Evidence-informed management of chronic low back pain with
transcutaneous electrical nerve stimulation, interferential current,
electrical muscle stimulation, ultrasound, and thermotherapy
Ste´phane Poitras, PhD, PT
a,*
, Lucie Brosseau, PhD, PT
baDepartment of Epidemiology and Biostatistics, Faculty of Medicine, McGill University, Montre´al, Quebec, Canada
bPhysiotherapy Program, School of Rehabilitation Sciences, Faculty of Health Sciences, University of Ottawa, Ottawa, Ontario, Canada
Received 4 October 2007; accepted 13 October 2007
Abstract EDITORS’ PREFACE: The management of chronic low back pain (CLBP) has proven to be very challenging in North America, as evidenced by its mounting socioeconomic burden. Choosing among available nonsurgical therapies can be overwhelming for many stakeholders, including pa-tients, health providers, policy makers, and third-party payers. Although all parties share a common goal and wish to use limited health-care resources to support interventions most likely to result in clinically meaningful improvements, there is often uncertainty about the most appropriate interven-tion for a particular patient. To help understand and evaluate the various commonly used nonsurgi-cal approaches to CLBP, the North American Spine Society has sponsored this special focus issue ofThe Spine Journal, titled Evidence-Informed Management of Chronic Low Back Pain Without Surgery. Articles in this special focus issue were contributed by leading spine practitioners and re-searchers, who were invited to summarize the best available evidence for a particular intervention and encouraged to make this information accessible to nonexperts. Each of the articles contains five sections (description, theory, evidence of efficacy, harms, and summary) with common subheadings to facilitate comparison across the 24 different interventions profiled in this special focus issue, blending narrative and systematic review methodology as deemed appropriate by the authors. It is hoped that articles in this special focus issue will be informative and aid in decision making for the many stakeholders evaluating nonsurgical interventions for CLBP. Ó2008 Elsevier Inc.
All rights reserved.
Keywords: Common low back pain; Therapeutic modalities; Transcutaneous electrical nerve stimulation (TENS)
Description
Terminology
Therapeutic modalities is a broad term referring to a va-riety of instruments, machines, and tools traditionally used in physical therapy for musculoskeletal conditions,
including CLBP. Two important categories of modalities used in CLBP are electrotherapeutic and physical agents [1,2].
Electrotherapeutic modalities involve the use of electric-ity and include therapies such as transcutaneous electrical nerve stimulation (TENS), electrical muscle stimulation (EMS), and interferential current (IFC)[3]. TENS delivers an electrical current through superficial electrodes placed on the skin around the affected area, causing a tingling sen-sation and disrupting the pain signal in surrounding nerves. Devices may be large clinical units or battery operated and portable. EMS delivers an electrical current through super-ficial electrodes placed on the skin causing one or more muscles to contract, which is thought to promote blood sup-ply and help strengthen the affected muscle. IFC delivers a high-frequency (4,000 Hz) electrical current through
FDA device/drug status: approved for these indications (TENS, inter-ferential current, electrical muscle stimulation, and ultrasound).
Nothing of value received from a commercial entity related to this manuscript.
* Corresponding author. Physiotherapy Program, School of Rehabilita-tion Sciences, Faculty of Health Sciences, University of Ottawa, 451 Smyth Road, Ottawa, Ontario K1H 8M5, Canada. Tel.: (613) 562-5800 Ext. 8121.
E-mail address: [email protected](S. Poitras)
superficial electrodes placed on the skin around the affected area, which is thought to penetrate the skin more deeply and cause less user discomfort than TENS.
Physical agents are modalities that involve thermal, acoustic, or radiant energy and include ultrasound (US), superficial heat (hot packs), and cryotherapy (cold packs or ice)[3].
US produces sound waves transmitted to the affected area through a handheld probe using conductive gel, thought to penetrate deep tissues and improve healing.
Hot packs are typically reusable, moldable bags of gel that are heated and wrapped in moist towels before being placed on the affected area to provide heat thought to pro-mote muscle relaxation through vasodilatation. Cold packs are typically reusable, moldable bags of gel that are frozen and wrapped in moist towels before being placed on the affected area to provide cold thought to promote vasocon-striction and decrease inflammation. Other types of modal-ities used in the treatment of CLBP include laser therapy, electromyography/biofeedback, iontophoresis, electromag-netic fields, diathermy, and vapocoolant spray; these will not be discussed in this review.
History
Electrotherapeutic modalities and physical agents have long been used in the management of CLBP, especially by physical therapists [1,2]. Depending on the type of modality/agent, they can be used to pursue the following objectives: reduce pain, inflammation, or tissue restriction, and increase movement and healing through vasodilation and neurostimulation.
