is a paucity of large RCTs. Conversely, it is clear that prompt endoscopy (within 24 hours) improves outcomes, but evidence suggests that lowering this threshold (e.g. to 12hours) confers no additional benefit. The useof PPIs, both pre and post endoscopy, for nonvariceal bleeds is also advocated by professional bodies, with substantial evidence that it reduces the risk of re-bleeding.5
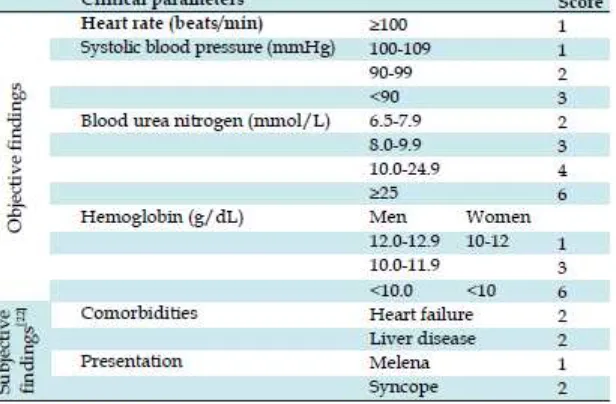
[image:2.595.132.440.444.646.2]Asia-Pacific Working Group consensus on non-variceal upper gastrointestinal bleeding stated that in the way to assess the need for endoscopic intervention in Asian patients with UGIB, the Blatchford score is preferred (table 1). When an emergency endoscopy service is available over weekends and public holidays, no increased mortality is seen at these times. High-dose oral PPIs may be effective in reducing rebleeding in Asian patients. Among patients receiving clopidogrel and aspirinas dual treatment, prophylactic use of a PPI is still recommended to reduce the risk of adverse gastrointestinal (GI) events. 6
Table 1. Risk stratification – Modified from Glasgow Blatchford risk score (GBS).4
3 present with hematemesis or bright red blood per nasogastric tube aspirate are at particularly high risk for rebleeding within the first 72 h.7
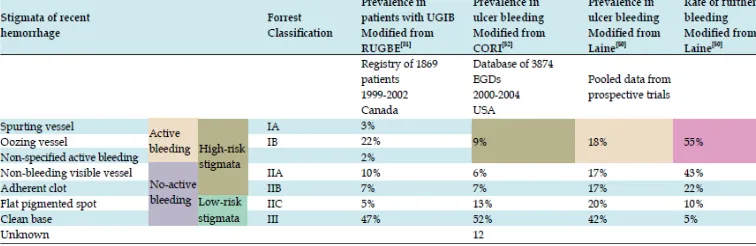
Endoscopic modalities used in the management of acute UGIB are classified into injection, thermal and mechanical therapies. Endoscopic hemostasis should be performed for all lesions exhibiting HRS (high Risk Stigmata) (Table 2) given high rates of rebleeding and improved outcomes with endoscopic treatments.4
Table 2. Endoscopic identification of stigmata of recent bleeding and associated prevalence and outcomes.4
In the management of cases with non-variceal bleeding, adequate resuscitation and initial risk assessment are crucial. Summay of all modalities in the management of non-variceal bleeding are as follows: Early endoscopy allows for categorization of patients into low versus high-risk of rebleeding and delivery of endoscopic hemostasis. Prokinetics are helpful in visualizing bleeding lesions at the initial endoscopy. Dual endoscopic modality therapy is superior to epinephrine injection alone followed by continuous PPI infusion for 72 hours should be applied for high-risk stigmata of rebleeding.8
All patients should be discharged on a single daily oral dose of a PPI the duration of PPI is determined by the underlying etiology of the bleeding ulcer, while in patients who are on antiplatelet agents, the cardiothrombotic risks should be balanced against the risk of further bleeding or rebleeding. ASA should be soon restarted in patients with high-risk of cardiothrombotic events. Finally, all patients presenting with bleeding ulcers should be tested for H. pylori, understanding that there is a high false negative rate in the acute setting of UGIB. 8
Further reading
1. Gralnek IM, Dumonceau J-M, Kuipers EJ, Lanas A, Sanders DS, Kurien M, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Nonvariceal upper gastrointestinal hemorrhage: ESGE Guideline. Endoscopy 2015; 47: a1–a46.
2. Lau JYW. Evidence-based management of patients with acute non-variceal upper gastrointestinal bleeding.Gastrointest Interv 2012; 1:53– 57.
3. Holster IL, Kuipers EJ. Management of acute nonvariceal upper gastrointestinal bleeding: Current policies and future perspectives. World J Gastroenterol 2012; 18(11): 1202-1207.
[image:3.595.126.504.205.328.2]4 Hepatology Research 2015; 4(3): 1515-1523. Available from: URL: http://www.ghrnet.org/index.php/joghr/article/view/1122.
5. Taylor AA, Redfern OC, Pericleous M. The management of acute upper gastrointestinal bleeding: a comparison of current clinical guideline and best practice. EMJ Gastroenterol. 2014;3:73-82.
6. Sung JJY, Chan FKL, Chen M, Ching JYL, Ho KY, Kachintorn U, et al. Asia-Pacific Working Group consensus on non-variceal upper gastrointestinal bleeding.Gut 2011;60:1170-1177. doi:10.1136/gut.2010.230292.
7. Maggio D, Barkun AN, Martel M,Elouali S, Gralnek IM, the REASON investigators Predictors of early rebleeding after endoscopic therapy in patients with nonvariceal upper gastrointestinal bleeding secondary to high-risk lesions. Can J Gastroenterol 2013;27(8):454-458.