Dibiayai oleh: DIPA PNBP Universitas Udayana
sesuai dengan Surat Perjanjian Penugasan Pelaksanaan Penelitian Nomor: 246-371/UN14.2/PNL.01.03.00/2015, tanggal 21 April 2015
RESEARCH REPORT
UDAYANA INTERNATIONAL RESEARCH
COLLABORATION
RESEARCH TITLE
THE IMPLEMENTATION RESEARCH OF A TEST AND TREAT STRATEGY FOR HIV TREATMENT AND PREVENTION AMONG HIGH RISK MEN (HRM) GROUP IN BALI INDONESIA
Assessment Study (year 1)
RESEARCH TEAM
dr. Pande Putu Januraga, M.Kes, DrPH (0010017902) Prof. dr. Dewa Nyoman Wirawan (0010104802) dr. Luh Putu Lila Wulandari, MPH (0027067806)
dr. AAS Sawitri, MPH (0014096801) Desak Widyanthini, SKM, M.Kes
Institution partner: Kirby Institute UNSW, Australia
FACULTY OF MEDICINE
UDAYANA UNIVERSITY
November 2015
2
TABLE OF CONTENTS
TABLE OF CONTENTS ... 2
SUMMARY ... 4
1 INTRODUCTION ... 5
1.1 Background and rationale ... 5
1.2 Objectives ... 6
2 METHODS ... 6
2.1 Overview of study design ... 6
2.2 Duration ... 6
2.3 Study setting ... 6
2.4 Study population and sample ... 7
2.5 Data collection and analysis ... 8
2.6 International partner (Kirby Institute) roles ... 9
2.7 Results dissemination and peer reviewed publications ... 9
2.8 Ethics consideration ... 9
3 STUDY BUDGET AND SCHEDULE ... 11
3.1 Budget summary ... 11
3.2 Schedule of activities ... 11
4 Survey Results ... 12
4.1 Respon rate ... 12
4.2 Sociodemographic characteristics of the participants ... 12
4.3 Number and type of sexual partners ... 13
4.4 The sexual practices with regular non commercial partners. ... 13
4.5 The sexual practices with casual non commercial partners. ... 13
4.6 The sexual practices with female sex workers partners ... 14
4.7 Social network ... 14
4.8 Knowledge about condom ... 15
4.9 Knowledge and history of STI ... 15
4.10 Knowledge on HIV ... 16
4.11 HIV testing ... 16
3
4.13 Health seeking behaviour ... 18
4.14 Predictors of HIV testing ... 18
Discussion ... 19
Conclusions ... 21
Appendix 1 Test and treatment facility ... 22
Appendix 2 Study team ... 23
Appendix 3 Questionnaire ... 24
Appendix 4 Observation form and In-depth interview questions ... 25
Appendix 5 Information card ... 26
Appendix 6 Information letters for in-depth and survey ... 27
Appendix 7 Verbal consent ... 28
4
SUMMARY
The primary objective of this study was to identify strategies of increasing HIV test and treatment uptake, also known as the test and treat (T&T) strategy, among clients of female sex workers (FSWs) i De pasa Bali. The stud ’s spe ifi o je ti es e e:
1. To investigate HIV related risk behaviours of clients of FSWs.
2. To investigate the barriers of HIV testing and treatment uptake among clients of FSWs 3. To quantify the cascade of HIV treatment during the time of study conducted.
Mixed research methods using quantitative and qualitative approaches were employed. The quantitative phase applied a survey procedure in brothel based sites in Denpasar area. Survey interviews were delivered by seven trained field workers of Yayasan Kerti Praja, Denpasar. They had been trained to approach clients of sex workers to join the study, to complete questionnaire and to provide survey respondents with information on HIV testing and treatment facilities at Yayasan Kerti Praja, Denpasar. Furthermore, in-depth interviews were conducted to investigate the barriers of HIV testing and treatment uptake among clients of FSWs. This report will only be describing the result of the first objectives of this study. Other objectives will be described in other report formats which will be published in international journals.
5
1 INTRODUCTION
1.1 Background and rationale
While a number of national and local surveillances is still reporting the high burden of HIV epidemic among injecting drug users (IDUs) in Indonesia, there is a growing evidence of an increasing trends of sexual transmission of HIV, with female sex workers (FSWs) and man having sex with man (MSM) bear a disproportionate burden of the epidemic.1-3 One of the province with continuing high prevalence of
HIV among FSWS is Bali. A number of surveys have indicated that relatively low rates of consistent condom use and high numbers of clients made FSWs at risk of infection.3
To anticipate the problems and to curb the spread of the epidemic into more general population, following the national policy, Bali Health Office (BHO), Bali AIDS Commission (BAC) and related stakeholders including local NGOs have agreed that the interventions should be designed comprehensively to facilitate health providers to be able to address the needs of affected populations while also empower them to participate actively in the designing and implementing of interventions.4
This will only be possible through the effective implementation of Layanan Komprehensif berkesinambungan (LKB) that consist of different strategies including health education, condoms distribution, STIs test and treatment, as well as strategic use of antiretroviral (SUFA). The implementation of this comprehensive package have been started gradually since 2009,5 with
intervention focusing on peer education, condom distribution and improvement of FSWs access to STIs clinics. Since 2013 the comprehensive package has been equipped by the implementation of test and treat strategy or SUFA.
