Pharmacology is simply defined as the study of drugs. Pharmacology can also be defined as the study of substances that interact with living systems through chemical processes, especially by binding to regulatory molecules and activating or inhibiting normal body processes. These substances are generally known as drugs. Drugs as we know including any substances that bring about a change in biologic function through its chemical actions or produce effect on living organism. According to definition from the Indonesian Ministry of Health, drugs included not only any substances that used for treating diseases, but also substances for preventing diseases and for confirming diagnosis of such diseases. These substances commonly produce more than one effect, it can be beneficial therapeutic effects or, in the other hand, undesirable effects on living systems (adverse or toxic effects). All substances (drugs) can be toxic under certain circumstances.
Pharmacology refers to a very broad area of study. Pharmacokinetics and pharmacodynamics are two basic subject area of pharmacology. Pharmacokinetics concern about the actions of the body on drug or the fate of drug in our body, including absorption, distribution, metabolism, and elimination; whereas pharmacodynamics concern about the action of drug in our body, including receptor interaction, as well as mechanism of therapeutic and toxic action.
In this block, we will learn about the basic concept of pharmacology, including drug development and regulation, drug category, drug pharmacokinetics, drug pharmacodynamics, drug interaction, adverse drug effects, and rational drug use, as well as some basic concepts of several important drugs including drugs act on autonomic nervous system, antibiotics and analgesic antiinflammation.
This block will take 10 meeting to be completed, each meeting consist of introductory lecture continued by independent learning, small group discussion (SGD), ending with plenary session. In each topic there will be a list of tasks to discuss on SGD which some of them are based on a case that commonly find in clinical practice. There will also a student project assignment that should be fulfilled by all students in group. Each group will be given one topic for student project and this has to be presented at the end of block based on schedule. There will be also practical session related to basic pharmacology.
Evaluation in this block will be formative and summative. The formative evaluation is directive and will take as checklist and peer assessment, while summative will be conducted at the end of this block.
We believe that the basic of pharmacology that you will learn in this block will impulse you to learn more about it to help you managing patients in your next clinical practice.
Good luck,
Planner team
No
List
Page
no.
1. Cover
2. Preface 1
3. List of Content 2
4. Planners and Lecturers Team 3
5. Facilitators 4
6. Curriculum Block: Basic Pharmacology 5
7. Time Table 6
8. Meeting of Student Representatives 8
9. Student Project 8
10. Assessment Method 9
11. References 9
12. Content Outline and Learning Task 10
13. Guideline for Practical Session 17
14. Curriculum Map 22
PLANNERS AND LECTURERS
No. NAME DEPARTEMENT PHONE
1. dr. I Gusti Ayu Artini, M.Sc. (Head) Pharmacology 08123650481 2. Desak Ketut Ernawati, S.Si, Apt, M.Pharm.
(Secretary)
Pharmacology 081236753646
3. dr. Agung Nova Mahendra, M.Sc. Pharmacology 087861030195
4. Prof. dr. IGM Aman, SpFK Pharmacology 081338770650
5. Dr. dr. I Made Jawi, M.Kes. Pharmacology 08179787972
2. LIST OF CONTENT
6. Dr. dr. BK Satriyasa, M.Repro Pharmacology 081237166686
7. dr. Ida Bagus Ngurah, M.FOr Pharmacology 08123687288
REGULAR CLASS
NO NAME GROUP DEPT PHONE ROOM
1 Dr.dr. I Made Jawi, M.Kes A1 Pharmacology 08179787972 2nd floor: R.2.01 2 dr. Ni Ketut Putri Ariani, Sp.KJ A2 Psychiatry 082237817384 2R.2.02nd floor:
3 dr. IGA Ratnayanti, M.Biomed A3 Histology 085104550344 2nd floor: R.2.03 4 dr. I B Darma Putra,
Sp.B-KBD A4 Surgery 08123600552
2nd floor: R.2.04 5 dr. I Gde Haryo Ganesha, S.Ked A5 DME 081805391039 2R.2.05nd floor:
6 dr. Gusti Ngurah Mayun,
Sp.HK A6 Histology 08155715359
2nd floor: R.2.06 7 dr. I Ketut Wibawa Nada,
Sp.An A7 Anasthesi 087860602995
2nd floor: R.2.07 8 dr. I Wayan Weta, MS, Sp.GK A8 Public Health 081337003560 2R.2.08nd floor:
9 dr. Muliani, M.Biomed A9 Anatomy 085103043575 2R.2.21nd floor: 10 dr. Putu Patriawan, Sp.Rad, A10 Radiology 08123956636 2nd floor:
MSc R.2.22
ENGLISH CLASS
NO NAME GROUP DEPT PHONE ROOM
1 dr. I Wayan Surudarma, M.Si B1 Biochemistry 081338486589 2
nd floor: R.2.01
2 dr. I Wayan Losen Adnyana, Sp PD B2 Interna 08123995536 2R.2.02nd floor:
3 Dr. dr. Sianny Herawati, Sp.PK B3 Clinical
Pathology 081236172840
2nd floor: R.2.03
4 dr. Yuliana, M.Biomed B4 Anatomy 085792652363 2nd floor:
R.2.04 5 dr. Made Agus Hendrayana , M.Ked B5 Microbiology 08123921590 2R.2.05nd floor:
6 dr. I Nyoman Semadi, Sp.B, Sp.BTKV B6 Surgery 08123838654 2R.2.06nd floor:
7 dr. I Wayan Eka Sutyawan,
Sp.M B7 Opthalmology 081338538499
2nd floor: R.2.07 8 dr. Kadek Budi Santosa, Sp.U B8 Surgery 081339977799 2R.2.08nd floor:
9 dr. Sri Laksminingsih Sp. Rad B9 Radiology 08164745561 2R.2.21nd floor:
10 dr. I Gede Suwedagatha, Sp.B
(K) Trauma B10 Surgery 0811387720
2nd floor: R.2.22
LEARNING OUTCOME
1. Comprehend the basic concept of pharmacology including concept of drug pharmacokinetics and pharmacodynamics.
2. Comprehend the process of drug development. 3. Comprehend the principle of drug interaction. 4. Comprehend the principle of rational drug use.
