Table of contents
Introduction
Global monitoring framework Global targets for NCDs Setting national targets
Reporting on the global NCD indicators
Indicators by Categorization Mortality and morbidity:
1. Premature NCD Mortality 2. Cancer incidence
Behavioural Risk Factors:
3. Harmful use of alcohol: Adult Per Capita Consumption 4. Harmful use of alcohol: heavy episodic drinking
5. Harmful use of alcohol: alcohol-related morbidity and mortality 6. Physical inactivity in adolescents
7. Physical inactivity in adults 8. Salt intake
9. Tobacco use in adolescents 10. Tobacco use in adults
Biological Risk Factors:
11. a) Blood pressure: raised blood pressure 11.b) Blood pressure: mean blood pressure 12. Raised blood glucose/diabetes 13. Overweight and obesity in adolescents 14. Overweight and obesity in adults 15. Saturated fat
16. Low fruit and vegetable consumption 17. a) Total Cholesterol: raised
17.b) Total Cholesterol: mean
National Systems Response:
18. Drug therapy and counselling to prevent heart attacks and stroke 19. Essential medicines and technologies for NCD
20. Palliative care
21. Elimination of trans-fats 22. Vaccination for HPV 23. Marketing to children 24. Vaccination for Hepatitis B 25. Cervical cancer screening
Introduction:
In May 2013 the 66th World Health Assembly adopted the comprehensive global monitoring framework (GMF) for the prevention and control of noncommunicable diseases. The Global Monitoring Framework included a set of indicators capable of application across regions and country settings to monitor trends and assess progress made in the
implementation of national strategies and plans on noncommunicable diseases.
The purpose of this document is to provide detailed guidance to Member States so they can correctly measure each of the 25 indicators and monitor their progress over time. For each indicator, a complete definition is provided,
appropriate data sources are identified and a detailed calculation, where applicable, is provided.
Global Monitoring Framework:
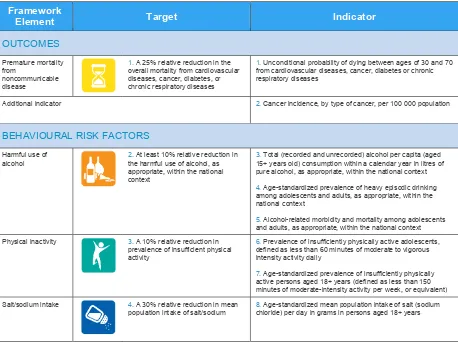
Member States have agreed 25 indicators across three areas which focus on the key outcomes, risk factors and national systems response needed to prevent and control NCDs. (see figure 1).
Figure 1. Global Monitoring Framework
Framework overall mortality from cardiovascular diseases, cancer, diabetes, or chronic respiratory diseases
1. Unconditional probability of dying between ages of 30 and 70 from cardiovascular diseases, cancer, diabetes or chronic respiratory diseases
Additional indicator 2. Cancer incidence, by type of cancer, per 100 000 population
BEHAVIOURAL RISK FACTORS
Harmful use of alcohol
2. At least 10% relative reduction in the harmful use of alcohol, as appropriate, within the national context
3. Total (recorded and unrecorded) alcohol per capita (aged 15+ years old) consumption within a calendar year in litres of pure alcohol, as appropriate, within the national context 4. Age-standardized prevalence of heavy episodic drinking among adolescents and adults, as appropriate, within the national context
5. Alcohol-related morbidity and mortality among adolescents and adults, as appropriate, within the national context Physical inactivity 3. A 10% relative reduction in
prevalence of insufficient physical activity
6. Prevalence of insufficiently physically active adolescents, defined as less than 60 minutes of moderate to vigorous intensity activity daily
Tobacco use 5. A 30% relative reduction in prevalence of current tobacco use
9. Prevalence of current tobacco use among adolescents 10. Age-standardized prevalence of current tobacco use among persons aged 18+ years
BIOLOGICAL RISK FACTORS
Raised blood pressure
6. A 25% relative reduction in the prevalence of raised blood pressure or contain the prevalence of raised blood pressure, according to national circumstances
11. Age-standardized prevalence of raised blood pressure among persons aged 18+ years (defined as systolic blood
pressure ≥140 mmHg and/or diastolic blood pressure ≥90
mmHg) and mean systolic blood pressure Diabetes and obesity 7. Halt the rise in diabetes & obesity 12. Age-standardized prevalence of raised blood
glucose/diabetes among persons aged 18+ years (defined as
fasting plasma glucose concentration ≥ 7.0 mmol/l (126 mg/dl) or on medication for raised blood glucose)
13. Prevalence of overweight and obesity in adolescents (defined according to the WHO growth reference for school-aged children and adolescents, overweight – one standard deviation body mass index for age and sex, and obese – two standard deviations body mass index for age and sex) 14. Age-standardized prevalence of overweight and obesity in
persons aged 18+ years (defined as body mass index ≥ 25 kg/m² for overweight and body mass index ≥ 30 kg/m² for obesity)
Additional indicators 15. Age-standardized mean proportion of total energy intake from saturated fatty acids in persons aged 18+ years 16. Age-standardized prevalence of persons (aged 18+ years) consuming less than five total servings (400 grams) of fruit and vegetables per day
17. Age-standardized prevalence of raised total cholesterol among persons aged 18+ years (defined as total cholesterol
≥5.0 mmol/l or 190 mg/dl); and mean total cholesterol
concentration receive drug therapy and counselling (including glycaemic control) to prevent heart attacks and strokes
18. Proportion of eligible persons (defined as aged 40 years and older with a 10-year cardiovascular risk ≥30%, including those with existing cardiovascular disease) receiving drug therapy and counselling (including glycaemic control) to prevent heart attacks and strokes affordable basic technologies and essential medicines, including generics required to treat major noncommunicable diseases in both public and private facilities