Subtypes
Common electrotherapeutic modalities include TENS, EMS, and IFC. Common physical agents include US, superficial heat (hot packs), and cryotherapy (cold packs or ice).
General description
There are numerous CLBP treatment protocols for each of the common electrotherapeutic modalities and physical agents. For TENS, EMS, and IFC, the intervention begins by exposing the skin in the lumbosacral area, which may be cleaned by the provider. Superficial skin electrodes are then placed over areas of pain (TENS, IFC) or targeted muscle groups (EMS) before attaching them to the devices. Current intensity will then be gradually increased until a tin-gling sensation is produced (TENS, IFC) or attainment of visible muscle contraction (EMS). The devices are then programmed to deliver current at constant or varying inten-sities over a period of 15 to 30 minutes, during which the provider will periodically inquire about patient comfort and may increase current intensity to maintain a steady stimulus.
With US, the intervention begins by exposing and clean-ing the skin in the lumbosacral area. Conductive gel is then applied to the handheld US probe and spread over the treat-ment area. The US device is then activated and a specific intensity (watts/cm2) and cycle (pulsed or continuous) are selected based on target tissue thickness, stage of healing, and desired effect. The provider then slowly moves the US probe in circular motions over the target area during a specific treatment time, usually 6 to 10 minutes. Unlike TENS, EMS, and IFC, patients may not directly perceive US while it is applied.
Hot or cold therapy involves the provider applying one or more layers of towels to the targeted area before apply-ing the hot or cold pack for a specific period of time (usu-ally 10–20 minutes) or until the area is suitably hot or cold, as reported by the patient.
Practitioner, setting, and availability
Electrotherapeutic modalities and physical agents are typ-ically administered by physical therapists working in various practice settings nationwide (private practice, rehabilitation centers, or hospitals). Other health professionals involved in the management of CLBP, such as physicians, occupa-tional therapists, or chiropractors, may also use modalities or instruct patients on their use, especially for heat and cold therapy. Some modalities can be used at home by the patient following education by the clinician. For home use, the nec-essary equipment can be lent by the health professional to the patient, or the patient can rent or buy it. Some equipment can be directly obtained by the patient. These interventions are widely available throughout the United States.
Reimbursement
Pertinent Current Procedural Terminology codes include 64550: application of surface (transcutaneous) neurostimu-lator. Most insurers will generally reimburse the cost of electrotherapeutic modalities and physical agents adminis-tered by a licensed health provider for CLBP, though there may be provisions restricting the number of modalities that may be used at each visit.
Regulatory status
Electrotherapeutic devices and US are generally regu-lated by the FDA, though the level of evidence required for marketing approval is often much less than that of new drugs or surgical devices.
Theory
Mechanism of action
the rate of tissue healing[3]. Although the general mecha-nism of action for these interventions is summarized below, it is currently unknown if they apply specifically for CLBP. TENS may use low or high frequencies. At low frequency (5–10 Hz), TENS is thought to produce muscle contractions and provide pain reduction for several hours. At high frequency (80–100 Hz), TENS is thought to tempo-rarily reduce pain by acting as a counterirritant stimulus [4]. IFC is thought to temporarily reduce pain by acting as a counterirritant stimulus. EMS provokes muscle contractions in the applied region, which is thought to act as a counterirritant stimulus, reduce muscle spasm, and increase muscle strength and endurance.
US may be applied in continuous or pulsed mode. In the continuous setting, US converts nonthermal energy into heat, which increases deep soft-tissue extensibility and acts as a counterirritant stimulus, thereby temporarily reducing pain. Pulsed US is thought to promote deep soft-tissue heal-ing by improvheal-ing blood flow, alterheal-ing cell membrane activ-ity, and vascular wall permeability to the applied region[4]. Superficial heat is thought to temporarily reduce pain by acting as a counterirritant stimulus, increasing soft-tissue extensibility, and reducing muscle tone and spasm; these ef-fects are noted mostly in superficial structures [4]. Cryo-therapy is thought to temporarily reduce pain by acting as a counterirritant stimulus, decreasing nociceptive input, and reducing muscle spasm; these effects are noted mostly in superficial structures [4].
Diagnostic testing required
A thorough medical history and physical examination are required to rule out the possibility of serious pathology related to CLBP before administering these interventions.
Indications and contraindications
These interventions are indicated for nonspecific, mechanical CLBP.
TENS, EMS, and IFC are contraindicated for use over the anterior cervical region, carotid sinuses, heart, transthoracic area, insensate skin, abdomen of a pregnant woman, with a cardiac pacemaker, implanted defibrillator, or any other implanted electrical device, during electrocardiogram test-ing or while operattest-ing diathermy devices, and for patients with venous or arterial thrombosis or thrombophlebitis[4].