5. Comprehend the basic concept of pharmacology for some drugs used in many system disorders (autonomic drugs, antibiotics and analgesics antiinflammation).
LEARNING OBJECTIVE
1. Describe the concept of drug pharmacokinetics. 2. Describe the concept of drug pharmacodynamics. 3. Define the process of drug development.
4. Identify the classification of drug. 5. Define the principle of drug interaction. 6. Define the principle of rational drug use.
7. Describe the concept of pharmacology for autonomic drugs. 8. Describe the concept of pharmacology for antibiotics.
9. Describe the concept of pharmacology for analgesics antiinflammation.
LEARNING STRATEGY
:
Introductory Lecture
Independent learning
Small group discussion
Plenary Session
Practical session
Student project
REGULAR CLASS
DAY/
DATE TIME ACTIVITY CONVEYER VENUE
1
Lecture 1 : Introduction to Pharmacology Lecture 2 : Drug Development and Regulation
Independent Learning
Lecture 3 : Drug Pharmacokinetics 1 Lecture 4 : Drug Pharmacokinetics 2
Practical session 1 (A1-A5)
Lecture 5 : Drug Pharmacodynamics 1 Lecture 6 : Drug Pharmacodynamics 2
SGD
5 Lecture 10 : Antibacterial Drugs
Independent learning
Lecture 11 : Analgesic antiinflammation Lecture 12 : Drug Interaction
SGD
Lecture 13 : Adverse Drug Reaction Lecture 14 : Rational Drug Use
Independent Learning
7 April 2016 08.00 – 16.00 Student Project Presentation Team Class R.
9
Friday
8 April 2016 SILENT DAY
10
Monday 11 April 2016
09.00 – 13.00 FINAL EXAM
LB / Internet
Lecture 1 : Introduction to Pharmacology Lecture 2 : Drug Development and Regulation
BREAK
Lecture 3 : Drug Pharmacokinetics 1 Lecture 4 : Drug Pharmacokinetics 2
BREAK
Lecture 5 : Drug Pharmacodynamics 1 Lecture 6 : Drug Pharmacodynamics 2
BREAK
Lecture 7 : Drugs act on Autonomic Nervous System (ANS) 1 Lecture 10 : Antibacterial Drugs
6
Lecture 11 : Analgesic antiinflammation Lecture 12 : Drug Interaction
BREAK
Lecture 13 : Adverse Drug Reaction Lecture 14 : Rational Drug Use
BREAK
7 April 2016 08.00 – 16.00 Student Project Presentation Team Class R.
9
Friday
8 April 2016 SILENT DAY 10
Monday 11 April 2016
09.00 – 13.00 FINAL EXAM LB / Internet
R.
Introductory Lecture, Plenary and Student Project Presentation will be held at Class Room 402; Practical Session at Laboratory of Pharmacology (2nd floor) and Pharmacy (1st floor); Discussion Rooms available at 2nd floor (Room 2.01-2.08 & 2.21-2.22).
In the middle of block schedule, a meeting is designed among the student representatives of each small group discussion, facilitators, and lecturers. The meeting will discuss the ongoing teaching learning process, quality of lecturers and facilitators as a feedback to improve the learning program. The meeting will be held based on schedule from Department of Medical Education.
Each group should write a paper (article review) about certain topics related to basic pharmacology. This paper should be discussed with the related lecturer and would be presented/ collected at the end of this block.
The topics are:
NO SGD TOPIC EVALUATOR
1 A1, B1 Pharmacokinetic changes in renal disorders Prof. Aman 2 A2, B2 Signal transduction for intracellular drug
receptor
Dr. Jawi
MEETING OF THE STUDENT REPRESENTATIVES
3 A3, B3 Signal transduction for G-protein coupled drug receptor
Dr. Jawi
4 A4, B4 Drug interaction dr. Ngurah
5 A5, B5 Antibiotic resistance Dr. Satriyasa
6 A6, B6 Drug allergy Dr. Satriyasa
7 A7, B7 Irrational prescription in geriatric patient dr. Artini
8 A8, B8 Self medication with antibiotics dr. Artini
9 A9, B9 Aplication of ANS drug for asthma dr. Nova
10 A10,B10 Aplication of ANS drug for cardiovascular disorders
dr. Nova
Format for Student Project Paper
Student project paper should be written in 5-10 pages of A4 paper with 1.5 spacing and font Times New Romance size 12. The general format is similar to format for elective study paper.
The Format is: 1. Cover
Tittle
Name
Student Registration Number
Faculty of Medicine Udayana University
2016 2. Introduction
3. Content 4. Conclusion
5. References (minimal 3 references, should mostly from journal and textbook or other valid sources that published not older than 10 years)
Example how to write references : Journal
Porrini M, Risso PL. 2011. Lymphocyte Lycopene Concentration and DNA Protection from Oxidative Damage is Increased in Woman. Am J Clin Nutr 11(1):79-84.
Abbas AK, Lichtman AH, Pober JS. 2011. Cellular and Molecular Immunology. 4th ed. Pennysylvania: WB Saunders Co. Pp 1636-1642.
Assessment in this block consists of:
SGD : 5%
Final Exam : 80%
Student Project : 15%
Total result will contribute as much as 40 % to overall score of Medical Communication Block
Final exam will be carried out at the end of block using Multiple Choice Questions (MCQ) type. The minimal passing score for the assessment is 70. Every student should pass the minimum passing score for both Medical Communication and Basic Pharmacology Block.