While intervention to reduce the risk of HIV infection among FSWs in Bali have developed progressively, limited is addressed to the other core group that link directly to FSWs group; their clients. This group has important role on HIV transmission to the general population, linking high prevalence of HIV infection among FSWs to the general population of women (wives, girlfriends).6,7
Traditionally, in Indonesia, this group is labelled as mobile man with money (3M), thus, within a number of surveys, clients of sex workers were represented mostly by driver (truck or taxi).8-10 This
made the overall characteristics of clients is remain unknown. Some studies conclude that efforts to reduce the risk of HIV infection among clients of FSWs might have a considerable impact in slowing the spread of epidemic.11,12
6 characteristics of clients, their related risk behaviours as well as barriers to access testing and treatment.
1.2 Objectives
1. To investigate HIV related risk behaviours of clients of FSWs.
2. To investigate the barriers of HIV testing and treatment uptake among clients of FSWs 3. To quantify the cascade of HIV treatment during the study time.
2 METHODS
2.1 Overview of study design
This was a cross sectional research study using quantitative and qualitative approaches that were conducted over three months of duration. During this time, a cross-sectional sexual behaviour study were conducted, 200 informants were recruited for interview. In addition to interviews, all survey informants received information on the availability of free HIV testing and treatment facility at YKP Clinic in Denpasar (details of the clinic is available in appendix 1). In order to have thorough understanding on the barriers of HIV testing and treatment uptake among clients of FSWs, 20 participants were recruited for in-depth interviews.
2.2 Duration
The study was conducted within 6 months from preparation for the study (refining the study protocol, obtain ethics approval, developing manual of operations, staff training et cetera) to the commencement of participant recruitment (survey, HIV test, and in-depth interviews).
Analysis and evaluation, reporting and preparing publication outputs will continue beyond the study period.
2.3 Study setting
7
2.4 Study population and sample
The study population is the clients of FSWs working in the selected brothels. A client of FSWs was defined as a male who is present in the brothel during the intensive outreach and who have a history of sexual transaction at the brothel sites with a FSW working there.
Eligibility criteria for enrolment:
Participants had to meet all of the following inclusion criteria: i. Aged 18 years and over;
ii. Self-reported sex with female sex workers in the last 12 months; iii. Providing consent to be enrolled in the study.
Exclusion criteria included:
i. Unable to provide informed consent;
ii. Participation in another study with a similar research focus;
iii. Known to be HIV-i fe ted the stud tea a d stud ’s e u e ato s.
All men who fall into the client definition and fulfil the criteria are eligible to participate, thus will were invited to join the study.
200 clients joined the survey and received information on free HIV testing and treatment at YKP clinic in Denpasar. Since providing survey respondents with information on free HIV testing and treatment facility is a normal practice in any outreach program among at risk populations, this activity was not considered as a study intervention. Within this scenario the study was not targeting number of survey respondents that would finally come to the clinic, however, based on regular reports provided by outreach and VCT program of YKP.
8
2.5 Data collection and analysis
The survey phase of the study was delivered by 7 field workers (penjangkau) of Yayasan Kerti Praja. These staffs have had experiences of working with hard to reach population including clients of sex workers. They were trained in a workshop to recruit survey informants, to conduct survey interviews using structured questionnaire (appendix 4) as well as to provide clients with information card on free HIV testing and treatment facilit at YKP’s li i appe di . The su e i te ie s e e o du ted in sex workers rooms available in each location/brothel. Before the survey, the YKP field staffs
egotiated the a aila ilit of these oo s ith all othels’ a age s of sele ted sites.
Meanwhile in-depth interviews in the qualitative phase of the study were delivered in a private room available at YKP building by the principal investigator and a co-investigator using semi-structured open ended questions (appendix 5). All potential parti ipa ts e e app oa hed a d e uited YKP’s field work staffs during the survey and clinic visits. For participants recruited during survey time, they will be offered transport costs for travelling to YKP building.
