ORIGINAL ARTICLE
Ethnic Variations in Risk Factor Profile, Pattern and
Recurrence of Non-Cardioembolic Ischemic Stroke
Dirk Deleu,
aAyman A. Hamad,
aSaadat Kamram,
aAbbas El Siddig,
aHassan Al Hail,
aand Samir M.K. Hamdy
baDepartments of Neurology andbCardiology, Hamad Medical Corporation, Doha, State of Qatar
Received for publication September 28, 2005; accepted January 6, 2006 (ARCHMED-D-05-00398).
Background. Ischemic stroke is influenced by ethnic and geographical variations. The aim of this study was to identify the risk factor profiles, subtypes and recurrence of non-cardioembolic ischemic stroke for the two largest subpopulations, the Arab and South Asians, at the only stroke-admitting hospital in Qatar.
Methods. Data on stroke patients admitted to Hamad Medical Corporation from January through December 2001 were reviewed in January 2005. Only patients with non-cardio-embolic ischemic stroke and complete work-up were included.
Results. A total of 303 patients with ischemic non-cardioembolic stroke fit the entry cri-teria. Sixty seven percent of the overall patient population (sex ratio 2:6, M/F) was of Arab origin, and 32% were South Asians. Hypertension was the most commonly encoun-tered risk factor followed by dyslipidemia, diabetes mellitus, and obesity. Significant dif-ferences between the Arab and South Asian subgroup of patients were observed with respect to number of risk factors and occurrence of obesity and diabetes. Carotid artery stenotic lesions, ventricular wall motion abnormalities and stroke recurrence were ob-served with a higher frequency in the Arab subgroup of patients compared with the South Asians. The majority of strokes were lacunar hemispheric strokes (68%), followed by lacunar brainstem strokes (15%) and large-vessel hemispheric infarctions (10%). Patients with a previous history of stroke had a higher frequency of carotid artery stenosis (p5
0.05) and risk of stroke recurrence (p5 0.04).
Conclusions. Unlike in other studies originating from the Arabian Gulf, lacunar stroke is the most common subtype of non-cardioembolic ischemic stroke in both the Arabs and South Asians in Qatar. Significant ethnic differences in age of occurrence, risk factor profile, and cardiovascular variables were observed. Ó2006 IMSS. Published by Elsevier Inc.
Key Words:Ischemic stroke, Risk factor, Echocardiography, Ethnicity, Qatar, Arab, South Asian.
Introduction
Stroke, the third leading cause of death in developed coun-tries, is a major cause of adult long-term neurological disability and accounts for the greatest number of hospital admissions related to neurological diseases (1). Stroke is generally more prevalent in the fifth and sixth decade of
life, and South Asians and people of African ancestry seem to be more susceptible than their Caucasian counterparts
(2,3). Over the last decade a series of publications on the epidemiology of stroke originating from the Arabian penin-sula have reported a stroke incidence among the local population on the order of 28273/100,000 inhabitants/year
(4–6). This low incidence rate probably relates to the rela-tive young age of this population and appears to be much lower compared with that encountered in Western countries (150–200/100,000 people/year)(7). However, the dramatic change in lifestyle in the Arabian Gulf countries over the past few decades shows that stroke, in particular ischemic
Address reprint requests to: Dirk Deleu, MD, PhD, FAAN, FRCP, Department of Neurology Medicine, P.O. Box 3050, Hamad Medical Corporation, Doha, State of Qatar; E-mail:[email protected]
stroke, poses a major health threat because of its associated morbidity and mortality, as well as its social and economic impact. For instance, in 1997 in Qatar, stroke patients occu-pied 10% of hospital beds (6).
The State of Qatar is the peninsula bordering the Ara-bian Gulf and Saudi Arabia and has an estimated popula-tion size of 850,000. No official data are available, but it is estimated that the expatriate population constitutes about 60% of the total population. Qatar is a member of the East-ern Mediterranean World Health Organization (WHO) and free national health care service for all nationals is the cor-nerstone of the health care program. In addition, free med-ical service is provided for expatriates and visitors examined at the Accident & Emergency Department, with-out requiring any referral from a health center. Hamad Medical Corporation (HMC) is the largest single govern-mental hospital in the State of Qatar with a capacity of 1,600 beds. Thus far, there are no private hospitals admit-ting stroke patients.
To understand the mechanisms of stroke and to target prevention, it is essential to recognize how risk factors dif-fer among etiological subtypes of stroke and/or ethnic groups. In addition, its prevention may critically reduce the cumulative public health burden associated with it. Sev-eral retrospective hospital-based studies on stroke have emerged from different Arabian Gulf countries (6,8–12). However, none has focused on the most common subtype of stroke, non-cardioembolic ischemic stroke. Furthermore, no data from government agencies are available on non-car-dioembolic ischemic stroke. The purpose of this hospital-based study was to evaluate risk factor profile and the sub-types, as well as the rate of recurrence, of non-cardioem-bolic ischemic stroke in this Arabian Gulf state community. More importantly, on the basis of this we inves-tigated for potential ethnic variations in non-cardioembolic ischemic stroke between the two largest subpopulations in this country, Arabs and South Asians.