19. Availability and affordability of quality, safe and efficacious essential noncommunicable disease medicines, including generics, and basic technologies in both public and private facilities
Additional indicators 20. Access to palliative care assessed by morphine-equivalent 21. Adoption of national policies that limit saturated fatty acids and virtually eliminate partially hydrogenated vegetable oils in the food supply, as appropriate, within the national context and national programmes
22. Availability, as appropriate, if cost-effective and affordable, of vaccines against human papillomavirus, according to national programmes and policies
23. Policies to reduce the impact on children of marketing of foods and non-alcoholic beverages high in saturated fats, trans fatty acids, free sugars, or salt
Global Targets for NCDs:
Nine areas have been selected from the 25 indicators in the Global Monitoring Framework to be targets (see figure 2): one mortality target (previously agreed at the WHA in May 2012); six risk factor targets (harmful use of alcohol, physical inactivity, dietary sodium intake, tobacco use, raised blood pressure, and diabetes and obesity), and two national systems targets (drug therapy to prevent heart attacks and strokes, and essential NCD medicines and technologies to treat major NCDs). The targets are both attainable and significant, and when achieved will represent major
accomplishments in NCD and risk factors reductions. The global NCD targets are intended to focus global attention on NCDs and would represent a major contribution to NCD prevention and control. Targets have been set for 2025, with a baseline of 2010.
Figure 2. Global voluntary targets for NCDs
A 25% relative reduction in risk of premature mortality from cardiovascular diseases, cancer, diabetes, or chronic respiratory diseases
At least 10% relative reduction in the harmful use of alcohol
A 10% relative reduction in prevalence of insufficient physical activity
A 30% relative reduction in mean population intake of salt/sodium
A 30% relative reduction in prevalence of current tobacco use
A 25% relative reduction in the prevalence of raised blood pressure or contain the prevalence of raised blood pressure, according to national circumstances
Halt the rise in diabetes and obesity
At least 50% of eligible people receive drug therapy and counselling (including glycaemic control) to prevent heart attacks and strokes
Setting National Targets:
Member States are strongly encouraged to consider the development of national targets based on their own national situations, which build on the nine global voluntary targets. Setting targets is a way to draw attention to NCDs and help mobilize resources to address NCD priorities. National targets may need to be adapted from the global targets if a country has already achieved a target or if the global target is too low given the progress already achieved within the country.
As a starting point, Member States interested in setting national NCD targets are encouraged to consider the following:
• Are the targets and indicators included in the GMF all suitable in the national context?
• Are there additional targets and indicators needed for the country?
• Are the systems in place to track these 25 global indicators and report on nine global targets? And systems which track any new proposed ones?
• What is the current level of exposure/mortality/service provision?
• Are the reductions or coverage proposed for global targets appropriate in the national context or should they be more ambitious?
Reporting on the Global NCD Indicators:
WHO is mandated to prepare regular updates on the progress towards achieving the nine global NCD targets and the status globally in relation to the 25 indicators included in the Global Monitoring Framework. To enable these reports to be as comprehensive as possible, Member States are strongly encouraged to submit data to WHO on a regular basis to enable analysis of the global status of NCD targets and indicators. For ease of data submission, WHO has prepared a template for reporting against the NCD indicators. This template is available upon request from WHO by contacting:
Where multiple indicators exist for one target (i.e. for alcohol), Member States should endeavor to report against as many indicators as possible. However they should also choose to report against the one most appropriate for their national circumstances.
It is important to note that WHO will continue to produce figures for each country that are comparable across all Member States. While these comparable figures will be based on the data submitted by Member States, they will also take into consideration differences across countries in data availability, data type, population structure and other data characteristics that reduce comparability across countries. Thus, the figures produced by WHO may differ from those reported by each individual Member State.
Name abbreviated
Premature NCD Mortality
Indicator name Unconditional probability of dying between ages 30 and 70 years from cardiovascular diseases, cancer, diabetes, or chronic respiratory diseases
Definition Probability of dying between the exact ages 30 and 70 years from cardiovascular diseases, cancer, diabetes, or chronic respiratory diseases. Deaths from these four causes will be based on the following ICD codes: I -I , C -C , E -E , and J30-J98.