The requirement for taking the final exam: - join 75% of total student activities - bring student ID card with photo
1. Katzung BG, Masters SB, Trevor AJ. 2012. Basic and Clinical Pharmacology. 12th ed. New York: McGraw Hill.
2. Trevor AJ, Katzung BG, Masters SB. 2005. Pharmacology Examination and Board Review. 7th ed. New York: McGraw Hill.
3. Brunton LL and Parker KL. 2008. Goodman and Gilman’s Manual of Pharmacology and Therapeutics. New York: McGraw Hill.
4. Lullman H, Mohr K, Hein L, Bieger D. 2005. Color Atlas of Pharmacology. 3rd ed. New York: Thieme Stutgart.
5. Hitner H and Nagle B. 2002. Glencoe Basic Pharmacology. 4th ed. New York: McGraw Hill.
9. ASSESSMENT METHOD
Pharmacology is defined as the study of substances that interact with living systems through chemical processes, especially by binding to regulatory molecules and activating or inhibiting normal body processes. These substances commonly known as drugs. Drugs might produce more than one effect, beneficial therapeutic effects or, in the other hand, undesirable effects on living systems (adverse or toxic effects). Pharmacology refers to a very broad area of study. Pharmacokinetics and pharmacodynamics are two basic subject area of pharmacology.
There are several sources of drugs, including plant, animal, microorganism and chemical synthesis. Drug candidates undergo several tests for screening their pharmacologic profile and activity as well as their selectivity. The safety and efficacy of drugs must be defined before they can be marketed; therefore some preclinical pharmacologic and toxicity testing (including invitro and animal studies), as well as clinical study (phase 1 – 4) must be performed.
Many factors affecting the action of drug in our body including the route of drug administration (which is related to drug preparation or drug form), age, sex, weight, genetic variation, the presence of other disease or interaction with other drug (drug interaction). Drug interaction refers to the effects that occur when the actions of one drug are affected by another drug. Drug interaction might affect the pharmacokinetic or pharmacodynamics process of drug that subsequently affects the drug action or effect.
Related to the regulation of drug distribution in Indonesia, Indonesian Ministry of Health has already classified marketed drugs into five groups of drugs (free drug, limited free drug, hard drug, psychotropic drug and narcotics). Generally, in the world, drugs are divided into prescription and nonprescription drugs (over the counter drugs/ OTC drugs). Drugs can also be classified into patent drugs, generic drugs and branded generic drugs.
Vignete
A 25 years old woman came to public health center (PHC) complaining fever since 3 days ago. Patients also complained sore throat, cough, cold and headache. After doing anamnesis and physical examination, doctor decided to prescribe Demacolin® and Amoxsan® tablet.
Learning Task 1
1. What are the categories of those two drugs?
2. What are the advantages and disadvantages of this route of administration? 3. What processes undergone by such oral drug in our body?
Learning Task 2
A few hours later, patient came back to PHC complaining rash and itchy in her whole body. 1. What condition possibly happened to this patient?
2. What information should be given to the patient related to her condition?
11. CONTENT OUTLINE AND LEARNING TASK
The aim of studying pharmacokinetic is to understand the term that commonly used in pharmacology and the fate of drug in the body. The action of the body to drug is called pharmacokinetics, that are including absorption, distribution, metabolism and excretion of drug.
If the drug is given to patient, the first reaction of the body is absorption of the drug. The drug is absorbed from the site of administration, pass through the cell membrane. In blood or plasma part of drug will bound to protein especially albumin and orosomucoid, and the others are free. So in plasma there are two kind of drugs, free drug (unbound drug) and bound drug. Each drug have its specific protein bound (eg.warfarin, only 2 % in the form of free, while penicilline 50 % are bound). Only free drug will be distributed, produce effects, metabolized and excreted.
The very common route of administration is oral route, although absorption may be slower and less complete. Ingested drugs are subject to the first pass effect, in which a significant amount of drug is metabolized in the gut wall and the liver before the drug reaches the systemic circulation.
The drug then distributed to all part of the body and reaches its receptor to produce its effects. An important pharmacokinetic parameter that reflect of dug distribution is apparent volume of distribution (Vd). The bigger the value of Vd, the greatest amount of drugs distributed to body organ.
After distribution process the drug will be metabolized. Metabolism of drug sometimes terminate its action. The action of many drugs (eg.phenothiazine) is terminated before they are excreted, but prodrugs (eg.Levodopa) are inactive as administered and must be metabolized in the body to become active. The other drugs (eg.benzodiazepine) are active as administered and have active metabolites as well. On the other hand lithium is not metabolized by the body, so lithium still active in the body until it is excreted. Elimination is not the same with excretion of drug. Elimination means that an active drugs are metabolized to become inactive, although it metabolites are still in the body, and excreted means that molecules of drugs are excreted from the body. But for drugs that are not metabolized, excretion is the mode of elimination. For most drugs and it’s metabolites, excretion is primarily by kidney and intestine. Anesthetic gases are excreted primarily by the lungs.
Vignete
A 40 years old patient came to private practice doctor with complain of cough, wheezing, chest tightness and/or dyspnoea (breathlessness), which are often worse at night or early in the morning. The patient was diagnosed with Bronchial Asthma. Salbutamol (Beta 2 agonist) is given to patient.
Learning Task
1. Describe the definition of : Drug, Pharmacology, Pharmacokinetic, Pharmacodynamic, Volume of distribution (Vd), Half life (t ½ ), Bioavailability, Minimum Effective Concentration (MEC), Therapeutic window, First Pass Effect (Presystemic elimination), 2. Differentiate drug elimination and drug excretion, first order elimination and zero order
elimination.
3. Describe the fate of drug, if taken orally.
4. Name and discuss the common route of drugs administration.
Lecture 3-4. Drug Pharmacokinetics
Pharmacodynamics is the study of the biochemical and physiological effects of drugs on the body or on microorganisms or parasites within or on the body and the mechanisms of drug action and the relationship between drug concentration and effect. Pharmacodynamics is often summarized as the study of what a drug does to the body. Pharmacodynamics is sometimes abbreviated as "PD". The majority effect of drugs on the body either: (a) mimic or inhibit normal physiological/biochemical processes or inhibit pathological processes in animals or (b) inhibit vital processes of endo- or ectoparasites and microorganisms.