Patients and Methods
Setting
The data of all patients admitted from January 2001 through December 2001 with stroke [categories 430–438 of the International Classification of Diseases, 9threvision (ICD–9)] at HMC—the only stroke-admitting facility in Doha and the whole of Qatar—were analyzed. To allow a sufficient long-term follow-up the review took place in January 2005, providing for some patients a follow-up period of at least 4 years. Only patients with non-cardioembolic ischemic stroke, complete medical records (history and physical examination) and work-up [including brain CT scan or MRI, carotid Doppler sonography, and transthoracic echocardiography (TTE) between 3 and 5 days of admission to HMC] were included in this study.
Hence, screening for these conditions was part of the work-up. Repeat neuroimaging was performed within 2 weeks of admission if the initial brain CT scan or MRI (and MR angiogram) was normal. When TTE was incon-clusive (e.g., due to lack of cooperation of the patient, un-clear imaging or high suspicion of cardioembolic source), transesophageal echocardiography (TEE) was performed.
Diagnostic Definitions and Criteria
The WHO definition for stroke: ‘‘rapidly developing clini-cal symptoms and/or signs resulting in foclini-cal or global dis-turbance in cerebral function leading to death or persisting for more than 24 h with no apparent cause other than vas-cular’’ was used(13). Non-cardioembolic ischemic stroke was defined as a stroke resulting from any cause except car-diac embolism, hypercoagulopathy or hematological disor-der. Hence, patients with transient ischemic attacks, intracerebral or subarachnoidal hemorrhage, proven cardi-oembolic ischemic stroke and stroke caused by hypercoa-gulopathies or hematological disorders were excluded.
A patient was considered to be hypertensive with an es-tablished history of blood pressure (BP)O140/90 mmHg in the non-acute phase or supervised use of antihypertensive medication(14). Patients with transient increase in BP on admission were not considered to be hypertensive. The cri-teria for diagnosing diabetes mellitus were the following: past history of supervised diabetes control or consistently high fasting plasma glucose levels (O7.0 mmol/L) (15). Dyslipidemia was defined as fasting plasma total choles-terol levels O5.2 mmol/L, plasma triglyceride levels
O2.0 mmol/L, plasma HDL-cholesterol!0.9 mmol/L or plasma LDL-cholesterolO3.4 mmol/L or using supervised treatment of hypolipidemic medication(16). A body mass index (BMI)$30 kg/m2was taken as diagnostic criterion for obesity. Smoking was classified into two categories:
(1) non-smokers/former smokers (never smoked regularly or stopped regular smoking$5 years ago) and(2)smokers (regular daily cigarette smoking within the last 5 years). Because of inaccuracy of the medical records, we did not quantify the amount of consumption or attempt to differentiate among cigarette, cigar and shisha (waterpipe) smoking.
the index stroke. All acute neurological events occurring within 3 weeks from the onset of the index stroke were con-sidered as part of the same event.
Data Collection
The following data were collected from all eligible pa-tients’ case records: age, gender, nationality, ethnicity (based on tribal name and area of origin), past or current history of stroke, presence of stroke-preventive therapy be-fore admission, presence of modifiable cardiovascular risk factors (including hypertension, diabetes, cigarette smok-ing, dyslipidemia, obesity, oral contraceptives, coronary artery disease, left ventricular dysfunction), complete neurological, vascular and cardiac examination, TTE or TEE with the determination of the left ventricular ejection fraction, carotid Doppler sonography to determine the pres-ence of stenotic lesions of the carotid arteries (50% stenosis was considered significant), neuroimaging (brain CT or MRI) with determination of subtype of ischemic stroke (small- or large-vessel stroke), site of stroke (hemispheric or brainstem) and, finally, in-hospital mortality due to stroke. In addition, secondary stroke prevention therapy and stroke recurrence after the index stroke in 2001 were recorded. Cases of symptomatic stroke recurrence were confirmed by readmission to HMC only.
Data Analysis
The data analysis is largely descriptive. All data were coded using Statistical Package for Social Sciences (SPSS) for Windows, version 10.0 data entry program. Data are ex-pressed as mean6standard deviation (SD). Where appro-priate, means of the different variables were compared using Student’s t-test. Comparison of non-continuous vari-ables between groups was performed by non-parametric testing. Pearson’s correlation coefficient was used to deter-mine the association between the left ventricular ejection fraction and the number of vascular risk factors and between smoking and carotid artery stenosis. Values of
p!0.05 were considered significant.
Results
Patient Population
From the 455 patients admitted with ischemic stroke in 2001, 303 (67%) matched the inclusion criteria of this study. Patients excluded had atrial fibrillation (61 patients), proven left ventricular thrombus (18 patients), hemorrhagic infarction or hemorrhagic conversion of the ischemic stroke (40 patients), hypercoagulopathy (6 patients), whereas in 27 patients data were missing or incomplete.