US is contraindicated for use over malignant lesions, pregnant abdomens, plastic implants, hemorrhagic regions, cemented areas of prosthetic joints, ischemic regions, in-sensate areas, infected lesions, electronic implants (includ-ing neurostimulators), areas that have been exposed to radiotherapy within the past 6 months, fractures, epiphyseal growth plates in skeletally immature patients, thrombotic areas, orbits of the eyes, gonads, and spinal cord after laminectomy[4].
Superficial heat is contraindicated over regions of acute injury, inflammation, hemorrhagic areas, malignancy,
impaired sensation, thrombophlebitis, or abdomens of preg-nant women[4].
Applying cold is contraindicated with urticaria, cold intol-erance or hypersensitivity, Raynaud disease or phenomenon, cryoglobulinemia or paroxysmal cold hemoglobinuria, deep open wounds, regenerating peripheral nerves, areas of circulatory compromise or peripheral vascular disease, or areas of impaired somatosensory discrimination[4].
Evidence of efficacy
Review methods
The objective of this systematic review was to evaluate the efficacy of IFC, TENS, EMS, US, hot packs, and cold packs in the treatment of nonspecific or rheumatic CLBP (longer than 12 weeks) by updating a previous review on this topic [5]. Evidence from randomized controlled trials (RCTs) and controlled clinical trials were identified and synthesized using a systematic approach to literature search, study selec-tion, data extracselec-tion, and data synthesis, as recommended by the Cochrane Collaboration. Studies with mixed acute low back pain and CLBP were excluded, whereas mixed subacute low back pain and CLBP were included.
A structured literature search for RCTs was performed using the electronic databases MEDLINE, EMBASE, Cur-rent Contents, CINAHL, and the Cochrane Controlled Tri-als Register up to August 2006. In addition, the registries of the Cochrane Field of Rehabilitation and Related Therapies and the Cochrane Musculoskeletal Group and the Physio-therapy Evidence Database were searched. The references of all included trials were searched for relevant studies. Only trials published in French and English were selected. Trained reviewers independently appraised the titles and abstracts of the literature search using a checklist with defined selection criteria. Articles selected for inclusion (or for which reviewers were uncertain based on the abstract) were then independently assessed in full-text format. Using predetermined extraction forms, the reviewers independently noted population characteristics, details of the interventions, trial design, allocation concealment, and outcomes. A senior reviewer (SP) checked the lists of articles and the reason for inclusion or exclusion.
Generally, comparisons of two active interventions (head-to-head studies) were excluded. Some studies had several comparative groups, and only some of the group comparisons were eligible to be included. Subjects who received placebo, were untreated, or received routine conventional therapeutic approaches were acceptable control groups. Studies were in-cluded if concurrent interventions were provided to the ex-perimental and control groups. However, studies where the patient acts as his or her own control were excluded. Cross-over studies were included, but only the data before the first crossing were analyzed to avoid potential confounders.
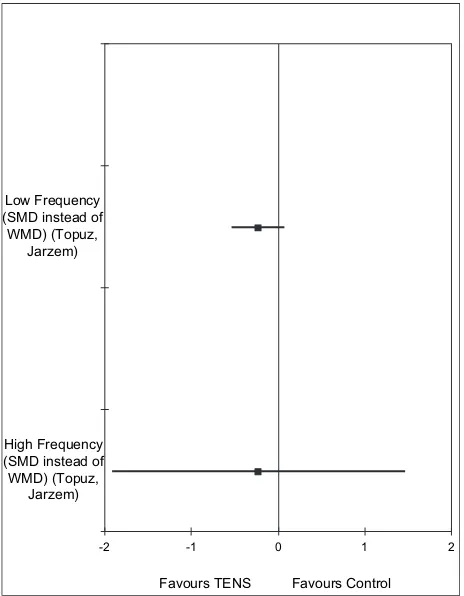
differences between the intervention and control groups at the end of the study. Dichotomous data were analyzed using relative risks. Meta-analyses were performed when contra-dictions were found in study results, when possible (similar population, outcome, intervention, and study design). Het-erogeneity between studies was tested using the chi-square statistic. We tested data heterogeneity among the results of different included studies to make sure that only homoge-neous data were pooled together. When heterogeneity was not significant, fixed-effect models were used. Random-effects models were used when heterogeneity was signifi-cant. Figures were created using Cochrane Collaboration methodology. The horizontal line represents the standard de-viation of the weighted mean difference for a specific out-come of interest. If the standard deviation line touches the central vertical line of the graph, the confidence interval is 0 and the difference between the two groups is not
statistically significant. Level of significance was set at p!.05 for all analyses.