The study were not provide or delive a li i al i te e tio to the stud ’s pa ti ipa ts; ho e e , as explained before, it is anticipated that there were a number of study participants who have received information on free HIV testing and treatment facility at YKP might come to the clinic for services. In this case, the clinic staffs (doctors, nurses, analyst and counsellors) would conduct HIV test and t eat e t as usi ess as usual usi g o al “OP p a ti ed the YKP’s li i . The “OP itself is alig ed with the national guidelines on HIV test and treatment for high risk group people including clients of sex workers. In order to prepare the clinic well, before the data collection begin, the study team held a meeting with YKP clinic staffs to discuss the data management procedure. There were two important procedures involved at this stage; first, the process of identifying clients who come to the clinic prior to receiving information card from the survey. Second, the process of de-identifying VCT and ART data from this group of clients to be used by the study.
F o those stud ’s a ti ities, th ee t pes of data e e de eloped:
a. Data from survey, this was a quantitative data useful for generating information on sexual behaviours of clients of FSWs. A number of univariate and multivariate statistical procedures were conducted in order to gain determinants of sexual behaviours including condom use; b. Data from in-depth interviews, this was a qualitative data useful for theorising the underlying
9 c. Results on HIV testing and treatment, this was a quantitative data useful for generating summary on HIV testing and treatment uptake. Demographic characteristics of all subjects being tested for HIV were summarized. The rates of HIV diagnosis, transfer to care, and commencing ART, was also summarized.
2.6 International partner (Kirby Institute) roles
The Kirby Institute, formerly the National Centre in HIV Epidemiology and Clinical Research (NCHECR) collaborated extensively in the international effort that ensured that HIV became one of the most intensively studied diseases in the history of medical science. The Kirby Institute is directly affiliated with the Faculty of Medicine at the University of New South Wales (UNSW), and receives funding th ough the Aust alia Go e e t Depa t e t of Health a d Agei g. The Ki I stitute’s p i a functions relate to the co-ordination of national surveillance programs, population health and epidemiological research, clinical research and clinical trials. With these extensive experiences, Kirby Institute provided active consultation for the development of study design including instruments developments. The Kirby Institute also assisted local research team in developing and analysing the stud ’s data.
2.7 Results dissemination and peer reviewed publications
A fi al epo t is su itted to Uda a a U i e sit Resea h I stitutio LPPM at the e d of the stud ’s duration as per their requirements. This report describes the results of the survey, while the results of interviews and observations will be reported in other format. The study results will also be disseminated for relevant stakeholders in Bali and Jakarta (KPAN and Ministry of Health) through policy briefs and series of seminars. Main study findings as well as sub-analyses and sub-studies will be published in peer-reviewed journals.
2.8 Ethics consideration
During the data collections, all potential subject in survey and in-depth interviews were handed an information letter explaining the purpose of the study (appendix 7). Those willing to participate in the study were asked to give verbal informed consent. For survey respondents responding to the questionnaire in the survey phase after receiving information on the survey procedure is considered as implying consent to participate in the study.13 For in-depth i te ie s, pa ti ipa ts’ o se t to e
10 workers. Also, verbal agreement is an alternative to signed consent forms in cross-cultural research and research in marginalised or oppressed groups or hard to reach population including clients of sex workers.13,14 By doing this, the study ensured that all subjects participate voluntarily. In addition,
during data collection all study subjects had right to withdraw their involvement at any time they want, this right has been clearly written in the information letters and verbal consent documents. Meanwhile for both HIV testing and ART initiation, the study will rely on the standard clinical procedu e of YKP’s li i , the stud ill o l gai de-ide tified data f o lie ts’ e o ds.
Furthermore, the study subjects were offered funds for their times spend in survey (Rp. 50,000.-) and in in-depth interviews (Rp. 75,000.-) to recognise their valuable contribution to this research. Participants also received information card on free HIV testing and treatment facility available at YKP in Denpasar. These practices are common for HIV research in Indonesia and particularly in Bali. For those who come to the clinic after receiving information from the survey, HIV test were performed based on normal procedure conducted at the clinic with adequate pre- and post-test counselling by trained personnel to minimize risk which might arise from learning of HIV diagnosis. There were no reward for clients who come to the clinic for testing and treatment as normal or usual procedure were applied to them. Irrespective of no direct financial reward for their participation in the test, knowing HIV status earlier and joining the ART earlier in case they are found to be positive will benefit the health of clients.
All stud i fo a ts, pa ti ipa ts a d patie ts’ o fide tialit e e ai tai ed th oughout the stud . “u je ts’ ha d op data e e sto ed i a lo ked a i et i P“IKM FK UNUD, while softcopy data were stored in a password protected laptop. These data were kept for the duration five years after the study fi ish, o l the stud ’s tea had a ess to it. Fu the o e, o l de-identified data will be used in all reports and publications related to the study. All patients starting ART in the study will be continuing the treatment after the conclusion of the study as there is no current evidence supporting treatment interruption. Also, this treatment will be provided through the national ART policy and program (Strategic use of ART –Layanan Komprehensif Berkesinambungan or SUFA-LKB).