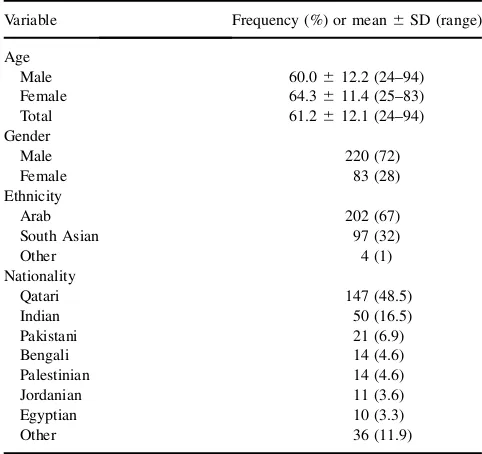
In our study population, the number of Qatari and non-Qatari was almost comparable (48.5 vs. 51.5%).
Further-more, 67% of the overall patient population was of Arab or-igin (Arab expatriates and Qataris), whereas 32% were South Asians. The overall sex ratio was 2:6 (M/F). Demo-graphic characteristics of the study population are summa-rized in Table 1. The age was significantly higher in the Qatari patients compared to the expatriate patients (67.3 vs. 55.5 years,p50.0001). The age distribution of the pa-tient population according to gender is shown in Figure 1. In addition, the male:female ratio was significantly lower in the Qatari patients (1:46) and Arab patient population (1:83) in general, compared with the South Asian patients (9:78, p50.0001).
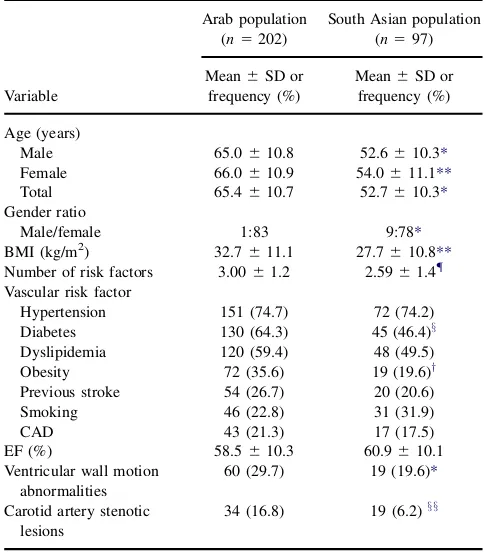
The clinical characteristics of the Arab and South Asian subgroup of patients are summarized inTable 2.
Risk Factors for Non-Cardioembolic Ischemic Stroke in this Community
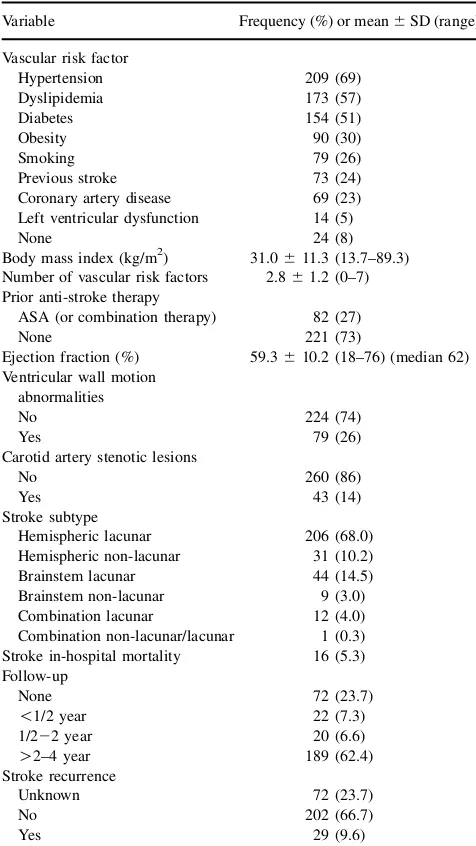
Table 3summarizes the patients’ modifiable cardiovascular risk factor profile: overall hypertension was the most com-monly encountered risk factor followed by dyslipidemia, diabetes mellitus, and obesity. More than 25% of patients were smokers, and a history of coronary artery disease including myocardial infarction was observed in 23% of patients. Eight percent of patients had no risk factor at all, whereas 12% had one risk factor, predominantly arterial hypertension. In the group of patients with at least two risk factors, dyslipidemia (particularly hypercholesterolemia) was most prevalent. One third of patients had three vascular risk factors, most commonly a combination of diabetes, hypertension and dyslipidemia (particularly hypercholesterolemia). Almost one quarter of the study
Table 1.Demographic characteristics of patients with
non-cardioembolic ischemic stroke (n5303)
Variable Frequency (%) or mean6SD (range)
Age
Male 60.0612.2 (24–94) Female 64.3611.4 (25–83) Total 61.2612.1 (24–94) Gender
Male 220 (72)
Female 83 (28)
Ethnicity
Arab 202 (67)
South Asian 97 (32)
Other 4 (1)
Nationality
Qatari 147 (48.5)
Indian 50 (16.5)
Pakistani 21 (6.9)
Bengali 14 (4.6)
Palestinian 14 (4.6)
Jordanian 11 (3.6)
Egyptian 10 (3.3)
Other 36 (11.9)
population had had a previous stroke, with 27% receiving aspirin either for secondary stroke prevention or cardiovas-cular reasons.