Age-specific death rates for the combined four cause categories (typically in terms of 5-year age groups 30- ,…, -69). A life table method allows calculation of the risk of death between exact ages 30 and 70 from any of these causes, in the absence of other
auses of death. The ICD odes to e i luded i the al ulatio a e: a dio as ula
disease: I -I , Ca e : C -C , Dia etes: E -E , Chronic respiratory: J30-J98. To calculate age-specific mortality rate for each five-year age group and country, for each 5-year age range between 30 and 70:
Then translate the 5-year death rate to the probability of death in each 5-year age range:
The probability of death from age 30 to age 70, independent of other causes of death can be calculated as:
Preferred data sources Vital registration systems which record deaths with sufficient completeness to allow estimation of all-cause death rates.
Other possible data sources Sample registration systems; verbal autopsy. NCD Framework Outcome
Disaggregation Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
Annual
Limitations Potential limitations include:
- incomplete or unusable death registration data
Name abbreviated
Cancer incidence
Indicator name Cancer incidence, by type of cancer
Definition Number of new cancers of a specific site/type occurring in the population per year, usually expressed as the number of new cancers per 100,000 population.
Method of
estimation/calculation
� � � �
At-ri � ℎ × ,
Numerator Number of new cancer cases diagnosed in a specific year. This may include multiple primary cancers occurring in one patient. The primary site reported is the site of origin and not the metastatic site. In general, the incidence rate would not include recurrences. Denominator At-risk population for the given category of cancer. The population used depends on the
rate to be calculated. For cancer sites that occur in only one sex, the sex-specific population (e.g., females for cervical cancer) is used.
Preferred data sources Population-based cancer registries, which collect and classify information on all new cases of cancer in a defined population
Other possible data sources
NCD Framework Outcome
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
Annual
Limitations Potential limitations include: - incomplete records
- inadequate coverage of registries
Data type Rate
Related links http://globocan.iarc.fr/
Name abbreviated
Harmful use of alcohol: Adult Per Capita Consumption
Indicator name Total (recorded and unrecorded) alcohol per capita (APC) (15+ years old) consumption within a calendar year in litres of pure alcohol
Definition Consumption of pure alcohol (ethanol) in litres per person aged 15+ during one calendar year.
Method of
estimation/calculation
ℎ � � �
� � � + ℎ
Numerator Sum of recorded and unrecorded alcohol consumed in a population during a calendar year, in litres.
Denominator Midyear resident population aged 15+ for the same calendar year.
Preferred data sources Administrative reporting systems for recorded APC and survey data for unrecorded APC. The priority of data sources for recorded alcohol per capita consumption should be given to government statistics on sales of alcoholic beverages during a calendar year or data on production, export and import of alcohol in different beverage categories. For countries, where the governmental sales or production data is not available, the preferred data source would be country specific and publicly available data from the private sector, including alcohol producers or country specific data from the Food and Agriculture Organization of the United Nations statistical database (FAOSTAT), which may also include the estimates of unrecorded alcohol consumption. For main categories of alcohol
e e ages Bee i ludes alt ee s, Wi e i ludes i e ade f o g apes, “pi its i lude all distilled e e ages, a d Othe i ludes o e o se e al othe al oholi
beverages, such as fermented beverages made from sorghum, maize, millet, rice, or cider, fruit wine, fortified wine, etc. Data sources for unrecorded alcohol consumption include survey data, FAOSTAT data, other data sources such as customs or police data, and expert opinions.
Other possible data sources Data sets of FAO and UN Statistical office NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
Annual
Limitations Potential limitations include:
- incomplete administrative records
- bias through self-report, including under-reporting of alcohol consumption - misunderstanding/ -interpretation of questions and/ or size of a standard drink - limited validity of survey instruments
Data type Volume
Name abbreviated
Harmful use of alcohol: heavy episodic drinking
Indicator name Age-standardized prevalence of heavy episodic drinking
Definition Heavy episodic drinking among adults is defined as those who report drinking 6 (60 grams) or more standard drinks in a single drinking occasion
Method of
estimation/calculation
� � �
ℎ � ℎ
�
x
%
Numerator Number of persons reporting consuming 60 grams or more of pure alcohol on at least one occasion monthly
Denominator All respondents of the survey
Preferred data sources Population-based (preferably nationally representative) survey Other possible data
sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of
data collection
At least every 5 years
Limitations Potential limitations include:
- bias through self-report, including under-reporting of alcohol consumption - misunderstanding/ -interpretation of questions and/ or size of a standard drink - limited validity of survey instruments
Data type Prevalence
Name abbreviated
Harmful use of alcohol: alcohol-related morbidity and mortality
Indicator name Alcohol-related morbidity and mortality among adolescents and adults (monitored by alcohol use disorders).
Definition Adults (15+ years) who suffer from disorders attributable to the consumption of alcohol (according to ICD-10: F10.1 Harmful use of alcohol; F10.2 Alcohol dependence) during a given calendar year.
Method of
estimation/calculation
� + � ℎ
� � � . � . �
� + x100%
Numerator Number of adults (15+ years) with a diagnosis of F10. or F10.2 during a calendar year. Using the algorithms specified in the validated instruments, presence or absence of harmful use of alcohol or alcohol dependence can be determined. AUD will be scored if either disease category is present.
Denominator All respondents of the survey aged 15+ years.