11
3 STUDY BUDGET AND SCHEDULE
3.1 Budget summary
The stud is fu ded th ough i te atio al esea h olla o atio g a t, U i e sitas Uda a a’s research unit. The overall budget for 6 months study is one hundred million rupiah. There is no funds support from the international partner.
3.2 Schedule of activities
The study will be conducted from May 2015 and should be concluded in November 2015 as outline in table below
Activities
2015
1 2 3 4 5 6 7
Preparatory activities and study setup
Apply for Ethics Committee approval
Intensive outreach training and workshop
Survey
In-depth interviews
Analysis and Reporting
12
4 Survey Results
4.1 Respon rate
Among 412 participants who were approached during the data collection, 200 of them agreed to participate in the survey, giving the response rate of 48.5%. Among these, 200 questionnaires were included in the analysis
4.2 Sociodemographic characteristics of the participants
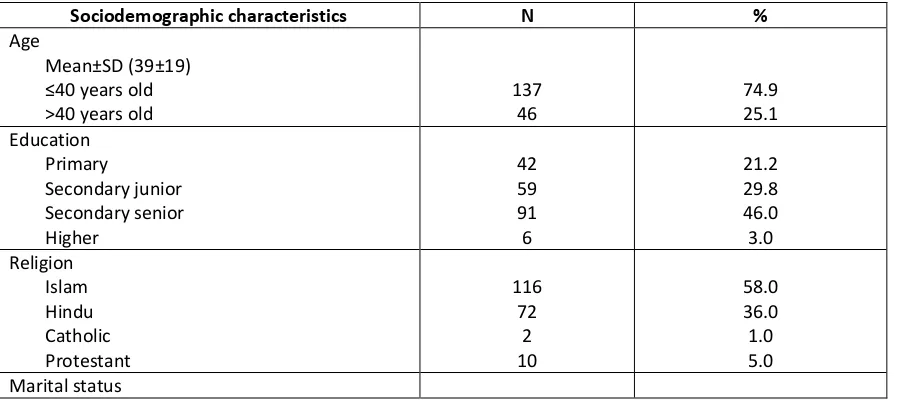
The mean age of participants were 39 years old, with the majority of them (46%) enjoyed the highest education in the senior high school. Islam and Hindu comprised the two main religions among participants, 58% and 36% respectively. The majority of the respondents came from Java (49%) and Bali(36%). 65% of respondents admitted that they consume alcohols at least less than once a week. Only 2 respondents had a history of drug use, and none of these were on injecting drug.
In terms of marital status, more than half (131 or 65,5%) of them have ever been married and currently remain married, with almost 70% of them married at the first time at the age between 23-30 years old. Those who reported that they currently married, 58% of them living with their spouse. On the other hand, those who reported that they do not married, 7% of them admitted they livewith their sexual partners.
While the majority of respondents (70.5%) of them reported that their age when they first married were between 23-30 years, surprisingly the majority of the respondents begin their sexual debut long before that age. More than 80% of the respondents reported that the first time they had sex were at the age between 14 to 22.
Table 4.1 Sociodemographic Characteristics of the Participants
Sociodemographic characteristics N %
13 Ever been married/currently remain married
Never married
4.3 Number and type of sexual partners
The number of commercial sexual partners the participants had within the last 12 months ranging from 1- 24, with 80% of the participants admitted they had sex with 1-5 female sex workers within the last 12 months. In addition to female sex workers, 18% of the respondents also admitted that they had other occasional non-commercial sexual partners, with the number of this type of partners ranging from 1-2. None of the respondents in this study reported the history of having sexual relationship with men.
4.4 The sexual practices with regular non commercial partners.
128 (64%) of the respondents reported that they had this regular non commercial sex partners (including wife). When they were asked about how many times they had sex with this partners in the last month, the answer was ranging from 0 to 20 times, with around 40% of them had sex 2-4 times within a month. Only 4 of the respondents reported the use of condom with this type of partners in the last sex. While the respondents who reported to use condom mentioned that it was the join decision with their partner, those who reported of not using condom mentions various reasons of not using it. The three most common reasons for not using condom were that because they already use other contraception methods (65%), because they thought it as ot e essa % a d the did ’t like it (35%). When the question on the time period of condom use was expanded to the period of
ithi the last ea , still the ajo it % of the espo de ts ad itted the e e use it.
4.5 The sexual practices with casual non commercial partners.
14 condom was not necessary ( 12%). When they were asked about the use of condom within last year, the majority answer given was sometime ( 43%).