The prevalence of major risk factors across sexes was only significant for diabetes mellitus (76% in females vs. 51% in males, p 5 0.0001). In addition, Qatari patients had a significant higher prevalence of diabetes mellitus compared to expatriates (67 vs. 49%, p5 0.003). Signifi-cant differences between the Arab and South Asian subgroup of patients were observed with respect to number of risk factors and occurrence of obesity (BMI) and dia-betes (Table 2). Although there was a trend of a higher frequency of smokers in the South Asian community, the difference was not statistically significant (p50.09).
Echocardiographic and Carotid Sonographic Parameters
Overall, the ejection fraction averaged 59.3% (Table 3). Over one quarter of the patients had ventricular wall motion abnormalities (hypokinetic, dyskinetic or akinetic ventricu-lar wall segments). In patients with and without ventricuventricu-lar wall motion abnormalities the mean ejection fraction was 49.6612.5% and 62.866.3% (p50.0001), respectively. The presence of ventricular wall motion abnormalities highly correlated (p50.001) with the number of vascular risk factors (3.2 in patients with ventricular wall motion ab-normalities vs. 2.7 in the group of patients without ventric-ular wall motion abnormalities). Ventricventric-ular wall motion abnormalities were not a predisposing factor for stroke recurrence.
Almost 15% of patients had significant stenotic lesions on the carotid arteries. In this study population there was no significant association between smoking and carotid ar-tery stenosis, but this may be related to the small number of patients in the subpopulations. Carotid artery stenotic
lesions, cardiac wall motion abnormalities and stroke recur-rence were observed with a higher frequency in the Arab subgroup of patients compared with the South Asians (Table 2).
0 10 20 30 40 50 60 70 80
31-39 40-49 50-59 60-69 70-79 80-89 above 90
Age category (years)
N
u
m
b
e
r
≤30
Male
Female
Figure 1.Age and sex distribution.
Table 2.Clinical characteristics, distribution of risk factors
and ischemic stroke subtype among patients of Arab and South Asian origin (n5299)
Arab population (n5202)
South Asian population (n597)
Variable
Mean6SD or frequency (%)
Mean6SD or frequency (%)
Age (years)
Male 65.0610.8 52.6610.3*
Female 66.0610.9 54.0611.1**
Total 65.4610.7 52.7610.3*
Gender ratio
Male/female 1:83 9:78*
BMI (kg/m2) 32.7
611.1 27.7610.8**
Number of risk factors 3.0061.2 2.5961.4{
Vascular risk factor
Hypertension 151 (74.7) 72 (74.2) Diabetes 130 (64.3) 45 (46.4)x
Dyslipidemia 120 (59.4) 48 (49.5) Obesity 72 (35.6) 19 (19.6)y
Previous stroke 54 (26.7) 20 (20.6) Smoking 46 (22.8) 31 (31.9)
CAD 43 (21.3) 17 (17.5)
EF (%) 58.5610.3 60.9610.1 Ventricular wall motion
abnormalities
60 (29.7) 19 (19.6)*
Carotid artery stenotic lesions
34 (16.8) 19 (6.2)xx
BMI, body mass index; CAD, coronary artery disease; EF, ejection frac-tion; LVD, left ventricular dysfuncfrac-tion; SD, standard deviation. *p50.0001; **p50.002;{p
50.005;xp
50.004;yp
50.006;xxp
5
Ischemic Stroke Characteristics
With regard to the location of the infarct, the anterior circu-lation was affected in 78% and the posterior circucircu-lation in 17% of patients, whereas both territories were affected in 5% of cases. The majority of non-cardioembolic ischemic strokes were small-vessel infarctions resulting in lacunar hemispheric strokes in 68%, followed by lacunar brainstem strokes in almost 15% of patients. Large-vessel hemispheric infarctions were observed in 10% of patients. The direct stroke-related mortality 1 month following the non-cardio-embolic ischemic stroke was 5% and was exclusively asso-ciated with large-vessel stroke. The ratio for mortality was consequently higher for males than females (65 vs. 35%).
With regard to the risk factors, there was no relationship between each of the risk factors and the ischemic stroke subtype. Furthermore, with regard to stroke subtype, no difference was observed between both subpopulations.
Secondary Stroke Prevention and Stroke Recurrence
Over 25% of patients had been treated with antiplatelet drugs, predominantly aspirin, prior to their index stroke. The number of patients lost to follow-up after their index stroke in 2001 (primarily expatriates returning to their country of origin) was 24%. The median follow-up of the study population was between O2 and 4 years (Table 3). In the 189 patients with long-term follow-up after the index stroke in 2001, the stroke recurrence rate was almost 10%. Patients with a previous history of stroke had a higher fre-quency of carotid artery stenosis (p 5 0.05) and risk of stroke recurrence (p 5 0.04). With relation to frequency of stroke recurrence, no difference was observed between both subpopulations.