To determine clinical improvement, the absolute benefit and relative difference in the change from baseline were cal-culated. Absolute benefit was calculated as the improvement in the treatment group less the improvement in the control group, maintaining the original units of measurement. Rela-tive difference was calculated as the absolute benefit divided by the baseline mean (weighted for the intervention and con-trol groups). For dichotomous data, the relative percentage of improvement was calculated as the difference in the percentage of improvement between the intervention and control groups. For meta-analyses, the pooled relative differ-ence was calculated by weighting the relative differdiffer-ence of each study with its sample size.
The recommendations were graded by the strength of evidence (Table 1). Outcomes of interest were pain,
Table 1
Details of the evidence grading system
Recommended (A) Evidence from two or more RCTs of a statistically significant, clinically important benefit (O15%) Recommended (Bþ) Evidence from only one RCT of a statistically significant, clinically important benefit (O15%) Recommended (B) Evidence from one or more CCTs of a statistically significant, clinically important benefit (O15%) Recommended (B) Evidence of clinical importance (O15%) but not statistical significance
Not recommended (C) Evidence from one or more CCTs of no clinically important difference and no statistical significance Not recommended (D) Evidence from one or more RCTs of no clinically important difference and no statistical significance Not recommended (E) Evidence from one or more RCTs of a statistically significant, benefit favoring the control group
RCT5randomized controlled trial; CCT5controlled clinical trials.
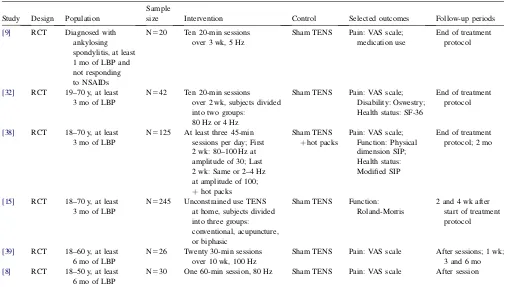
Table 2
Characteristics of included studies for TENS
Study Design Population
Sample
size Intervention Control Selected outcomes Follow-up periods
[9] RCT Diagnosed with ankylosing spondylitis, at least 1 mo of LBP and not responding to NSAIDs
N520 Ten 20-min sessions over 3 wk, 5 Hz
Sham TENS Pain: VAS scale; medication use
End of treatment protocol
[32] RCT 19–70 y, at least 3 mo of LBP
N542 Ten 20-min sessions over 2 wk, subjects divided into two groups:
80 Hz or 4 Hz
Sham TENS Pain: VAS scale; Disability: Oswestry;
N5125 At least three 45-min sessions per day; First 2 wk: 80–100 Hz at amplitude of 30; Last 2 wk: Same or 2–4 Hz at amplitude of 100; þhot packs
N5245 Unconstrained use TENS at home, subjects divided into three groups:
N526 Twenty 30-min sessions over 10 wk, 100 Hz
Sham TENS Pain: VAS scale After sessions; 1 wk; 3 and 6 mo [8] RCT 18–50 y, at least
6 mo of LBP
N530 One 60-min session, 80 Hz Sham TENS Pain: VAS scale After session
perceived disability, ability to work, patient satisfaction with treatment, health status, and medication use. Scales demonstrated to be valid and responsive to change were required to support a recommendation.
The search identified 36 potential articles on electrother-apeutic modalities and physical agents for CLBP[7–42], of which 6 were included in the analysis [8,9,15,32,38,39] (Table 2). Reasons for exclusion are noted inTable 3.
Systematic reviews
A Cochrane review on TENS for CLBP pain [43] ex-cluded two of the studies summarized below [9,39], did not have access to two subsequently published trials[15,32], and concluded there was a lack of studies to elaborate recommendations.
Randomized controlled trials
Transcutaneous electrical nerve stimulation. Six RCTs were identified [8,9,15,32,38,39] (Table 2). Number and length of treatment sessions varied among studies, as did TENS parameters. All studies included a form of control group, mostly consisting of sham TENS. The two types of TENS frequency parameters were used in the studies:
low frequency/acupuncture or high frequency. Apart from minor skin irritations suffered by a minority of subjects in one study [38], no complications related to TENS use were noted. Results are presented according to the assess-ment period and the frequency parameter used.
Immediately after TENS session. A clinically important and statistically significant reduction in pain intensity was seen in the two trials that assessed pain immediately after a high-frequency TENS session[8,39].