Preferred data sources Population-based (preferably nationally representative) survey using validated instruments
Other possible data sources Additional health services reporting systems may provide complementary or confirmatory information regarding to the frequency and severity of alcohol use
Disorders.
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include:
-bias through self-report, including under-reporting - misunderstanding/ -interpretation of questions - limited validity of survey instruments
Data type Prevalence
Name abbreviated
Physical inactivity in adolescents
Indicator name Prevalence of insufficiently physically active adolescents
Definition Percentage of adolescents participating in less than 60 minutes of moderate to vigorous intensity physical activity daily.
Adolescents are defined as 10 – 19 year olds or according to country definition.
Method of
estimation/calculation
ℎ ℎ
� ℎ < �
� � � � � � <
x %
Numerator Number of respondents for whom the number of days per week with <60 minutes of moderate to vigorous intensity activity is <7 days
Denominator All adolescent respondents of the survey
Preferred data sources School-based or population-based (preferably nationally representative) survey Other possible data
sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of
data collection
At least every 5 years
Limitations Potential limitations include:
- bias through self-report, including over-reporting of activity
- misunderstanding/ -interpretation of questions and/ or intensity of physical activity - limited validity of survey instruments
Data type Prevalence
Related links http://who.int/chp/gshs/en/
Name abbreviated
Physical inactivity in adults
Indicator name Age-standardized prevalence of insufficiently physically active persons aged 18+ years
Definition Percentage of adults aged 18+ years not meeting any of the following criteria:
– 150 minutes of moderate-intensity physical activity per week
– 75 minutes of vigorous-intensity physical activity per week
– an equivalent combination of moderate- and vigorous-intensity physical activity accumulating at least 600 MET-minutes* per week
Minutes of physical activity can be accumulated over the course of a week but must be of a duration of at least 10 minutes.
*MET refers to metabolic equivalent. It is the ratio of a person's working metabolic rate relative to the resting metabolic rate. One MET is defined as the energy cost of sitting quietly, and is equivalent to a caloric consumption of 1 kcal/kg/hour. Physical activities are frequently classified by their intensity, using the MET as a reference.
Method of
estimation/calculation
+ � ℎ
� � � ℎ � � �
+ x %
Numerator Number of respondents where all 3 of the following criteria are true: (1) Weekly minutes* of vigorous activity < 75 mins.
(2) Weekly minutes* of moderate activity < 150 mins. (3) Weekly MET-minutes** < 600.
* Weekly minutes is calculated by multiplying the number of days on which
vigorous/moderate is done by the number of minutes of vigorous/moderate activity per day.
** Weekly MET-minutes is calculated by multiplying the weekly minutes of vigorous activity by 8 and the number of weekly minutes of moderate activity by 4 and then adding these two results together.
Denominator All respondents of the survey aged 18+ years.
Preferred data sources Population-based (preferably nationally representative) survey Other possible data sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include:
- bias through self-report, including over-reporting of activity
Data type Prevalence
Related links http://www.who.int/chp/steps/GPAQ/en/ http://www.who.int/chp/steps/en/index.html
Name abbreviated
Salt intake
Indicator name Age-standardized mean population intake of salt (sodium chloride) per day in grams in persons aged 18+ years
Definition Mean population intake of salt in grams
Method of
estimation/calculation
� � � � +
+
Numerator Sum of sodium excretion in urine samples from all respondents aged 18+years. The gold-standard for estimating salt intake is through 24-hour urine collection, however other methods such as spot urines and food frequency surveys may be more feasible to administer at the population level.
Denominator All respondents of the survey aged 18+ years.
Preferred data sources Population-based (preferably nationally representative) survey Other possible data sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include: - measurement error
Data type Mean
Related links http://www.who.int/chp/steps/en/index.html
Name abbreviated
Tobacco use in adolescents
Indicator name Prevalence of current tobacco use among adolescents
Definition Percentage of adolescents who currently use any tobacco product (smoked or
smokeless). “ oked to a o p odu ts i ludes the o su ptio of iga ettes, idis, cigars, cheroots, pipes, shisha (water pipes), fine-cut smoking articles (roll-your-own), krekets, and any other form of smoked tobacco.
"Smokeless tobacco" includes moist snuff, plug, creamy snuff, dissolvables, dry snuff, gul, loose leaf, red tooth powder, snus, chimo, gutkha, khaini, gudakhu, zarda, quiwam, dohra, tuibur, nasway, naas/naswar, shammah, betel quid, toombak, pan (betel quid),
i ’ ik, ish i, tapkee , to ol a d a other tobacco product that is sniffed, held in the
mouth, or chewed.
Adolescents are defined as 10 – 19 year olds or according to country definition. Method of non-daily users of smoked or smokeless tobacco.
Denominator All adolescent respondents of the survey.
Preferred data sources School-based or population-based (preferably nationally representative) survey
Other possible data sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include:
- bias through self-report, including under-reporting of tobacco use - misunderstanding/ -interpretation of questions
- limited validity of survey instruments Data type Prevalence
Related links http://www.who.int/tobacco/surveillance/gyts/en/ http://who.int/chp/gshs/en/
Name abbreviated
Tobacco use in adults
Indicator name Age-standardized prevalence of current tobacco use among persons aged 18+ years
Definition “ oked to a o p odu ts i ludes the o su ptio of iga ettes, idis, iga s, he oots, pipes, shisha (water pipes), fine-cut smoking articles (roll-your-own), krekets, and any other form of smoked tobacco.