Discussion
Consistent with other studies in the region (9–11,18), our findings indicate that non-cardioembolic ischemic stroke is most prevalent between the ages of 55–75 years with a male preponderance, both in the Arab and South Asian subgroup of patients.
As for most studies originating from the Arab Gulf countries(4,5,8)and as observed in our study as well, the gender ratio is largely in favor of males and reflects the de-mographic structure in Qatar with its large expatriate male work force. Male preponderance seems to be a phenomenon observed in most epidemiological studies related to vascu-lar events in the Middle East. For instance, a recent epide-miological study assessing risk of acute myocardial infarction in different areas of the world found the highest male:female ratios in the Middle East and South Asia, 6.2 and 5.8, respectively, compared with values around 2.4 in Western populations (19). The same study provides inter-esting data with regard to age of a vascular event. The Arab and South Asian population have myocardial infarction around the age of 52 years, being 10 years earlier than Cau-casians(19). Our study revealed that the South Asian sub-group of patients had stroke at approximately the same age as the age reported for myocardial infarction. However, our Arab subgroup of patients had stroke at a much older age (65 years). Whether this demonstrates differential predispo-sition of cerebral and coronary vascular structure across populations to develop atherosclerosis is unclear but defi-nitely needs further exploration. Furthermore, it should be emphasized that other factors besides ethnic factors, such as sociocultural and economic factors, may have contrib-uted to this difference.
Table 3.Identifiable vascular risk factors, echocardiographic
parameters, carotid Doppler sonographic findings and ischemic stroke subtype (n5303)
Variable Frequency (%) or mean6SD (range)
Vascular risk factor
Hypertension 209 (69) Dyslipidemia 173 (57)
Diabetes 154 (51)
Obesity 90 (30)
Smoking 79 (26)
Previous stroke 73 (24) Coronary artery disease 69 (23) Left ventricular dysfunction 14 (5)
None 24 (8)
Body mass index (kg/m2) 31.0611.3 (13.7–89.3) Number of vascular risk factors 2.861.2 (0–7) Prior anti-stroke therapy
ASA (or combination therapy) 82 (27)
None 221 (73)
Ejection fraction (%) 59.3610.2 (18–76) (median 62) Ventricular wall motion
abnormalities
No 224 (74)
Yes 79 (26)
Carotid artery stenotic lesions
No 260 (86)
Yes 43 (14)
Stroke subtype
Hemispheric lacunar 206 (68.0) Hemispheric non-lacunar 31 (10.2) Brainstem lacunar 44 (14.5) Brainstem non-lacunar 9 (3.0) Combination lacunar 12 (4.0) Combination non-lacunar/lacunar 1 (0.3) Stroke in-hospital mortality 16 (5.3) Follow-up
None 72 (23.7)
!1/2 year 22 (7.3)
1/222 year 20 (6.6)
O2–4 year 189 (62.4) Stroke recurrence
Unknown 72 (23.7)
No 202 (66.7)
Yes 29 (9.6)
Hypertension, diabetes mellitus, dyslipidemia, smoking and coronary heart disease are well-known risk factors for stroke and are found in up to 80% of patients with ischemic stroke.(20)Diabetes mellitus proved to be a strong determi-nant for coronary artery disease and ischemic stroke among middle-aged women. (21) The prevalence of hypertension and diabetes mellitus in stroke populations in industrialized countries and certain Arabian Gulf countries (e.g., Saudi Arabia and Kuwait) is|54–72% and 14–69%, respectively (5,8,9,1,22–24). Hypertension and diabetes mellitus were much more commonly observed in our patient population (69% and 51%, respectively) than in Western studies.
Over the last 4 years, changes in the pattern of risk fac-tors have emerged. An epidemiological study on stroke in Qatar in 1997 (6) revealed that hypertension (66%) was the most common risk factor, followed by diabetes mellitus (46%). Although these epidemiological studies focused on stroke in general, comparison is still valid because ischemic stroke constituted the majority of cases (80%). In our over-all patient population, dyslipidemia has surpassed diabetes mellitus and has become the second most important modifi-able vascular risk factor in ischemic stroke. However, dif-ferent potentially modifiable vascular risk factor profiles were identified for the two ethnic subgroups of patients. Whereas dyslipidemia was the second most important risk factor in the South Asian subgroup of stroke patients, in the Arab subgroup of patients diabetes mellitus remained the second most important risk factor, and this largely be-cause of the significant contribution of native Qatari pa-tients, particularly female. Diabetes mellitus is prevalent among Qataris and Arabs in the Middle East with preva-lence rates varying between 15.0 and 23.7%(6,22,25). En-vironmental and sociocultural factors such as changes in lifestyle (sedentary, stress, fast food) in this rapidly devel-oping part of the world and consanguineous marriages may account for these findings. Similarly, the prevalence of diabetes mellitus in the South Asian population is also high, varying between 11 and 24%(26,27). The prevalence (around 25%) of coronary artery disease was similar to that reported in other studies (9,18,22). Cigarette smoking in a dose-related manner is a known risk factor for coronary artery disease and stroke, especially ischemic stroke (28). In our study, smoking accounted for 2% of all non-cardio-embolic strokes, a figure comparable with that of other re-cent studies in the region(22,29).