4.6 The sexual practices with female sex workers partners
While all of the respondents reported to have sex with brothel based sex workers within the last year, only 5(2.5%) of them reported to have sex with non-brothel based sex workers within the same period, with the number of non-brothel based sex workers they had sex with were 1, and admitted that they have sex with this type of sexual partners 1-3 times in the last year.
The number of brothel based commercial sex partners the respondents had within the last year ranging from 1 to 24. The number of sexual engagement with FSW within the last month were ranging from 0-8, with the majority of respondents (76.5%) reported the number of sexual activity with this type of partner in the last month between 1-3 times.
The majority of the respondents (88.5%) said they use condom when the last time they had sex with the brothel based sex workers. Those who used condom, mentioned the decision maker process of using condom that that it was the decision of their sexual partners to use it (43.3%), it was the join decision (37.8%), and his decision ( 18.3%). Those who reported not to use condom mentioned despite they aware of the availability of condoms in the brothels, the three most common reasons for not usi g o do e e as follo : e ause the did ot like it . % , e ause it as ’t e essa to use condom ( 27.3%), and because they did not think of it ( 13.6%). When the time period of condom use uestio e e e pa ded as ithi the last o th , 61% of the respondents reported the use of condom every time they have sex with sex workers.
4.7 Social network
15
4.8 Knowledge about condom
192(96%) of the respondents reported that they have ever used condom previously. Almost all ( 199 or 99.50%) have heard about male condoms, however only 4% of the respondents have heard about female condoms. 97% of the respondents know where to find condoms, with sexual partners (56.41%), pharmacy (56.41%) and friends (21.5%) were three most quoted sources where they can find condoms.
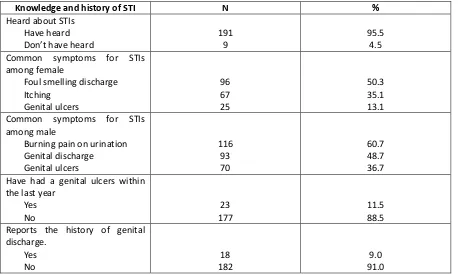
4.9 Knowledge and history of STI
Regarding knowledge on STI, 95.5% of the respondents have heard about STIs. Foul smelling discharge (50.3%), itching (35.1%), and genital ulcers (13.1%) were three most perceived common symptoms for STIs among female; while the three most quoted STIs symptoms among male were burning pain on urination (60.73%), genital discharge (48.7%), and genital ulcers (36.7%). Among the respondents, 11,50% admitted that they have had a genital ulcers within the last year, while 9% also reports the history of genital discharge.
Table 4.2 Knowledge and history of HIV among participants
16
4.10 Knowledge on HIV
Almost all (185 or 92.50%) of the respondents have heard about HIV. However only 43% perceived themselves at high risk of HIV, while 40% others perceived that they may be at risk, and 7.6% of them perceived that they were not at risk at all of HIV.
Although more than half (59%) of the respondents did not know someone who are infected with HIV, and no relatives were infected with the virus (91.3%), the majority of the respondents (61.62%) perceived HIV as very severe.
Although most two third (77%) answered yes when they were asked of whether we can protect ourselves by consistently using condom during sexual act, 71% said yes when asked whether having faithful partner can protect them from HIV, and 72% answered yes when asked about whether abstinentia can protect them from HIV infection, and 91% said yes when asked whether sharing needles can be a means of HIV transmission; misconception about HIV transmission is still common. Only 44% of the respondents said that HIV cannot be transmitted by mosquito bites nor by sharing food and drink with HIV infected persons. Additionally, around 67% do not or not sure if person infected with HIV might look as other healthy people.
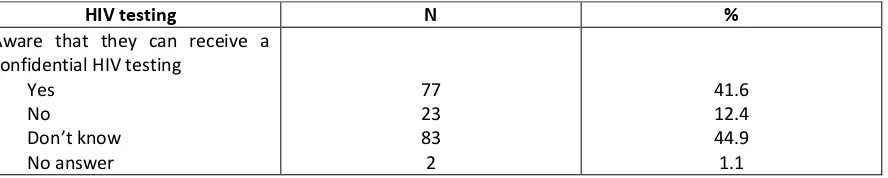
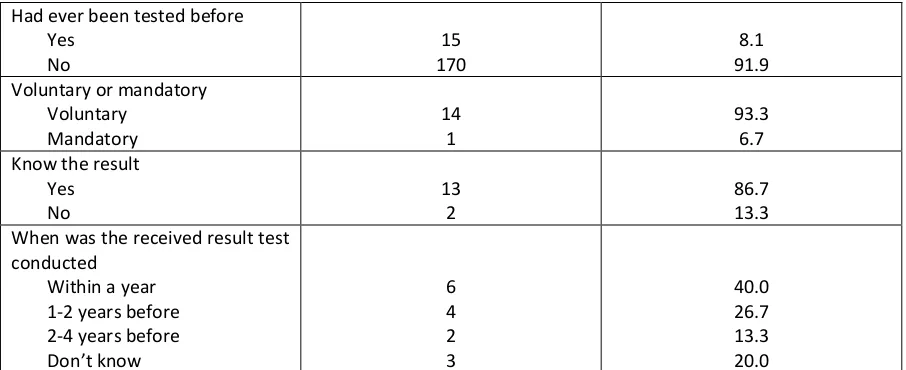
4.11 HIV testing
With regards to HIV testing, only 41.6% of the respondents aware that they can receive a confidential HIV testing. Only 15 people (8.1%) had ever been tested before, and most of them ( 14 persons) seek the test voluntarily, and only 13 people got the results of the test. Among those who got the results. 6(40%) of them mentioned that the test was conducted within a year, 4(26.67%) of them did the test 1-2 years before, and 2 of them did the test 2-4 years ago.