"Smokeless tobacco" includes moist snuff, plug, creamy snuff, dissolvables, dry snuff, gul, loose leaf, red tooth powder, snus, chimo, gutkha, khaini, gudakhu, zarda, quiwam, dohra, tuibur, nasway, naas/naswar, shammah, betel quid, toombak, pan (betel uid , i ’ ik, ish i, tapkeer, tombol and any other tobacco product that is sniffed, held in the mouth, or chewed. Method of non-daily users or smoked or smokeless tobacco.
Denominator All respondents of the survey aged 18+ years.
Preferred data sources Population-based (preferably nationally representative) survey Other possible data
sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of
data collection
At least every 5 years
Limitations Potential limitations include:
- bias through self-report, including under-reporting of tobacco use - misunderstanding/ -interpretation of questions
- limited validity of survey instruments - representativeness of the sample Data type Prevalence
Related links http://www.who.int/tobacco/surveillance/survey/gats/en/ http://www.who.int/chp/steps/en/index.html
Name abbreviated
Tobacco use in adults
Definition
Name abbreviated
Raised blood pressure
Indicator name Age-standardized prevalence of raised blood pressure among persons aged 18+ years
Definition “ stoli lood p essu e ≥ a d/o diastoli lood p essu e ≥ a o g pe so s aged + years.
Method of
estimation/calculation
+ � ℎ �
≥ � � � ≥ �
+ x %
Numerator Number of respondents with systolic blood pressure ≥140mmHg or diastolic blood pressure
≥90mmHg. Ideally three blood pressure measurements should be taken and the average systolic and diastolic readings of the second and third measures should be used in this calculation.
Denominator All respondents of the survey aged 18+ years.
Preferred data sources Population-based (preferably nationally representative) survey in which blood pressure was measured, not self-reported.
Other possible data sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of
data collection
At least every 5 years
Limitations Potential limitations include: - measurement error
- representativeness of the sample
Data type Prevalence
Name abbreviated
Mean blood pressure
Indicator name Age-standardized mean systolic blood pressure in persons aged 18+ years
Definition Mean systolic blood pressure in persons aged 18+ years
Method of
estimation/calculation
� +
+
Numerator Sum of systolic blood pressure from all participants aged 18+ years. Ideally three blood pressure measurements should be taken and the average systolic reading of the second and third measures should be used in this calculation.
Denominator All respondents of the survey aged 18+ years.
Preferred data sources Population-based (preferably nationally representative) survey in which blood pressure was measured, not self-reported.
Other possible data sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include: - measurement error
- representativeness of the sample
Data type Mean
Name abbreviated
Raised blood glucose/diabetes
Indicator name Age-standardized prevalence of raised blood glucose/diabetes among persons aged 18+ years or on medication for raised blood glucose
Definition Fasti g plas a glu ose alue ≥ . ol/L g/dl o o edi atio fo aised lood glucose among adults aged 18+ years.
Method of
estimation/calculation
+ � ℎ �
≥ . / mg/dl or � � �
+ x %
Numerator Number of respondents aged 18+ years with fasting plasma glucose value ≥7.0 mmol/L (126 mg/dl) or on medication for raised blood glucose. Fasting blood glucose must be measured, not self-reported, and measurements must be taken after the person has fasted for at least eight hours.
Denominator All respondents of the survey aged 18+ years.
Preferred data sources Population-based (preferably nationally representative) survey. There are two main blood chemistry screening methods- dry and wet chemistry. Dry chemistry uses capillary blood taken from a finger and used in a rapid diagnostic test. Wet chemistry uses a venous blood sample with a laboratory based test. Either method is acceptable. Other possible data sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include: - measurement error
- lack of fasting status
- limited validity of measurement instruments - representativeness of the sample
Data type Prevalence
Name abbreviated
Overweight and obesity in adolescents
Indicator name Prevalence of overweight and obesity in adolescents
Definition According to the WHO growth reference for school-aged children and adolescents, overweight – one standard deviation body mass index for age and sex, and obese – two standard deviations body mass index for age and sex.
Adolescents are defined as 10 – 19 year olds or according to country definition. Method of
estimation/calculation ℎ � ℎ
x %
ℎ
x %
Numerator Number of adolescent respondents who are overweight. Number of adolescent respondents who are obese.
Body mass index (BMI) is calculated by dividing weight in kilograms by height in meters
s ua ed. O e eight is ≥ “D BMI fo age a d se e ui ale t to BMI kg/ ² at
ea s . O ese is ≥ “D BMI fo age a d se e ui ale t to BMI 30kg/m² at 19 years).
Denominator All adolescent respondents of the survey.
Preferred data sources School-based or population-based (preferably nationally representative) survey in which height and weight were measured.
Other possible data sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include: - measurement error
- representativeness of the sample
Data type Prevalence
Name abbreviated
Overweight and obesity in adults
Indicator name Age-standardized prevalence of overweight and obesity in persons aged 18+ years
Definition Bod ass i de ≥ kg/ ² fo o e eight a d od ass i de ≥ kg/ ² fo o esit i adults aged 18+ years.