Some studies found an increasing risk of stroke, partic-ularly ischemic stroke, with a 6% increase in adjusted rel-ative risk for each unit increase in BMI(30,31). This was subsequently confirmed by Song et al., who showed a linear relationship between ischemic stroke and BMI(32). Com-pared with the BMI average in their study, the overall BMI average of our patient population was O30. This was particularly attributed to the Arab subgroup of patients (including Qataris), who had a significantly higher BMI than the South Asian subgroup of patients.
With reference to stroke subtype, our proportion of lacu-nar infarctions (68%) was higher than that in Western stroke studies, ranging from 10 to 24%(23,33,34). Previous stroke studies in Arabian Gulf countries revealed conflict-ing results. Large-vessel non-cardioembolic infarction was the most common type of stroke in hospital-based studies originating from Kuwait(4)and Saudi Arabia (11,29). Is-chemic stroke studies from South Asia revealed mixed re-sults: a Pakistani study showed a preponderance of lacunar strokes (43 vs. 27% large-vessel infarcts) (35), whereas an Indian study revealed a majority of large-vessel infarcts (41 vs. 18% lacunar infarcts)(36). In both studies the frequency of cardioembolic strokes was comparable. Although the association between small-vessel ischemic stroke and hypertension and diabetes mellitus has recently been challenged (37), it is widely believed that hyperten-sion constitutes a risk factor for large- and small-vessel dis-ease, whereas diabetes mellitus is mainly associated with arteriolopathy, probably explaining the high frequency of lacunar infarctions in our patients. Yip et al. showed that se-rum levels of cholesterol did not differ between various subtypes of ischemic strokes(38). Contrary to that finding
(38), patients with large-vessel infarcts did not have more vascular risk factors than those with lacunar stroke.
Doppler sonographic findings corresponded well with those reported in a Saudi Arabian study, which had similar rates of significant carotid artery stenosis, associated however with a lower rate of lacunar infarctions (11). Admittedly, their patients included all strokes subtypes (including intracranial hemorrhage).
There is a wide variation among stroke recurrence rates in study populations. These differences may be related to hospital vs. community-based samples, study designs and qualifying criteria for a recurrent event (39–41). In our study, the stroke recurrence rate corresponded well with that reported in other long-term follow-up studies(40,42). Furthermore, data from a recent Japanese study indicate that a previous history of stroke predicts stroke recurrence for all subtypes of ischemic stroke, whereas diabetes melli-tus appears to be a predictor of recurrence for patients with lacunar infarcts(43). Our study was not designed and did not have the power to evaluate the potential role of diabetes mellitus in recurrence of lacunar infarction.
Furthermore, the ejection fraction was substantially lower in our patients compared with that in the Japanese study, taking into account the fact that our patients did not have atrial fibrillation. Overall, we did not observe a higher frequency of stroke recurrence in patients with ventricular wall motion abnormalities. The reason for this might be that our patients had no ventricular thrombus and/or atrial fibrillation, which are known risk factors for ischemic stroke. The frequency of patients with ventricular wall motion abnormalities was sig-nificantly higher in the Arab subgroup of patients compared with South Asians and was most likely related to the signif-icantly higher number of risk factors (3.00 vs. 2.59).
In-hospital mortality rates in non-cardioembolic stroke are lower than that in cardioembolic stroke or intracerebral hemorrhage(45). Compared to a 12% mortality rate for is-chemic stroke reported in Qatar in 1997(6), the in-hospital case-fatality rate in our patient population was 6% and was in accordance with that reported in other studies
(5,6,35,40,45–49). Improvements in stroke care probably account for this reduction.
The limitations of this study may include its retrospec-tive nature making determination of etiology (cardioem-bolic vs. non-cardioem(cardioem-bolic stroke) sometimes more difficult and the imbalance in number of patients between both subpopulations. In addition, the non-systematic use of transesophageal echocardiography and conventional an-giography may have led to underestimation of angiopathies and cardiac abnormalities. It is important to highlight that the differences found are applicable to ethnic differences found in this community and cannot be extrapolated. Rea-sons for this include potential sociocultural and economic differences between the Arab and South Asian population. The results with regard to stroke recurrence need to be in-terpreted with caution, particularly because of high lost to follow-up of the expatriate patients. Finally, although it is realized that the data from patients with incomplete or missing information could have influenced our findings, this was very unlikely because they accounted for !6% of potentially eligible patients.