Only 39.50% of the respondents know where to get tested, and 76% of these who knew where to get tested, 76% perceived that those places were convenient.
66.5% of the participants answered yes when they were asked whether they would willing to receive an HIV test offer in the future.
Table 4.3 HIV testing awareness and experiences
17 When was the received result test
conducted
4.12 Exposure to health promotion activities
The exposure of health promotion activities were explored in this survey. When exposure to everyday social media was asked, the rank of media used every day by the participants rank from television ( 91.50%), radio ( 25%), online social media ( 11%), and newspaper ( 6.5%). However, the rank is different, when they were asked about whether they have heard about HIV information from those media, i.e newspaper (84.50%), social media (77.8%), tv (71.50%), and radio ( 61.3%).
When they were asked about health education session they had ever attended, only 19% of said that they have attended health education session, with almost all of these mentioned that they received HIV information on that session.
Table 4.4 Exposure to HIV Promotion Activities
Experiences on health promotion activities
N %
18
4.13 Health seeking behaviour
Among those who had a history of STI symptoms, the first thing they did when they had the symptoms were seek medicine at the chemist. This was the answer mostly expressed by the participants (35.71%).
Analysis was conducted to identify predictors of history of HIV testing among this group. Several variables were selected based on that they suggested as factors that more likely to influence HIV testing. These factors include age, age at the first married, age at first sexual intercourse, number of wife and regular partners, number of female sex workers they have had sex with, and number of occasional sexual partners; the highest education level, history of alcohol, and drugs, history of marriage, the use of condom, knowledge that HIV can be transmitted through sexual act, history of genital ulcer within a year, history of genital discharge within a year, have heard about AIDS, perceived risk, and the history of HIV information exposure through several media; history of having attended education session on HIV, and know the place to get tested, and perception whether those place were convenient.
4.14 Predictors of HIV testing
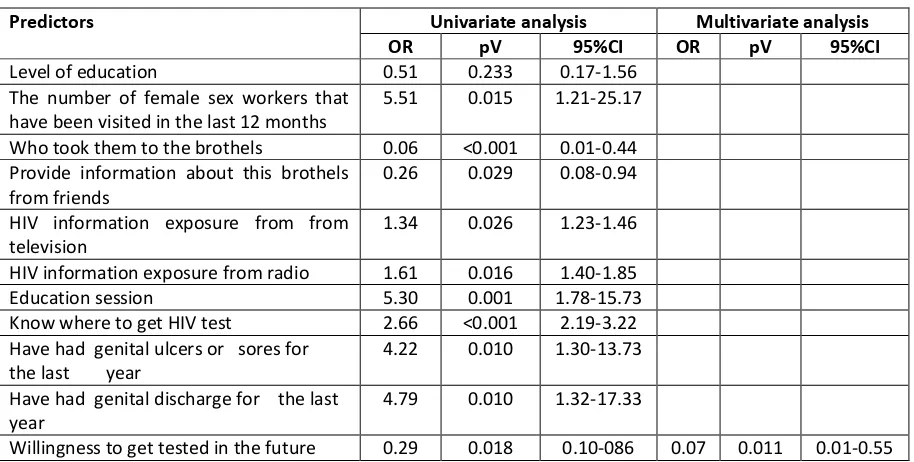
Analysis was conducted to identify factors associated with HIV testing. Several variables, which were considered as factors that might predict HIV testing behaviours were selected. These includes the level of education, the number of female sex workers that have been visited in the last 12 months, the importance of sexual network (such as, who took them to the brothels, and who provide information about this brothels); HIV information exposure from tv, radio, and education session, history of STI symptoms, and willingness to get tested in the future.