There are 7 main drug actions:
Stimulating action through direct receptor agonism and downstream effects
Depressing action through direct receptor agonism and downstream effects (ex.: inverse agonist)
Blocking/antagonizing action (as with silent antagonists), the drug binds the receptor but does not activate it
Stabilizing action, the drug seems to act neither as a stimulant or as a depressant (ex.: some drugs possess receptor activity that allows them to stabilize general receptor activation, like buprenorphine in opioid dependent individuals or aripiprazole in schizophrenia, all depending on the dose and the recipient)
Exchanging/replacing substances or accumulating them to form a reserve
Direct beneficial chemical reaction as in free radical scavenging
Direct harmful chemical reaction which might result in damage or destruction of the cells, through induced toxic or lethal damage (cytotoxicity or irritation)
The desired activity of a drug is mainly due to successful targeting of one several site/target of actions. The targets are c ellular membrane disruption, c hemical reaction with downstream effects, interaction with enzyme proteins, interaction with structural proteins, interaction with carrier proteins, interaction with ion channels, & l igand binding to receptors (h ormone receptors, n euromodulator receptors, & n eurotransmitter receptors).
In principle, a pharmacologist would aim for a target plasma concentration of the drug for a desired level of response. In reality, there are many factors affecting this goal. Pharmacokinetic factors determine peak concentrations, and concentrations cannot be maintained with absolute consistency because of metabolic breakdown and excretory clearance. Genetic factors may exist which would alter metabolism or drug action itself, and a patient's immediate status may also affect indicated dosage.
The therapeutic window is the amount of a medication between the amount that gives an effect (effective dose) and the amount that gives more adverse effects than desired effects. For instance, medication with a small pharmaceutical window must be administered with care and control, e.g. by frequently measuring blood concentration of the drug, since it easily loses effects or gives adverse effects.
The duration of action of a drug is the length of time that particular drug is effective. Duration of action is a function of several parameters including plasma half-life, the time to equilibrate between plasma and target compartments, and the off rate of the drug from its biological target.
Receptors are macromolecules involved in chemical signaling between and within cells; they may be located on the cell surface membrane or within the cytoplasm. Activated receptors directly or indirectly regulate cellular biochemical processes (e.g., ion conductance, protein phosphorylation, DNA transcription, enzymatic activity). Molecules (e.g., drugs, hormones, neurotransmitters) that bind to a receptor are called ligands. A ligand may activate or inactivate a receptor; activation may increase or decrease a particular cell function. Each ligand may interact with multiple receptor subtypes. Few, if any, drugs are absolutely specific for one receptor or subtype, but most have relative selectivity. Selectivity is the degree to which a drug acts on a given site relative to other sites; selectivity relates largely to physicochemical binding of the drug to cellular receptors.
to which a ligand activates receptors and leads to cellular response). A drug’s affinity and activity are determined by its chemical structure.
The pharmacologic effect is also determined by the duration of time that the drug-receptor complex persists (residence time). The lifetime of the drug-receptor complex is affected by dynamic processes (conformation changes) that control the rate of drug association and dissociation from the target. A longer residence time explains a prolonged pharmacologic effect. Drugs with long residence times include finasteride and darunavir. A longer residence time can be a potential disadvantage when it prolongs a drug's toxicity. For some receptors, transient drug occupancy produces the desired pharmacologic effect, whereas prolonged occupancy causes toxicity. Receptor up-regulation and down-regulation affect adaptation to drugs (e.g., desensitization, tachyphylaxis, tolerance, acquired resistance, postwithdrawal supersensitivity).
The structures of receptors are very diverse and can broadly be classified into the following categories:
1. Type 1: L (ionotropic-receptors) – These receptors are typically the targets of fast-neurotransmitters such as acetylcholine (nicotinic) and GABA; and, activation of these receptors results in changes in ion-movement across a membrane. They have a hetero-structure. Each subunit consists of the extracellular-ligand-binding domain and a transmembrane-domain where the transmembrane-domain in turn includes four transmembrane-alpha helixes. The ligand-binding cavities are located at the interface between the subunits.
2. Type 2: G protein-coupled receptors (metabotropic) – This is the largest family of receptors and includes the receptors for several hormones and slow transmitters e.g. dopamine, metabotropic-glutamate. They are composed of seven transmembrane-[alpha helix|alpha helices]]. The loops connecting the alpha-helices form extracellular and intracellular-domains. The binding-site for larger peptidic-ligands is usually located in the extracellular-domain whereas the binding-site for smaller non-peptidic ligands is often located between the seven alpha-helices and one extracellular-loop. The aforementioned receptors are coupled to different intracellular-effector systems via G-proteins.
3. Type 3: kinase linked and related receptors (see "r eceptor tyrosine kinase", and "e nzyme-linked receptor") - They are composed of an extracellular-domain containing the ligand-binding site and an intracellular-domain, often with enzymatic-function, linked by a single transmembrane-alpha helix. e.g. the insulin-receptor. 4. Type 4: nuclear receptors – While they are called nuclear-receptors, they are
actually located in the cytosol and migrate to the nucleus after binding with their ligands. They are composed of a C-terminal-ligand-binding region, a core- DNA-binding domain (DBD) and an N-terminal-domain that contains the AF1 (activation function 1) region. The core-region has two zinc-fingers that are responsible for recognizing the DNA sequences specific to this receptor. The N-terminal interacts with other cellular-transcription factors in a ligand-independent manner; and, depending on these interactions it can modify the binding/activity of the receptor. Steroid and thyroid-hormone receptors are examples of such receptors.
Ligands bind to precise molecular regions, called recognition sites, on receptor macromolecules. The binding site for a drug may be the same as or different from that of an endogenous agonist (hormone or neurotransmitter). Agonists that bind to an adjacent site or a different site on a receptor are sometimes called allosteric agonists. Nonspecific drug binding also occurs—ie, at molecular sites not designated as receptors (e.g., plasma proteins). Drug binding to such nonspecific sites, such as binding to serum proteins, prohibits the drug from binding to the receptor and thus inactivates the drug. Unbound drug is available to bind to receptors and thus have an effect.
1. Plasma concentration of the drug for a desired level of response are very important. In reality, there are many factors affecting this goal. Mention and explains each of its ! 2. Please explain about the concept of therapeutic window! Medication with a small
therapeutic window must be administered with care and control, e.g. by frequently measuring blood concentration of the drug. Why?