In conclusion, in both ethnic groups the triad of hyperten-sion, diabetes and dyslipidemia are the most common risk factors for non-cardioembolic ischemic stroke. A previous history of stroke was a determined factor for stroke recur-rence in our patient population. Furthermore, our results in-dicate that the overall distribution of non-cardioembolic ischemic stroke types in Qatar differ substantially from that of the Western and Southeast Asian populations and even from that of other Arab Gulf countries. High frequency of small-vessel disease, i.e., lacunar infarcts, and the high prev-alence of diabetes mellitus as a risk factor are quite distinc-tive. Diabetes, obesity, carotid artery stenosis and coronary artery disease with ventricular wall motion abnormalities were found significantly more in the Arab subgroup of pa-tients. However, this did not result in a difference in subtype of ischemic stroke between both ethnic groups.
References
1. Bonita R, Beaglehole R, Asplund K. The worldwide problem of stroke. Curr Opin Neurol 1994;7:5–10.
2. Cappuccio FP. Ethnicity and cardiovascular risk: variations in people of African ancestry and South Asian origin. J Hum Hypertens 1997; 11:571–576.
3. Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The Northern Manhattan Stroke Study. Stroke 1995;26:14–20.
4. Abdul-Ghaffar NU, el-Sonbaty MR, el-Din Abdul-Baky MS, Marafie AA, al-Said AM. Stroke in Kuwait: a three-year prospective study. Neuroepidemiology 1997;16:40–47.
5. al-Rajeh S, Larbi EB, Bademosi O, Awada A, Yousef A, al-Freihi H, et al. Stroke register: experience from the eastern province of Saudi Arabia. Cerebrovasc Dis 1998;8:86–89.
6. Hamad A, Hamad AA, Sokrab TO, Momeni S, Mesrauoa B, Lingren A. Stroke in Qatar: a one-year, hospital-based study. J Stroke Cerebrovasc Dis 2001;10:236–241.
7. Sudlow CL, Warlow CP. Comparing stroke incidence worldwide: what makes studies comparable? Stroke 1996;27:550–558.
8. Qari FA. Profile of stroke in a teaching university hospital in the West-ern region. Saudi Med J 2000;21:1030–1033.
9. Al Rajeh S, Awada A, Niazi G, Larbi E. Stroke in a Saudi Arabian National Guard community. Analysis of 500 consecutive cases from a population-based hospital. Stroke 1993;24:1635–1639.
10. al-Rajeh S, Larbi E, Bademosi O, Awada A, Ismail H, al-Freihi H. Pattern and ethnic variations in stroke in Saudi Arabia. J Neurol Sci 1991;102:112–118.
11. Awada A, al Rajeh S. The Saudi Stroke Data Bank. Analysis of the first 1000 cases. Acta Neurol Scand 1999;100:265–269.
12. Al Jishi A, Pochiaratu K, Mohan PK. Profile of stroke in Bahrain. Saudi Med J 1999;20:958–962.
13. World Health Organization. Cerebrovascular diseases: prevention, treatment, and rehabilitation: report of a WHO meeting. World Health Organ Tech Rep Ser No 469, 1971.
14. MacMahon S, Rodgers A. The epidemiological association between blood pressure and stroke: implications for primary and secondary prevention. Hypertens Res 1994;17(suppl 1):S23–32.
15. Anon. Report of the Expert Committee on the diagnosis and classifi-cation of diabetes mellitus. Diabetes Care 2000;25(suppl 1):S5–20. 16. Expert Panel on Detection, Evaluation, and Treatment of High Blood
Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on De-tection, Evaluation, and Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001;285:2486–2497. 17. Hier DB, Foulkes MA, Swiontoniowski M, Sacco RL, Gorelick PB,
Mohr JP, et al. Stroke recurrence within 2 years after ischemic infarc-tion. Stroke 1991;22:155–161.
18. al-Rajeh S, Larbi E, Bademosi O, Awada A, Ismail H, al-Freihi H, et al. Stroke in a tertiary hospital in Saudi Arabia: a study of 372 cases. Eur Neurol 1991;31:251–256.
19. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocar-dial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937–952.
20. Sandercock PA, Warlow CP, Jones LN, Starkey IR. Predisposing fac-tors for cerebral infarction: the Oxfordshire community stroke project. BMJ 1989;298:75–80.
21. Manson JE, Colditz GA, Stampfer MJ, Willett WC, Krolewski AS, Rosner B, et al. A prospective study of maturity-onset diabetes melli-tus and risk factors of coronary heart disease and stroke in women. Arch Intern Med 1991;151:1141–1147.
23. Bogousslavsky J, Van Melle G, Regli F. The Lausanne Stroke Regis-try: analysis of 1,000 consecutive patients with first stroke. Stroke 1988;19:1083–1092.
24. Jorgensen H, Nakayama H, Raaschou HO, Olsen TS. Stroke in pa-tients with diabetes. The Copenhagen Stroke Study. Stroke 1994;25: 1977–1984.
25. Al-Nozha MM, Al-Maatouq MA, Al-Mazrou YY, Al-Harthi SS, Arafah MR, Khalil MZ, et al. Diabetes mellitus in Saudi Arabia. Saudi Med J 2004;25:1603–1610.
26. Shera AS, Rafique G, Khwaja IA, Baqai S, Khan IA, King H. Pakistan National Diabetes Survey prevalence of glucose intolerance and asso-ciated factors in North West at Frontier Province (NWFP) of Pakistan. J Pak Med Assoc 1999;49:206–211.