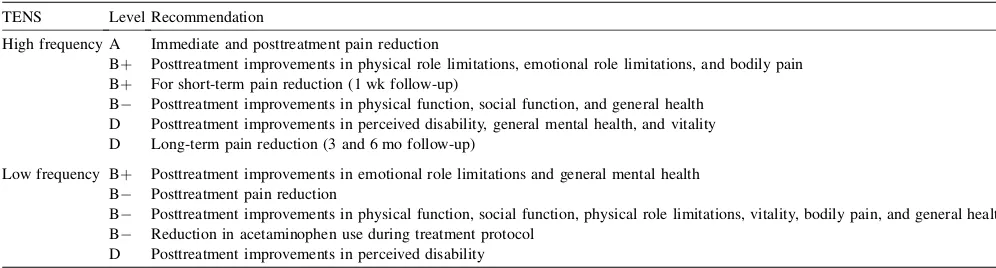
After the intervention protocol. Because contradictory results were found among the four studies that assessed this period [9,15,32,38], meta-analyses were performed when possible. The study that used both frequency parameters was included in both sections, but perceived disability and health status results were excluded from the meta-analyses because subjects appeared much less disabled than in the other studies. This study found no clinical or statistical differ-ences in these outcomes after the intervention protocol[38]. High-frequency TENS. A clinically important and statisti-cally significant reduction in pain intensity was obtained in the pooled result of the trials that assessed pain after the TENS protocol [32](Fig. 1). However, there were no clinical or statistically significant differences in the pooled result of perceived disability[15,32](Fig. 2). As for health status, a study found the following results: clinically impor-tant and statistically significant improvements in physical role limitations, emotional role limitations, and bodily pain;
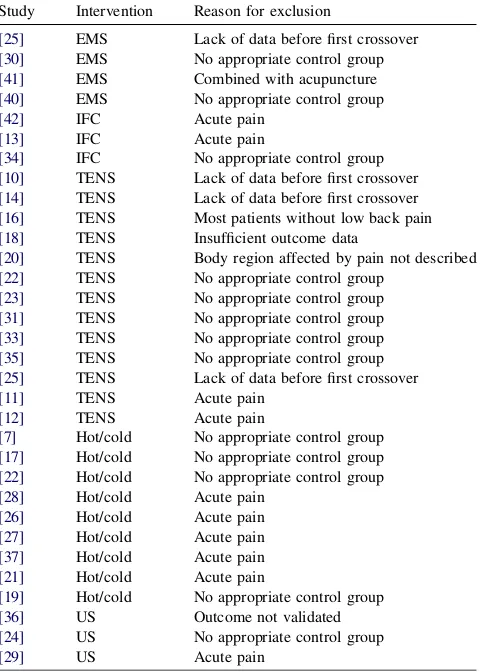
Table 3
Excluded studies and reason for exclusion
Study Intervention Reason for exclusion
[25] EMS Lack of data before first crossover [30] EMS No appropriate control group
[41] EMS Combined with acupuncture
[40] EMS No appropriate control group
[42] IFC Acute pain
[13] IFC Acute pain
[34] IFC No appropriate control group [10] TENS Lack of data before first crossover [14] TENS Lack of data before first crossover [16] TENS Most patients without low back pain [18] TENS Insufficient outcome data
[20] TENS Body region affected by pain not described [22] TENS No appropriate control group
[23] TENS No appropriate control group [31] TENS No appropriate control group [33] TENS No appropriate control group [35] TENS No appropriate control group [25] TENS Lack of data before first crossover
[11] TENS Acute pain
[12] TENS Acute pain
[7] Hot/cold No appropriate control group [17] Hot/cold No appropriate control group [22] Hot/cold No appropriate control group
[28] Hot/cold Acute pain
[26] Hot/cold Acute pain
[27] Hot/cold Acute pain
[37] Hot/cold Acute pain
[21] Hot/cold Acute pain
[19] Hot/cold No appropriate control group
[36] US Outcome not validated
[24] US No appropriate control group
[29] US Acute pain
EMS5electrical muscle stimulation; IFC5interferential current; TENS5transcutaneous electrical nerve stimulation; US5ultrasound.
-15 -10 -5 0 5
Low Frequency (Topuz, Gemignani, Deyo)
High Frequency (Topuz, Deyo)
Favours TENS Favours Control
clinically important improvements without statistical sig-nificance in physical function, social function, and general health; no clinical or statistical differences in general men-tal health and vimen-tality[32].
Low-frequency TENS. There was a clinically important improvement without statistical significance in the pooled result of pain intensity [9,32,38] (Fig. 1). There were no clinical or statistically significant differences in the pooled result of perceived disability[15,32](Fig. 2). As for health status, a study found the following results: clinically impor-tant and statistically significant improvements in emotional role limitations and general mental health; clinically impor-tant improvement without statistical significance in physi-cal function, social function, physiphysi-cal role limitations, vitality, bodily pain, and general health [32]. Although not significant, the study that assessed medication found a clinically important reduction in acetaminophen use during the TENS protocol[9].