The autonomic nervous system (ANS) is the involuntary portion of the nervous system. The ANS consists of sympathetic (SANS) and parasympathetic nervous system (PANS). Both of these systems regulates many important bodily functions to maintain homeostasis, such as heart rate, blood pressure, and respiratory function. It involves neurotransmitters as it hallmark in regulating those functions. The synthesis, storage, release, receptor interaction, reuptake, and metabolism of the involved neurotransmitters can be modulated by many drugs. Hence, it is very important for undergraduate medical students to comprehend and master the knowledge of ANS pharmacology as a basis of rational therapy and good clinical practice.
Vignete
A man, 21 years old, accompanied by his parents, came to the emergency room of RSUP Sanglah complaining about breathing difficulty and dizziness. Those symptoms commenced about an hour after he took amoxicillin prescribed previously by a GP due to the diagnosis of upper respiratory tract infection. He said that he frequently take amoxicillin when he think that he get pharyngitis. He denied the history of drug allergy, but admitted that he has allergy to seafood. Physical examination revealed urticaria in both of the volar aspects of his lower arms, blood pressure of 80/50 mmHg, heart rate of 124 x/minute, breathing rate of 30 x/minute, wheezing on chest auscultation, and O2 saturation of 90%. The emergency physician diagnosed him with anaphylactic shock. After being administered with epinephrine injection, he showed dramatic clinical improvements. He was then hospitalized for 3 days for clinical observation and stabilization under the supervision of a clinical allergo-immunologist.
Learning Task
1. What receptors and neurotransmitters are involved in the pathomechanism of the case above? Please explain their functions!
2. Why does the emergency physician administer epinephrine, and not dopamine, when he treat the shock?
3. Please explain the neurotransmitter aspect of the SANS! 4. Please explain the neurotransmitter aspect of the PANS!
5. What are the steps in autonomic transmission? Please give an example of drug and its pharmacodynamics for each step!
Penicillins and chepalosporins are the major antibiotics that inhibit bacterial cell wall synthesis. They are called beta-lactams because of the unusual 4-member ring that is common to all their members. The beta-lactams include some of the most effective, widely used, and well-tolerated agents avaliable for the treatment of microbial infections. Vancomysin, fosfomycin, and bacitracin also inhibit cell wall synthesis but for various reasons are not nearly as important as the beta-lactams drugs. The Selective toxicyti of the drug discussed in this chapter is mainly due to specific actions on the synthesis of a cellular structure that is unique to the microorganism. More than 50 antibiotics that acts as cell wall
Lecture 7-9. Drug Act on Autonomic Nervous System
synthesis inhibitors are currently avaliable, with individual spectra of activity that afford a wide range of clinical applications.
The antimicrobial drugs reviewed in this chapter selectively inhibit bacterial protein synthesis. The mechanism of protein synthesis in microorganism are not identical to those of mammalian cells. Bacteria have 70S ribosomes, whereas mammalian sell have 80S ribosomes. Differences exist in ribosomal subunits and in the chemical composition and functional specificities of component nucleic acids and proteins. Such differences from the basis for the selective toxicity of these drugs against microorganisms without causing major effect on protein synthesis in mammalian cells.
Aminiglycosides are also capable of exerting a postantibiotic effect such that their killing action continues when their plasma levels have declined below measurable levels. Consequently, aminoglycosides have greater efficacy when administered as a single large dose than whwn given as multiple smaller doses. The toxicity (in contrast to the antibacterial efficacy ) of aminoglycosides depends both on critical plasma concentration and on the time that such a level is exceeded. The time above such a single large dose of an aminoglyciside than when multiple smaller doses are given. These concepts from the basis for once-daily aminoglycoside dosing protocols, which can be more effective and less toxic than traditional dosing regimens.
Sulfonamides and trimethoprim are antimetabolites selectively toxic to microorganisms because they interfere with folic asid synthesis. Sulfonamides continue to be used selectively as individual antimicrobial agents , altough resistance is common. The combination of a sulfonamide with trimethoprin causes a sequential blockade of folic acid synthesis. This results in a synergistic actions againts a wide 1Fluoroquinolons, which selectively inhibit microbial nucleic asid metabolism, also have a broad spectrum of antimicrobial activity that includes many common pathogens. Resistance has emerged to the older antibioticsin this class, but has been offset to some extent by the introduction of newer generations of fluoroquinolones with expanded activity against common pathogenic organism.
Learning Task
1. A 36- year-old woman recently treated for leukemia is admitted to the hospital with malaise, chills, and high fever. Gram stain of blood reveals the presence of gram-negative bacilli. The initial diagnosis is bacteremia, and parenteral antibiotics are indicated. The records of the patient reveal that she had a severe urticarial rash, hypotension, and respiratory difficulty after oral penicillin V about 6 mo ago. The most appropriate drug for empiric treatment is:
A. ampicillin plus sulbactam B. aztreonam
C. Cefazolin
D. imipenem plus cilastatin E. ticarcillin plus clavulanic acid
2. A 2-year-old child is brought to the hospital after ingesting pills that a parent had used for bacterial dysentery when traveling outside the United States. The child has been vimiting for more than 24 h and has had diarrhea with green stools. He is now lethargic with an ashen color. Other signs and symptoms include hypothermia, hypotention, and abdominal distention. The drug most likely to be the cause of this problem is:
3. A 24-year- old woman has primary syphilis. She has a history of penicillin hypersensitivity, so tetracycline will be used to treat the infection. Which one of the following statements about the proposed drug treatment of this patient is false ?
A. She will have to take the drug for 15 days
B. She should avoid taking antacids at the same time as she takes the drug C. She may experience anorexia and gastrointestinal distress
D. She should eat plenty of yogurt to prevent vaginal candidiasis E. She should call her physician if she develop severe diarrhea
4. A 31-year-old man has gonorrhea. He has no drug allergies, but a few years ago while in Afrika acute hemolysis followed use of an antimalarial drug. The physician is concerned that the patient has an accompanying urethritis caused by C trachomatis, although no cultures or enzyme tests have been perfomed. Which of the following drug is most likely to be effective against gono cocci and to eradicate C trachomatis in this patient?