27. Reddy NK, Kumar DN, Rayudu NV, Sastry BK, Raju BS. Prevalence of risk factors for coronary atherosclerosis in a cross-sectional popu-lation of Andhra Pradesh. Indian Heart J 2002;54:697–701. 28. Ueshima H, Choudhury SR, Okayama A, Hayakawa T, Kita Y,
Kadowaki T, et al. Cigarette smoking as a risk factor for stroke death in Japan: NIPPON DATA80. Stroke 2004;35:1836–1841.
29. El Sayed MM, Adeuja AO, El-Nahrawy E, Olaish MA. Characteristics of stroke in Hofuf, Saudi Arabia. Ann Saudi Med 1999;19:27–31. 30. Jood K, Jern C, Wilhelmsen L, Rosengren A. Body mass index in
mid-life is associated with a first stroke in men: a prospective population study over 28 years. Stroke 2004;35:2764–2769.
31. Kurth T, Gaziano JM, Berger K, Kase CS, Rexrode KM, Cook NR, et al. Body mass index and the risk of stroke in men. Arch Intern Med 2002;162:2557–2562.
32. Song YM, Sung J, Davey Smith G, Ebrahim S. Body mass index and ischemic and hemorrhagic stroke: a prospective study in Korean men. Stroke 2004;35:831–836.
33. Lemesle M, Milan C, Faivre J, Moreau T, Giroud M, Dumas R. Incidence trends of ischemic stroke and transient ischemic attacks in a well-defined French population from 1985 through 1994. Stroke 1999;30:371–377.
34. Mohr JP, Caplan LR, Melski JW, Goldstein RJ, Duncan GW, Kistler JP, et al. The Harvard Cooperative Stroke Registry: a prospec-tive registry. Neurology 1978;28:754–762.
35. Syed NA, Khealani BA, Ali S, Hasan A, Akhtar N, Brohi H, et al. Ischemic stroke subtypes in Pakistan: the Aga Khan University Stroke Data Bank. J Pak Med Assoc 2003;53:584–588.
36. Kaul S, Sunitha P, Suvarna A, Meena AK, Uma M, Reddy JM. Subtypes of ischemic stroke in a metropolitan city of South India (one year data from a hospital based stroke registry). Neurol India 2002;(suppl 50):S8–14.
37. Schulz UG, Rothwell PM. Differences in vascular risk factors between etiological subtypes of ischemic stroke: importance of population-based studies. Stroke 2003;34:2050–2059.
38. Yip PK, Jeng JS, Lee TK, Chang YC, Huang ZS, Ng SK, et al. Subtypes of ischemic stroke. A hospital-based stroke registry in Taiwan (SCAN-IV). Stroke 1997;28:2507–2512.
39. Petty GW, Brown RD Jr, Whisnant JP, Sicks JD, O’Fallon WM, Wiebers DO. Survival and recurrence after first cerebral infarction: a population-based study in Rochester, Minnesota, 1975 through 1989. Neurology 1998;50:208–216.
40. Sacco RL, Shi T, Zamanillo MC, Kargman DE. Predictors of mortality and recurrence after hospitalized cerebral infarction in an urban com-munity: the Northern Manhattan Stroke Study. Neurology 1994;44: 626–634.
41. Burn J, Dennis M, Bamford J, Sandercock P, Wade D, Warlow C. Long-term risk of recurrent stroke after a first-ever stroke. The Oxfordshire Community Stroke Project. Stroke 1994;25:333–337. 42. Moroney JT, Bagiella E, Paik MC, Sacco RL, Desmond DW. Risk
factors for early recurrence after ischemic stroke: the role of stroke syndrome and subtype. Stroke 1998;29:2118–2124.
43. Soda T, Nakayasu H, Maeda M, Kusumi M, Kowa H, Awaki E, et al. Stroke recurrence within the first year following cerebral infarction— Tottori University Lacunar Infarction Prognosis Study (TULIPS). Acta Neurol Scand 2004;110:343–349.
44. Naito S, Imataka K, Seko Y, Fujii J. The predictive factors for cerebral infarction in patients with non-rheumatic atrial fibrillation. J Cardiol 1990;20:385–391.
45. Fang J, Foo SH, Jeng JS, Yip PK, Alderman MH. Clinical character-istics of stroke among Chinese in New York City. Ethn Dis 2004;14: 378–383.
46. Ward G, Jamrozik K, Stewart-Wynne W. Incidence and outcome of ce-rebrovascular disease in Perth, Western Australia. Stroke 1988;19: 1501–1506.
47. Sacco SE, Whisnant JP, Broderick JP, Philips SJ, O’Fallon WM. Epi-demiological characteristics of lacunar infarcts in a population. Stroke 1991;22:1236–1241.
48. Ashok PP, Radhakrishnan K, Sridharan R, el-Mangoush MA. Inci-dence and pattern of cerebrovascular diseases in Benghazi, Libya. J Neurol Neurosurg Psychiatry 1986;49:519–523.