19 Table 4.5 Predictors of previous HIV testing
Predictors Univariate analysis Multivariate analysis
OR pV 95%CI OR pV 95%CI
Level of education 0.51 0.233 0.17-1.56 The number of female sex workers that
have been visited in the last 12 months
5.51 0.015 1.21-25.17
Who took them to the brothels 0.06 <0.001 0.01-0.44 Provide information about this brothels
from friends
0.26 0.029 0.08-0.94
HIV information exposure from from television
1.34 0.026 1.23-1.46
HIV information exposure from radio 1.61 0.016 1.40-1.85 Education session 5.30 0.001 1.78-15.73 Know where to get HIV test 2.66 <0.001 2.19-3.22
It can be seen from the tables, in univariate analysis, all variables included are significantly related to HIV testing, except education level.
However, in the multivariate analysis, factors that predict HIV testing was only willingness to get tested in the future.
Discussion
This study was aimed at identifying the sexual related risk behaviours and experiences among clients of sex workers and analysing factors associated with HIV testing among this group. Mixed research method was conducted by surveying 200 clients of sex workers in the brothels area, and conducted a follow up interview with limited number of sample.
This study shows that the clients of sex workers came from a range of sociodemographic characteristics background and with varying sexual risk related behaviours.
More than half of the participants are currently married, and at 18% of the respondents admitted that in addition to having a sexual relationship with sex workers, and wives, they also had other relations their occasional non-commercial sex partners. Multiple sexual relationship among clients of sex workers are common.15 The heavy multiple sexual relationship, suggest the important roles of the
20 The fact that the two most common origin were from java and Bali, and the significant percentage of them were married but not living with their spouses suggested that HIV interventions programs need to be tailored that fitted with the living conditions of migrant workers with lack of supports from close relatives which push them more at risk of engaging in HIV related risky behaviours. Study among migrants in Mexico revealed the specific vulnerability of this group in HIV transmission, and the needs to address this with distinctive approaches.17
While the mean of sex workers clients are 39 years old, the age ranging from 17 -77 years old. In addition, while the majority of the participants had married at the age between 23 and 30, however their sexual debut had started long before that age. These two facts suggestive of the need to reach a younger group populations for HIV interventions.
It is interesting to note that the frequency of the use of condom were different with the type of partner. The least frequent condom use were with their regular non commercial sex partners and it was most frequent use was with commercial sex partners. While there were two common reasons for not using condoms were shared within these three types of partners, i.e perceived of unnecessary and did not like it, the differences in condom use frequency among this three types of partners indicates that suggest that the level of condom were decreasing as the level of trust increase. This consistent difficulties in encouraging the use of condom within the long term partnership were not uncommon.18
Only a small percentage of the participants have had an HIV test, and this is much lower than those found in other settings.19 Factors that predict HIV testing in the univariate analysis were the number
of female sex workers visited in the last 12 months, if they came to the brothels with friends, if they know about the brothels information from their friends, have attended education sessions, know where to get HIV test, willingness to get tested in the future, and have had a history of genital ulcer and genital discharge. However, only willingness to get tested in the future was significantly associated with history of HIV testing.
21 This study also highlights the importance of social network in shaping the HIV protective behaviours. Those who came to the brothels with friends and knew the existence of the brothels from friends were more likely to had HIV tested in the univariate analysis, though this association was not significant in multivariate analysis. In this study, almost all of the respondents reported that they knew about the existence of the brothels from their friends, and more than half of the participants admitted that they went to the brothels with their friends, indicating that peers were the potential outreach workers to expose clients of sex workers with HIV information. Peer based HIV programs have been identified among effective HIV interventions targeting men at risk.20
While knowing where to get tested were among the factors that is associated with HIV testing the univariate analysis, only 39.5 percent of the participants know where to get tested. This highlighted the needs to widespread the VCT testing venues among this group. And this also highlight the need to explore the methods of scaling up VCT testing beyond a facility based HIV services. A mobile VCT testing conducted in brothels areas, have proved to increase awareness and willingness of men to get tested.19 A systematic review conducted recently confirmed the significant contribution of non-facility
based HIV testing in improving the scaling up HIV testing among high risk and low risk groups around the world.21
Finally, only willingness to get tested in the future was associated with the past history of HIV testing. This might suggest that once they seek VCT test and demystify the difficulties and stigma around HIV testing, their acceptance for future HIV test will be more likely. This is important especially for high risk group of HIV where their behaviours often require them to seek repeat test.