Short-term follow-up. A clinically important and statisti-cally significant reduction in pain intensity was seen in the trial that assessed the short-term impact of high-frequency TENS (1 week follow-up)[39].
Long-term follow-up. No statistically significant difference or clinically important benefit was observed in the study that assessed the long-term pain impact of high-frequency TENS (3 and 6 months follow-up)[39]. The study that as-sessed long-term perceived disability (2 months follow-up)
reported no statistically significant difference, although no data were provided by the authors[38].
Interferential current. No eligible studies were found on which to base recommendations for IFC.
Electrical muscle stimulation. No eligible studies were found on which to base recommendations EMS.
Ultrasound. No eligible studies were found on which to base recommendations for US.
Hot/cold packs/ice. No eligible studies were found on which to base recommendations for hot packs, cold packs or ice.
Harms
Although infrequent, skin irritations can occur with the use of electrotherapeutic modalities and physical agents. Rarely, skin burns are associated with the inappropriate use of these interventions, such as prolonged continuous use, incorrect placement, or settings.
Summary
Although electrotherapeutic modalities and physical agents are frequently used in the management of CLBP, few studies were found to support their use. Most of the in-cluded studies on TENS can be considered of relatively poor methodological quality, with four [8,9,32,39] of the six scoring 2 or below on the Jadad scale[44]. Power cal-culations were not reported in any study. Variations in the number, length, and parameters of TENS sessions make comparisons difficult. Globally, high– and low-frequency TENS appears to have an immediate impact on pain inten-sity, with results favoring high-frequency TENS. TENS also appears to improve in the short-term pain, certain health status dimensions, and acetaminophen use, although these results come from only one trial each. Caution should be taken with the health status dimensions results, because the risks of a type 1 error are increased by the multiplicity of statistical tests used in the study. TENS does not appear to have an impact on perceived disability or long-term pain. Contradictory postintervention results (two studies re-ported mostly positive outcomes [9,32] and two mainly negative ones [15,38]) could be explained by differences in assessment periods. It is possible that the outcomes of the positive studies were assessed immediately after the last TENS session, making these outcomes not short term but immediate ones. We contacted the author of one of the positive studies, who informed us that the outcomes were indeed measured right after the last TENS session[32]. In the two negative result studies, delays in outcome mea-surement were quite probable, with TENS being used at home and evaluations accomplished at the clinic. This
-2 -1 0 1 2
Low Frequency (SMD instead of WMD) (Topuz,
Jarzem)
High Frequency (SMD instead of WMD) (Topuz,
Jarzem)
Favours TENS Favours Control
reinforces the notion that TENS appears to have immedi-ate impacts, but questions its short-term impact. Results of these studies suggest that TENS should probably be used as an adjunct tool for immediate to short-term pain relief, with no impact on perceived disability or long-term pain. Thus, although TENS appears to immediately reduce pain, its repercussions in overall management of CLBP are not well known. Given the preceding study results, clinical recommendations are summarized in Table 4.
One interesting observation of this review is that high-frequency TENS appears to be more effective on pain in-tensity when compared with low frequency, but this has to be confirmed in future comparative trials. Questions that remain on the implications of TENS use in the clinical management of CLBP include 1) Does the addition of TENS improve patient satisfaction with overall treatment? 2) Is TENS effective in reducing pain when taking analge-sics? 3) What are the consequences of long-term TENS use? 4) Is TENS effective in reducing pain with long-term users? 5) Does TENS use increase fear-avoidance behav-iors in patients by focusing treatment on pain? and 6) What is the cost effectiveness of TENS when compared with tra-ditional over-the-counter pain medication? It is also not known if adding TENS to an evidence-based intervention, such as exercise, improves even more outcomes. However, one of the studies did assess the interactions between exer-cise and TENS and found no cumulative impact, but it did not provide data on this[38].
Acknowledgments
We would like to thank Ms Natalie Morris and Mr. Michael Del Rio for their help in literature search, data extraction, and analysis.
References
[1] Poitras S, Blais R, Swaine B, Rossignol M. Management of work-related low back pain: a population-based survey of physical therapists. Phys Ther 2005;85:1168–81.
[2] Mikhail C, Korner-Bitensky N, Rossignol M, Dumas JP. Physical therapists’ use of interventions with high evidence of effectiveness in the management of a hypothetical typical patient with acute low back pain. Phys Ther 2005;85:1151–67.