A. Cefixime B. Ciprofloxacin C. Ofloxacin D. Spectinomycin E. Sulfamethoxazole
The treatment of patients with inflammation involves two primary goals: first, the relief of pain, which is often the presenting symptom and the major continuing complaint of the patient; and second, arrest of the tissue-damaging process.
Reduction of inflammation with nonsteroidal antiinflamatory drugs (NSAIDs) often results in relief of pain for signifificant periods. Furthermore, most of the non-opiod analgesics(aspirin, etc.) also have anti-inflammatory effects, so they are apppropriate for the treatment of both acute and chronic inflammatory conditions.
The glucocorticoids also have powerful anti-inflammatory effects and when first introduced were considered to be the ultimate answer to the treatment of antiinflammatory arthritis. Unfortunately, the toxicity associated with chronic corticosteroid therapy limits their use except in the control of acute flare-up of joint disease. Therefore, the nonsteroidal anti-inflammatory drugs have assumed a major role in the long term-term treatment of arthritis. Another important group of agents are characterized as slow-acting antirheumatic drugs (SAARDs) or disease-modifying antirheumatic drugs (DMARDs). They may slow the bone damage associated with rheumatoid arthritis and are thought to affect more basic inflammatory mechanism than do the NSAIDs.
Vignete
A 25-year-old woman presented with intense pain in her stomach. The physician diagnoses her with dysmenorrhea. Which of the following drugs is used in the treatment of dysmenorrhea?
A. Allopurinol B. Colchicine C. Leflunomide D. Naproxen E. Sulfinpyrazone
Learning Task
1. List NSAIDs, non-opioid analgesics and drugs used in gout!
2. Describe the mechanisms of action of anti-inflammatory drugs, non-opiod analgesics and drugs used in gout!
3. Describe the pharmacokinetics of anti-inflammatory drugs, non-opioid analgesics and drugs used in gout!
4. Describe the toxic effects of anti-inflammatory drugs, non-opioid analgesics and drugs used in gout!
5. Describe of the clinical uses of anti-inflammatory drugs, non-opioid analgesics and drugs used in gout!
6. Describe the advantages of the disease-modifying antirheumatic drugs in the treatment of arthritis!
7. List the disease-modifying antirheumatic drugs (DMARDs)!
When a drug is administered, a response occurs; if a second drug is given and the response to the first drug is altered, a drug interaction is said to have occurred. A drug interaction may be beneficial or harmful. It is deliberately sought in multidrug treatment of tuberculosis and when naloxone is given to treat morphine overdose. It is an embarrasment when a woman taking a combined estrogen / progesteron oral contraseptive for a desired interaction is prescibed a drug that is a metabolic enzyme inducer, with the result that she becomes pregnant. Although dramatic unintended interactions attract most attention and are the principal subject of this section, they should not distract attention from the many therapeutically useful interactions that are the basis of rational polypharmacy.
Vignete
Report of cardiac arrhythmias caused by unusually high blood level of 2 antihistamines, terfenadine and astemizole . These effect were best explained by?
A. Concomitant treatment with phenobarbital B. Use of these drugs by smokers
C. A genetic predisposition to metabolize succinylcholine slow D. Concomitant treatment with procainamide
E. Treatment of these patients with ketoconazole, an antifungi agent
Learning Task
1. What is pharmacodynamic interaction ? 2. What is pharmacokinetic interaction ? 3. Describe the antagonism!
4. Describe the synergism!
5. Describe the drug interactions that occur outside the body! 6. Describe the drug interactions that occur at site of absorption! 7. Describe the drug interactions that occur during distribution!
8. Describe the drug interactions that occur directly on receptors or on body systems! 9. Describe the drug interactions that occur during metabolism!
10. Describe the drug interactions that occur during excretion!
Adverse drugs reactions (ADRs), put simply, are noxious, unintended, and undesirable effects that occur as a result of drug treatment at doses normally used in man for diagnosis, prophylaxis, and treatment. Although there are many terms indicating the harmful and undesirable effects of drug treatment, the term ‘adverse drug reaction’ describes them best.
Lecture 12. Drug Interaction
During the course of treatment, drugs prescribed to patients produce certain effects other than the desired or expected effects. These cause concern both to the physician and the patient. They not only add to spiralling costs of medical treatments, but also cause a great deal of morbidity and mortality. These are generally referred to as ‘side effects’. People usually attribute these abnormal effects to either overdose or inappropriate medications prescribed by the doctor or the attending specialists. The unwanted effects are categorised into many types such as toxic effects, side effects, adverse reactions, and adverse drug events etc., depending upon the taxonomic classification used. Worldwide, studies have shown them to be a major cause of morbidity and mortality. Therefore, incidence of the adverse drug reactions is likely to be same as that of the West, or more. Unfortunately, inspite of presence of five wellorganised centres for drug monitoring in the country, the number of reports sent annually are dismal. Most of the adverse drug reactions are, fortunately, preventable. This calls for the urgent need to reinforce the monitoring of adverse reactions to drugs; public education against self-medication, inclusion of reaction monitoring, and an introduction to drug-safety in the curriculum of medical undergraduates, and systemic and periodic continuing medical education of health professionals. This multi-pronged strategy can lead to reduction in the incidence of adverse drug reactions
Learning Task
1. D.W. is a 9-year-old boy with osteosarcoma, which is being treated with ifosfamide and etoposide. He has no history of allergy. After two courses of chemotherapy, D.W. develops an upper arm deep venous thrombosis because of the chemotherapy. He is admitted to the hospital and initiated on heparin, omeprazole, and prophylactic antibiotics (piperacillin/tazobactam). On the third day of treatment, the swelling and pain in his upper arm have decreased significantly. Which one of the following best classifies D.W.’s chemotherapy adverse drug reaction (ADR)?
A. Type A. B. Type B. C. Type C. D Type D.
2. On the third hospital day, D.W.’s platelet count has dropped by 50% from baseline, and his alkaline phosphatase has increased to twice the normal value. He also begins to have some oozing of blood from his central catheter line site. The team agrees that these events are ADRs and asks you to narrow the suspected drugs to two agents. Which two-drug option is most likely causing these ADRs in D.W.?