Conclusions
22
APPENDIX
Appendix 1 Test and treatment facility
Clinics Yayasan Kerti Praja (YKP), Denpasar, Bali
23
Appendix 2 Study team
No. Name/NIDN Institution Expertise area Job Descriptions
1 dr. Pande Putu Januraga, M.Kes, DrPH
FK Unud Public health Design the study and instrument as well as coordinating data management and analysis 2 Prof. dr. IDN
Wirawan, MPH
FK Unud Epidemiology Supervise the development of study design and quantitative instruments
3 dr. Luh Putu Lila Wulandari, MPH
FK Unud Public Health Assist PI with qualitative design, data collection and analysis 4 dr. AAS Sawitri,
MPH
FK Unud Epidemiology Assist PI with quantitative design, data collection and analysis
6 Prof David Cooper Kirby Institute, UNSW, data analysis. Prof Cooper also is responsible to supervise
24
25
26
27
28
29
REFERENCES
1. MOH of Indonesia. Mathematic Model of HIV Epidemic in Indonesia 2008-2014. Jakarta: Ministry of Health Of Indonesia; 2008.
2. NAC of Indonesia. Indonesia country report on the follow up to the declaration of commitment on HIV-AIDS (UNGASS). Jakarta: NAC of Indonesia; 2012.
3. Januraga P, Wulandari L, Muliawan P, et al. Sharply rising prevalence of HIV infection in Bali: a critical assessment of the surveillance data. International journal of STD & AIDS.
2013;24(8):633-637.
4. Anshori Y. Pemberdayaan Pokja Lokasi dengan melibatkan Mucikari dalam mereduksi IMS/HIV: Sebuah Model Intervensi Struktural di Bali. Denpasar: Bali AIDS Comittee; 2012. 5. NAC of Indonesia. Panduan Nasional Program Pencegahan HIV melalui Transmisi Seksual
(National Guidelines for HIV Prevention Programs by Sexual Transmission). Jakarta: National AIDS Committee of Indonesia; 2011.
6. Espirito Santo M, Etheredge G. How to reach clients of female sex workers: a survey" by surprise" in brothels in Dakar, Senegal. Bulletin of the World Health Organization.
2002;80(9):709-713.
7. Voeten HA, Egesah OB, Ondiege MY, Varkevisser CM, Habbema JDF. Clients of female sex workers in Nyanza province, Kenya: a core group in STD/HIV transmission. Sexually transmitted diseases. 2002;29(8):444-452.
8. MOH of Indonesia. Integrated Biological - Behavioral Surveillance of Most-at-Risk-Groups (MARG): Ministry of Health Republic Indonesia; 2007.
9. MOH of Indonesia. Integrated Biological - Behavioral Surveillance of Most-at-Risk-Groups (MARG): Ministry of Health Republic Indonesia; 2009.
10. MOH of Indonesia. Integrated Biological - Behavioral Surveillance of Most-at-Risk-Groups (MARG): Ministry of Health Republic Indonesia; 2011.
11. Hor LB, Detels R, Heng S, Mun P. The role of sex worker clients in transmission of HIV in Cambodia. International journal of STD & AIDS. 2005;16(2):170-174.
12. Lowndes CM, Alary M, Labbe A-C, et al. Interventions among male clients of female sex workers in Benin, West Africa: an essential component of targeted HIV preventive interventions. Sexually transmitted infections. 2007;83(7):577-581.
13. Liamputtong P. Qualitative research methods: Oxford University Press; 2009.
14. Liamputtong P. Researching the vulnerable: A guide to sensitive research methods: Sage Publications Limited; 2006.
15. Remple VP, D. M. Patrick, C. Johnston, M. W. Tyndall, Jolly. AM. Clients of Indoor
Commercial Sex Workers: Heterogeneity in Patronage Patterns and Implications for HIV and STI Propagation through Sexual Networks. Sexually Transmitted Diseases. 2007;34:754–760. 16. Alary M, Lowndes CM, Mukenge-Tshibaka L, et al. Sexually transmitted infections in male
clients of female sex workers in Benin: Risk factors and reassessment of the leucocyte esterase dipstick for screening of urethral infections. Sexually Transmitted Infections.
2003;79(5):388-392.
17. Martinez-Donate AP, Hovell MF, Rangel MG, et al. Migrants in Transit: The Importance of Monitoring HIV Risk Among Migrant Flows at the Mexico–US Border. American Journal of Public Health. 2015/03/01 2015;105(3):497-509.
18. Aral SO, N. S. Padian, Holmes KK. Advances in Multilevel Approaches to Understanding the Epidemiology and Prevention of Sexually Transmitted Infections and HIV: An Overview. The Journal of Infectious Diseases 2005;191((Suppl. 1): S1–S6).
19. Diserens EA, Bodenmann P, N'Garambe C, et al. Clients of sex workers in Switzerland: it makes sense to counsel and propose rapid test for HIV on the street, a preliminary report.
30 20. Schneider JA, McFadden RB, Laumann EO, Prem Kumar SG, Gandham SR, Oruganti G.
Candidate change agent identification among men at risk for HIV infection. Social Science & Medicine.75(7):1192-1201.
21. Suthar AB, Ford N, Bachanas PJ, et al. Towards Universal Voluntary HIV Testing and