[3] Guide to Physical Therapist Practice. Part 1: A description of pa-tient/client management. Part 2: Preferred practice patterns. Ameri-can Physical Therapy Association. Phys Ther 1997;77:1160–656. [4] Allen RJ. Physical agents used in the management of chronic pain by
physical therapists. Phys Med Rehabil Clin N Am 2006;17:315–45. [5] Philadelphia Panel evidence-based clinical practice guidelines on selected rehabilitation interventions for low back pain. Phys Ther 2001;81:1641–74.
[6] Review Manager (RevMan). [computer program]. Copenhagen: Nordic Cochrane Centre; 2006.
[7] Beyerman KL, Palmerino MB, Zohn LE, Kane GM, Foster KA. Efficacy of treating low back pain and dysfunction secondary to osteoarthritis: chiropractic care compared with moist heat alone. J Manipulative Physiol Ther 2006;29:107–14.
[8] Cheing GL, Hui-Chan CW. Transcutaneous electrical nerve stimula-tion: nonparallel antinociceptive effects on chronic clinical pain and acute experimental pain. Arch Phys Med Rehabil 1999;80:305–12. [9] Gemignani G, Olivieri I, Ruju G, Pasero G. Transcutaneous electrical
nerve stimulation in ankylosing spondylitis: a double-blind study. Arthritis Rheum 1991;34:788–9.
[10] Ghoname EA, Craig WF, White PF, et al. Percutaneous electrical nerve stimulation for low back pain: a randomized crossover study. J Am Med Assoc 1999;281:818–23.
[11] Herman E, Williams R, Stratford P, Fargas-Babjak A, Trott M. A randomized controlled trial of transcutaneous electrical nerve stimu-lation (CODETRON) to determine its benefits in a rehabilitation program for acute occupational low back pain. Spine 1994;19: 561–8.
[12] Hsieh RL, Lee WC. One-shot percutaneous electrical nerve stimula-tion vs. transcutaneous electrical nerve stimulastimula-tion for low back pain: comparison of therapeutic effects. Am J Phys Med Rehabil 2002;81: 838–43.
[13] Hurley DA, Minder PM, McDonough SM, Walsh DM, Moore AP, Baxter DG. Interferential therapy electrode placement technique in acute low back pain: a preliminary investigation. Arch Phys Med Rehabil 2001;82:485–93.
[14] Jarzem P. Transcutaneous electrical nerve stimulation [TENS] for short-term treatment of low back pain-randomized double blind crossover study of sham versus conventional TENS. J Musculoskelet Pain 2005;13:11–7.
[15] Jarzem PF, Harvey EJ, Arcaro N, Kaczorowski J. Transcutaneous electrical nerve stimulation [TENS] for chronic low back pain. J Musculoskelet Pain 2005;13:3.
Table 4
Recommendations for TENS use in chronic low back pain
TENS Level Recommendation
High frequency A Immediate and posttreatment pain reduction
Bþ Posttreatment improvements in physical role limitations, emotional role limitations, and bodily pain Bþ For short-term pain reduction (1 wk follow-up)
B Posttreatment improvements in physical function, social function, and general health D Posttreatment improvements in perceived disability, general mental health, and vitality D Long-term pain reduction (3 and 6 mo follow-up)
Low frequency Bþ Posttreatment improvements in emotional role limitations and general mental health B Posttreatment pain reduction
B Posttreatment improvements in physical function, social function, physical role limitations, vitality, bodily pain, and general health B Reduction in acetaminophen use during treatment protocol
D Posttreatment improvements in perceived disability
[16] Jeans ME. Relief of chronic pain by brief, intense transcutaneous electrical stimulation: a double blind study. Adv Pain Res Ther 1979;3:601–6.
[17] Landen BR. Heat or cold for the relief of low back pain? Phys Ther 1967;47:1126–8.
[18] Lehmann TR, Russell DW, Spratt KF, et al. Efficacy of electroacu-puncture and TENS in the rehabilitation of chronic low back pain patients. Pain 1986;26:277–90.
[19] Lidstrom A, Zachrisson M. Physical therapy on low back pain and sci-atica. An attempt at evaluation. Scand J Rehabil Med 1970;2:37–42. [20] Lundeberg T. Long-term results of vibratory stimulation as a pain
relieving measure for chronic pain. Pain 1984;20:13–23.
[21] Mayer J, Ralph L, Look M, et al. Treating acute low back pain with continuous low-level heat wrap therapy and/or exercise: a randomized controlled trial. Spine J 2005;5:395–403.
[22] Melzack R, Jeans ME, Stratford JG, Monks RC. Ice massage and transcutaneous electrical stimulation: comparison of treatment for low-back pain. Pain 1980;9:209–17.