Method of
estimation/calculation
+ ℎ � ℎ
+ x %
+ ℎ
+ x %
Numerator Number of respondents aged 18+ years who are overweight. Number of respondents aged 18+ years who are obese.
Body mass index (BMI) is calculated by dividing weight in kilograms by height in meters
s ua ed. O e eight is defi ed as ha i g a BMI ≥ kg/ ² a d o esit is defi ed as ha i g a BMI ≥ kg/ ².
Denominator All respondents of the survey aged 18+ years.
Preferred data sources Population-based (preferably nationally representative) survey in which height and weight were measured.
Other possible data sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include: - measurement error
- representativeness of the sample
Data type Prevalence
Name abbreviated
Saturated fat
Indicator name Age-standardized mean proportion of total energy intake from saturated fatty acids in persons aged 18+ years
Definition Mean proportion of total energy intake from saturated fatty acids in persons aged 18+ years
Method of
estimation/calculatio n
� � � � � +
+ %
X100%Numerator Sum of proportion of SFA of total energy intake from all participants aged 18+years. For each participant, divide the saturated fatty acid intake by the total energy intake to get the
proportion of total energy from SFA.
Denominator All respondents of the survey aged 18+ years. Preferred data
sources
Population-based (preferably nationally representative) survey
Other possible data sources
FAO National Food Balance Sheets
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of
data collection
At least every 5 years
Limitations Potential limitations include:
- bias through self-report, including under-reporting of consumption - misunderstanding/ -interpretation of questions
- limited validity of survey instruments Data type Prevalence
Name abbreviated
Low fruit and vegetable consumption
Indicator name Age-standardized prevalence of persons aged 18+ years consuming less than five total servings (400 grams) of fruit and vegetables per day
Definition Percentage of population aged 18+ years who eat less than five servings of fruit and/or vegetables on average per day
Unit of measure A serving of fruit and vegetables is equivalent to 80 grams Method of
Numerator Number of respondents aged 18+ years eating less than 5 servings of fruit and/or vegetables per day. The average number of servings of fruit and/or vegetables is calculated for each participant as follows:
1) Calculate the average number of vegetable servings per week: total number of vegetable servings per day multiplied by number of days per week vegetables are eaten divided by 7. 2) Calculate the average number of fruit servings per week: total number of fruit servings per day multiplied by number of days per week fruit are eaten divided by 7.
3) Sum the average number of vegetable and fruit servings per week.
If this total is less than 5, then the participant is counted in the numerator of the equation as eating less than 5 servings of fruit and/or vegetables per day.
A serving of fruit or vegetables is equivalent to 80 grams. Denominator All respondents of the survey aged 18+ years.
Preferred data sources Population-based (preferably nationally representative) survey Other possible data
sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of
data collection
At least every 5 years
Limitations Potential limitations include: - bias through self-report
- misunderstanding/ -interpretation of questions and/ or portion size of a serving of fruit or Data type Prevalence
Name abbreviated
Raised total cholesterol
Indicator name Age-standardized prevalence of raised total cholesterol among persons aged 18+ years
Definition Total holeste ol ≥ . ol/L g/dl .
Method of
estimation/calculation
+ � ℎ ℎ
≥ . / mg/dl
+ x %
Numerator Number of respondents aged 18+ years with total cholesterol value ≥ 5.0 mmol/L (190 mg/dl).
Denominator All respondents of the survey aged 18+ years.
Preferred data sources Population-based (preferably nationally representative) survey in which cholesterol was measured, not self-reported. There are two main blood chemistry screening methods- dry and wet chemistry. Dry chemistry uses capillary blood taken from a finger and used in a rapid diagnostic test. Wet chemistry uses a venous blood sample with a laboratory based test. Either method is acceptable.
Other possible data sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include:
- measurement error due to insufficient blood sample - limited validity of measurement instruments
representativeness of the sample Data type Prevalence
Name abbreviated
Mean total cholesterol
Indicator name Age-standardized mean total cholesterol among persons aged 18+ years
Definition Mean total cholesterol.
Method of
estimation/calculation
ℎ +
+
Numerator Sum of total cholesterol (in mmol/L or mg/dl) from all participants aged 18+ years. Denominator All respondents of the survey aged 18+ years.
Preferred data sources Population-based (preferably nationally representative) survey in which cholesterol was measured, not self-reported. There are two main blood chemistry screening methods- dry and wet chemistry. Dry chemistry uses capillary blood taken from a finger and used in a rapid diagnostic test. Wet chemistry uses a venous blood sample with a laboratory based test. Either method is acceptable.
Other possible data sources
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include:
- measurement error due to insufficient blood sample - limited validity of measurement instruments
- representativeness of the sample
Data type Mean
Name abbreviated
Drug therapy and counseling to prevent heart attacks and stroke
Indicator name Proportion of eligible persons receiving drug therapy and counseling (including glycaemic control) to prevent heart attacks and strokes
Definition Percentage of eligible persons (defined as aged 40 years and older with a 10-year
a dio as ula disease CVD isk* ≥ %, i ludi g those ith e isti g CVD e ei i g d ug
therapy** and counseling*** (including glycaemic control) to prevent heart attacks and strokes.