A. Omeprazole and heparin. B. Heparin and ifosfamide. C. Ifosfamide and omeprazole.
D. Omeprazole and piperacillin/tazobactam.
3. You have been asked by your department’s director to compile a listing of your institution’s reported ADRs for review by your health system’s quality committee. Which one of the following metrics would be most helpful to ADR prevention?
A. Rate of ADRs per 100 admissions. B. Rate of ADRs per 100 discharges.
Once a patient with a clinical problem has been evaluated and a diagnosis has been identified, the doctor can often select from a variety of therapeutic approaches, including drug therapy. This requires the writing of prescription.
According to definition from WHO, a drug therapy is considered to be rational if patient receive medication in appropriate clinical indication, in appropriate dosage, in adequate duration of treatment and reachable cost. Therefore rational drug therapy must follow several basic principles including right indication, right drug, right patient, right dosage, right route of administration, right interval of treatment, right duration of treatment and caution for adverse effect.
Medication error is defined as any preventable event that may cause or lead to inappropriate medication use or patient harm, while the medication is in the control of the healthcare professional, patient or consumer. This might be derived from prescription (by a doctor), from preparation and dispension (by pharmacist) as well as from administration (by nurse).
Some issues related to medication error included incomplete prescription, wrong technique, poor communication, unreadable prescription, off label prescription, preparation error, excessive treatment, excessive cost, look alike and sound alike medication.
Vignete
A 30 years old man came to general practitioner due to fever since 4 days ago. Patient also complained headache, cough, cold and sore throat. Patient has already taken paracetamol but the complaints not getting better. After complete examination, patient was prescribed Demacolin® and Amoxsan® tablet. Patient was also still taken his previous medication (paracetamol) along with drugs given by the doctor because doctor didn’t instruct him to stop his previous medication.
Learning Task
1. Is there any irrational treatment happened in this patient? 2. What medication error has occurred in this patient?
3. Mention other type of medication error or irrational therapy. 4. How to avoid medication error?
5. What are the basic principles must be followed to perform rational drug therapy to the patient?
GENERAL DIRECTIONS
The aims of practicum
Direct observation on the effects of drugs in vivo
Comparing the practicum results with existing theories and making conclusion based on the comparation
Helping the students to comprehend the basics of pharmacology
The implementation of practicum by the students
By using this manual, the students are expected to work independently, in a solemn and systematic manner
The students are expected to take notes on the practicum results in a good way to optimize their way of studying
The lectures are only facilitators during the practicum
Evaluation
The knowledge on the effect of the drugs, based on the practicum results, will be assessed along with final exam.
Things that are expected from the students
The practicum can be done in an ordered manner
The students are expected to make good preparations before practicum to get maximum benefit from the implementation of practicum
The laboratory devices and the chemicals should be handled carefully
The laboratory animals should be handled with care, in a gentle manner. Do not inflict unnecessary sufferings to the animals.
HANDLING OF LABORATORY ANIMALS
Good knowledge and skills on laboratory animals handling is crucial in the establishment of ethically-sound research and to ensure good data collection. Thus, before doing any laboratory works (including practicum), the researcher should pay good attentions on these matters:
Working in a relaxed but solemn manner. If we become afraid and handle the animals in doubt, we are prone to technical difficulties.
Every step of laboratory works should not be done in rushed manner. It is recommended to not giving any kind of treatment if the animals are in agitated
state. Please make sure that they are calm before the treatment is commenced.
Improper animal handling may cause physical injuries to the researcher and/or the animals per se. This kind of handling may cause unnecessary stress to the animals, while also putting the laboratory devices in risk of damage.
Every laboratory animals should be handled with care, in a gentle and loving manner.
In vivo studies elaborately involving mice, rats, and rabbits as animal models.
Mice (Mus musculus)
Generally, mice will try to bite the handler for the first time. Gentle and loving care for several days may tame this animal, but we should always be careful not to bitten or scratched. Taking mice from its cage should be done gently, because this animal is easily startled. Please remember that mice can landed safely without injuries after jumping out from its cage/previous position for several meters.
Rabbit (Oryctolagus cuniculus)
Rabbit is usually tame, does not bite unless being stressed. Untame rabbit tends to live solitarily in the corner of its cage & behaves relatively aggressive (e.g., making intimidating sounds & positioning its forepaws in ready-to-scratch manner). Here are some tips to handle this animal:
Please be careful with its powerful hindpaws & sharp nails on its forepaws.
Generally, rabbit is prone to back (spinal) injury due to fall or incorrect handling.
It is recommended to wear long-armed lab coat to avoid being injured by this animal.
Do not handle this animal near your face. Avoid being scratched!
To handle rabbit out of its cage, hold both of its ears & nuchal skin. Using the other hand, hold its rear part (gluteal region) while setting its hindpaws freely. Under this handling, position the animal under your upper arm & armpit. This kind of positioning will calm the animal. Do not ever hold its ears if the abdominal or gluteal part has not been handled properly!
loves to be placed onto rough-textured surfaces (e.g., bambo or wire mesh). This animal may become panic if placed onto soft- or smooth-textured surfaces.
The purpose of therapeutics is to achieve the expected therapeutic effects, while minimizing the adverse effects in the same time. A physician should know the relative pharmacologic potencies and maximal efficacies of drugs in terms of instigating rational therapy. One of several parameters of drug effects is median effective dose or ED50. The definition of ED50 is the drug dose than can exert its therapeutic effect on 50% of the tested animals or individual. Several experts recommend the use of 4 graded doses, with a minimum of 4 sample animals per dose group to determine the ED50 value. In this practicum, we use diazepam (a sedative-hypnotic drug). Mice will be used to determine the ED50 of diazepam.