[23] Melzack R, Vetere P, Finch L. Transcutaneous electrical nerve stim-ulation for low back pain. A comparison of TENS and massage for pain and range of motion. Phys Ther 1983;63:489–93.
[24] Mohseni-Bandpei MA, Critchley J, Staunton T, Richardson B. A pro-spective randomised controlled trial of spinal manipulation and ultra-sound in the treatment of chronic low back pain. Physiotherapy 2006;92:34–42.
[25] Moore SR, Shurman J. Combined neuromuscular electrical stimula-tion and transcutaneous electrical nerve stimulastimula-tion for treatment of chronic back pain: a double-blind, repeated measures comparison. Arch Phys Med Rehabil 1997;78:55–60.
[26] Nadler SF, Steiner DJ, Erasala GN, et al. Continuous low-level heat wrap therapy provides more efficacy than ibuprofen and acetamino-phen for acute low back pain. Spine 2002;27:1012–7.
[27] Nadler SF, Steiner DJ, Petty SR, Erasala GN, Hengehold DA, Weingand KW. Overnight use of continuous low-level heatwrap ther-apy for relief of low back pain. Arch Phys Med Rehabil 2003;84: 335–42.
[28] Nadler SF, Steiner DJ, Erasala GN, Hengehold DA, Abeln SB, Weingand KW. Continuous low-level heatwrap therapy for treating acute nonspecific low back pain. Arch Phys Med Rehabil 2003;84: 329–34.
[29] Nwuga VC. Ultrasound in treatment of back pain resulting from pro-lapsed intervertebral disc. Arch Phys Med Rehabil 1983;64:88–9. [30] Pope MH, Phillips RB, Haugh LD, Hsieh CY, MacDonald L,
Haldeman S. A prospective randomized three-week trial of spinal manipulation, transcutaneous muscle stimulation, massage and corset in the treatment of subacute low back pain. Spine 1994;19:2571–7.
[31] Sherry E, Kitchener P, Smart R. A prospective randomized controlled study of VAX-D and TENS for the treatment of chronic low back pain. Neurol Res 2001;23:780–4.
[32] Topuz O, Ozfidan E, Ozgen M, Ardic FO. Efficacy of transcutaneous electrical nerve stimulation and percutaneous neuromodulation ther-apy in chronic low back pain. J Back Musculoskeletal Rehabil 2004;17:127–33.
[33] Tsukayama H, Yamashita H, Amagai H, Tanno Y. Randomised con-trolled trial comparing the effectiveness of electroacupuncture and TENS for low back pain: a preliminary study for a pragmatic trial. Acupunct Med 2002;20:175–80.
[34] Werners R, Pynsent PB, Bulstrode CJ. Randomized trial comparing interferential therapy with motorized lumbar traction and massage in the management of low back pain in a primary care setting. Spine 1999;24:1579–84.
[35] Yokoyama M, Sun X, Oku S, et al. Comparison of percutaneous elec-trical nerve stimulation with transcutaneous elecelec-trical nerve stimula-tion for long-term pain relief in patients with chronic low back pain. Anesth Analg 2004;98:1552–6. [table].
[36] Roman MP. A clinical evaluation of ultrasound by use of a placebo technique. Phys Ther Rev 1960;40:649–52.
[37] Tao XG, Bernacki EJ. A randomized clinical trial of continuous low-level heat therapy for acute muscular low back pain in the workplace. J Occup Environ Med 2005;47:1298–306.
[38] Deyo R, Walsh N, Martin D, Schoenfeld L, Ramamurthy S. A controlled trial of transcutaneous electrical nerve stimulation and exercise for chronic low back pain. N Engl J Med 1990;322: 1627–34.
[39] Marchand S, Charest J, Li J, Chenard JR, Lavignolle B, Laurencelle L. Is TENS purely a placebo effect? A controlled study on chronic low back pain. Pain 1993;54:99–106.
[40] Glaser JA, Baltz MA, Nietert PJ, Bensen CV. Electrical muscle stim-ulation as an adjunct to exercise therapy in the treatment of nonacute low back pain: a randomized trial. J Pain 2001;2:295–300. [41] Hamza MA, Ghoname EA, White PF, et al. Effect of the duration of
electrical stimulation on the analgesic response in patients with low back pain. Anesthesiology 1999;91:1622–7.
[42] Hurley DA, McDonough SM, Dempster M, Moore AP, Baxter GD. A randomized clinical trial of manipulative therapy and interferential therapy for acute low back pain. Spine 2004;29:2207–16.
[43] Khadilkar A, Milne S, Brosseau L, et al. Cutaneous electrical nerve stimulation (TENS) for chronic low-back pain. Cochrane Database Syst Rev 2005;20. CD003008.