*A 10- ea CVD isk of ≥ % is defi ed a o di g to Age, “e , othe ele a t so io -demographic stratifiers where available, blood pressure, smoking status (current smokers OR those who quit smoking less than 1 year before the assessment), total cholesterol, and diabetes (previously diagnosed OR a fasting plasma glucose concentration >7.0 mmol/l (126 mg/dl).
**Drug therapy is defined as taking medication for raised blood glucose/diabetes, raised total cholesterol, or raised blood pressure, or taking aspirin or statins to prevent or treat heart disease.
***Counseling is defined as receiving advice from a doctor or other health worker to quit using tobacco or not start, reduce salt in diet, eat at least five servings of fruit and/or vegetables per day, reduce fat in diet, start or do more physical activity, maintain a healthy body weight or lose weight.
Numerator Number of eligible survey participants who are receiving drug therapy and counseling. See Denominator for definition of eligible people. Receiving drug therapy and counseling is calculated by self-report from respondents reporting they are taking medication for raised blood glucose/diabetes, raised total cholesterol, or raised blood pressure, or taking aspirin or statins to prevent or treat heart disease; and receiving advice from a doctor or other health worker to quit using tobacco or not start, reduce salt in diet, eat at least five servings of fruit and/or vegetables per day, reduce fat in diet, start or do more physical activity, maintain a healthy body weight or lose weight.
Denominator Total number of eligible survey participants. Eligible people are those people aged 40 and older who either currently self-report that they have existing CVD or who have a 10 year cardiovascular risk of 30 per cent or higher calculated by using the WHO/ISH Risk
prediction charts for 14 WHO epidemiological sub-regions which provide the approximate estimates of cardiovascular disease (CVD) risk in people who do not have established coronary heart disease, stroke or other atherosclerotic disease, based on responses to the following: Age, gender, smoking status, SBP, TC and absence or presence of diabetes. Preferred data sources Population-based (preferably nationally representative) survey
Other possible data sources
NCD Framework Risk factor exposure
Limitations Potential limitations include: - bias through self-report
- misunderstanding/ -interpretation of questions - limited validity of survey instruments
- measurement error due to insufficient blood sample - limited validity of measurement instruments
Data type Prevalence
Related links http://www.who.int/chp/steps/en/
Name abbreviated
Essential medicines and technologies for NCD
Indicator name Availability and affordability of quality, safe and efficacious essential noncommunicable disease medicines, including generics, and basic technologies in both public and private facilities
Definition Percentage of public and private primary health care facilities who have all of the following available: Medicines - at least aspirin, a statin, an angiotensin converting enzyme inhibitor, thiazide diuretic, a long acting calcium channel blocker, a beta-blocker, metformin, insulin, a bronchodilator and a steroid inhalant. Technologies - at least a blood pressure measurement device, a weighing scale, blood sugar and blood cholesterol measurement devices with strips and urine strips for albumin assay.
Method of
estimation/calculation
� � � ℎ ℎ � � �
� ℎ � ℎ � � � �
� � � x %
Numerator Number of facilities that have available during assessment the minimum list of essential medicines and basic technologies. The minimum list is: Medicines - at least aspirin, a statin, an angiotensin converting enzyme inhibitor, thiazide diuretic, a long acting calcium channel blocker, a beta-blocker, metformin, insulin, a bronchodilator and a steroid inhalant. Technologies - at least a blood pressure measurement device, a weighing scale, height measuring equipment, blood sugar and blood cholesterol measurement devices with strips and urine strips for albumin assay.
Denominator Number of surveyed facilities.
Preferred data sources Nationally-representative health facility assessment Other possible data sources
NCD Framework National systems response Disaggregation Public, Private
Expected frequency of data collection
At least every 5 years
Limitations
Data type Prevalence
Name abbreviated
Palliative care
Indicator name Access to palliative care assessed by morphine-equivalent consumption of strong opioid analgesics (excluding methadone) per death from cancer
Definition Consumption of morphine-equivalent strong opioid analgesics (excluding methadone) per death from cancer. Morphine- equivalent is a method of standardizing and combining volumes of opioids with differing potencies and is used as a measure of opioid
consumption, which is used as the indicator for access to pain and palliation. Method of
estimation/calculation
� � n-le � ℎ� -e � � � �
ℎ ℎ � �
Numerator Population-level consumption of morphine-equivalent strong opioid analgesics for a given time period. Levels of consumption of opioid medicines in kilograms or grams (for
Fentanyl) are calculated by the INCB on the basis of statistics on manufacture and trade provided by Governments. Consumed quantities include those distributed by wholesalers or manufacturers to retailers (mainly pharmacies and hospitals) plus quantities imported directly by retailers. In countries where the retailers obtain their supply from abroad, quantities declared as imported are considered to be destined for consumption.
Therefore the average reported consumption for the previous three-year period in many cases provides a more accurate estimate of actual consumption since volumes procured in one year may be consumed in the following year.