Animal Subjects
Mice (male) 16
Materials
Syringe (1mL) 4
Diazepam in 4 graded doses
(0,156 mg; 0,312 mg; 0,625 mg; 1,25 mg)
Plastic container (mice cage) + wire lids 4
Timer 1
Permanent marker 1
Details of Experimental Procedure
Take the mice from its cage by handling its tail
Put the mice on wire lids, handle its tail with left hand, then handle its posterior aspect of the neck using right hand
After the mice is handled safely, inject the 0,5 cc of diazepam intraperitoneally
Give mark on every mice that had been treated with the drug
Do all of the above steps for all of the animals
Evaluate the mice condition (sleep or fully alert) every 15 minutes for 30 minutes. To evaluate their conditions, put each of them on the wire lid then push them gently into supine position. If the animals can not grab the wire and tend to be in prone position, it can be concluded that the animals had been well sedated.
Note the observation results using the format of this table below! Zero (0) point is given If the mice is sedated (i.e., sleep), meanwhile one (1) point is given if the mice is fully alert/do not sleep.
Mice Dose I Group Dose II Group Dose III Group Dose IV Group
I II III IV TOTAL
Count the ED50 value!
From the above evaluation, ED50 value can be determined using this formula:
Log ED50 = Log Dα + d(f+1)
ED50 = median effective dose Dα = smallest dose
d = Log r; r = dilution factor = 2
f = can be known from a special table using n and k value (must be read from the smallest dose to the largest dose group)
n = number of the test animals
k = constant (the number of dose group – 1)
By using confidence interval (CI) 95%, the ED50 95% value can be determined from this formula:
Log ED50 95% = Log m + 2 α log m
ED50 95% = median effective dose 95%
Log m = Log ED50
α log m = d f
d = log r
f = table value
Disscuss the meaning of ED50 value you got from the experiment!
Autonomic nervous system (ANS) is the involuntary-controlled nervous system. The ANS regulates the functions of visceral organs (e.g., heart, respiratory tract, GI tract, glands, & blood vessels). The ANS consists of sympathetic & parasympathetic nervous system (abreviated as SANS & PANS, respectively).
The SANS consists of preganglionic fibers that synapse with neurons to form paravertebral ganglia, postganglionic fibers that innervate specificic glands or organs, adrenergic receptors that are widely distributed in the body, & several types of neurotransmitter.
Postganglionic SANS fibers end as swollen structures called varicoses. These structures contain neurotransmitter (noradrenaline/NA) storage vesicles. If an appropriate stimulus is present, NA can be released from its vesicles into the synaptic cleft. This neurotransmitter interacts with its receptor (presynaptic & postsynaptic) to exert its effect. This interaction will results in biochemical, biophysical & mechanical changes within the effector cell that can be observed as “response”. Thus, response in this context can be defined as the reaction of effector cell or organ upon specific stimulus. Because NA acts as transmitter in the SANS, hence sympathetic fibers are also called noradrenergic fibers. Due to the history of hypothetizing adrenaline as the primary transmitter in these fibers, they are classically known as adrenergic fibers. Drugs acting on the SANS are called sympathomimetics (mimic the effect of NA) & sympatholytics (lyse the effect of NA).
The PANS consists of soma that are located within ganglia (near the innervated organs), relatively short fibers, cholinergic receptors, & acetylcholine (ACh) as neurotransmitter. The fibers are also called as cholinergic fibers due to the role of ACh as their primary transmitter. Drugs acting on the PANS are called parasympathomimetics (mimic the effect of ACh) & parasympatholytics (lyse the effect of ACh).
Generally, SANS & PANS works as an opposite to one another (such as in the bronchial activity control), but there are some exceptions. The arterioles, for example, is dominantly innervated by SANS. The ventricular contractility is also dominantly regulated by SANS. Eye is one of several good examples of opposite function of the ANS innervations (i.e., SANS & PANS), because the response of topical ANS drugs on this organ can be easily observed. The SANS innervate the radial muscle of iris, meanwhile PANS fibers innervate circular muscle of iris. Both of these type of innervations regulate the diameter of pupils of both eyes. This practicum is about the effects of ANS drug on pupil diameter, using atropine and pilocarpine as experimental drugs.
The Aim of Practicum
This practicum is aimed on establishing better comprehension on ANS drugs pharmacodynamics, especially several drugs acting on PANS.
Animal Subjects
Rabbit (Oryctolagus cuniculus) Materials
Ruler (with milimeter scale)
Drop pipette
Flashlight
Test drug
Pilocarpine eyedrop (Pilocarpine Hydrochloride 0.001 %)
Atropine eyedrop (Atropine Sulphate 0.025 %)
Details of Experimental Procedure
1. Every students in each group should work under solemn manner using 1 rabbit. Treat the animal gently in order to make it calm.
2. Measure pupil diameter (LP), pupil reflex (RP), and observe conjunctival vessel (PD) condition of both eyes. Please take note on the results of observation (based on table of observation below).
Pupil diameter is expressed in mm (measurement using ruler).
Pupil reflex is expressed as positive and negative (measurement using flashlight). Conjunctival vessel condition is expressed as vasoconstricted or vasodilated
(measurement by direct observation).
3. Drop a little amount of pilocarpine solution onto right conjunctival sacs (3 drops).
4. Measure pupil diameter, pupil reflex, and observe conjunctival vessel condition every 5 minutes for 15 minutes. Please take note on the results of observation.
5. Wash the exposed eye with aquadest.
6. Perform same procedure using atropine eye drop to left eye. Take note on the results of observation.
7. Disscuss in your group about the result you observe from the experiment!
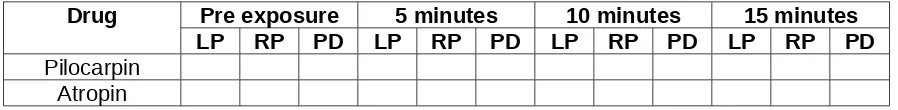
Table of Observation Result
Drug Pre exposure 5 minutes 10 minutes 15 minutes
LP RP PD LP RP PD LP RP PD LP RP PD
Smstr
Program or curriculum blocks
10 Senior Clerkship
9 Senior Clerkship
8 Senior Clerkship
7 Health System-based Practice
(3 weeks)
6 The Cardiovascular System and Disorders - sexology & anti aging Pathology & Clinical pathology (3 weeks)
Pendidikan Pancasila & Kewarganegaraan ( 3 weeks ) Inter Professional Education (smt 3-7)