Morphine-equivalent volumes are calculated as:
(1*morphine)+(83.3*fentanyl)+(5*hydromorphone)+(1.33*oxycodone)+ (0.25*pethidine)
Denominator Number of cancers deaths occurring in the population over the same time period. Preferred data sources Consumption of opioids from International Narcotics Control Board annual reports for
narcotics consumption. Cancer deaths from vital registration systems which record deaths with sufficient completeness to allow estimation of all-cause death rates. Other possible data sources Opioid consumption data from national competent authorities
NCD Framework National systems response Disaggregation None
Expected frequency of data collection
Annual
Limitations Potential limitations include: - incomplete administrative records
- incomplete or unusable death registration data
Name abbreviated
Elimination of trans-fats
Indicator name Adoption of national policies that limit saturated fatty acids and virtually eliminate partially hydrogenated vegetable oils in the food supply, as appropriate, within the national context and national programmes
Definition Adoption of a policy to limit saturated fatty acids and virtually eliminate partially hydrogenated vegetable oils in the food supply.
Method of
estimation/calculation
Country can respond " es" to the uestio Is ou ou t i ple e ti g a atio al policies that limit saturated fatty acids and virtually eliminate industrially produced
trans-fats i.e. pa tiall h d oge ated egeta le oils i the food suppl ?
Preferred data sources WHO NCD Country Capacity Survey Other possible data sources
NCD Framework National systems response Disaggregation None
Expected frequency of data collection
Every 2 years
Limitations Potential limitations include: - bias through self-report
- misunderstanding/ -interpretation of questions - limited validity of survey instruments
Data type Prevalence
Name abbreviated
Vaccination for Human Papillomavirus (HPV)
Indicator name Availability, as appropriate, if cost-effective and affordable, of vaccines against human papillomavirus, according to national programmes and policies
Definition Availability of HPV vaccines as part of a national immunization schedule Method of
estimation/calculation
Country can indicate that they have added HPV vaccine to their national immunization programme, as reflected in their responses to the WHO-UNICEF Joint Reporting Form. Preferred data sources WHO-UNICEF Joint Reporting Form (JRF)
Other possible data sources
NCD Framework National systems response Disaggregation None
Expected frequency of data collection
Annual
Limitations Potential limitations include: - bias through self-report
- misunderstanding/ -interpretation of questions Data type Percentage
Related links http://www.who.int/nuvi/hpv/decision_implementation/en/index.html
http://www.who.int/immunization_monitoring/routine/joint_reporting/en/index.html
Name abbreviated
Name abbreviated
Marketing to children
Indicator name Policies to reduce the impact on children of marketing of foods and non-alcoholic beverages high in saturated fats, trans-fatty acids, free sugars, or salt
Definition Existence of a policy to reduce the impact on children of marketing of foods and non-alcoholic beverages high in saturated fats, trans-fatty acids, free sugars, or salt
Method of
estimation/calculation
Country can respond " es" to the uestio Is ou ountry implementing any policies to reduce the impact on children of marketing of foods and non-alcoholic beverages high in saturated fats, trans-fatt a ids, f ee suga s, o salt?
Preferred data sources WHO NCD Country Capacity Survey Other possible data sources
NCD Framework National systems response Disaggregation None
Expected frequency of data collection
Every 2 years
Limitations Potential limitations include: - bias through self-report
- misunderstanding/ -interpretation of questions - limited validity of survey instruments
Data type Prevalence
Related links http://www.who.int/chp/ncd_capacity/en/
Name abbreviated
Vaccination for Hepatitis B
Indicator name Vaccination coverage against hepatitis B virus monitored by number of third doses of Hep-B vaccine (HepB3) administered to infants
Definition Percentage of one-year-olds who have received three doses of hepatitis B vaccine in a given year.
Unit of measure Doses of Hep-B vaccine (HepB3) administered to infants
Method of measurement Service/facility reporting system /administrative data: Reports of vaccinations performed by service providers (e.g. district health centres, vaccination teams, physicians) are used for estimates based on service/facility records. The estimate of immunization coverage is derived by dividing the total number of vaccinations given by the number of children in the target population, often based on census projections. Household surveys: Survey
ite s o espo d to hild e ’s histo i o e age su e s. The p i iple t pes of su e s
are the Expanded Programme on Immunization (EPI) 30-cluster survey, the UNICEF Multiple Indicator Cluster Survey (MICS), and the Demographic and Health Survey (DHS). The indicator is estimated as the percentage of children ages 12–23 months who received three doses of hepatitis B vaccine either any time before the survey.
Method of
Service/facility reporting system /administrative data:
Household survey data:
Numerator Service/facility reporting system /administrative data:
Total number of hepatitis B vaccinations given to children taken from reports of vaccinations performed by service providers (e.g. district health centres, vaccination teams, physicians).
Household survey data:
Total number of children aged 12-23 months who received three doses of hepatitis B vaccine any time before the survey.
Denominator Service/facility reporting system /administrative data:
Number of children in target population covered by service/facility reporting system/administrative data.
Household survey data:
Other possible data sources
NCD Framework National systems response Disaggregation None
Expected frequency of data collection
Annual
Limitations Potential limitations include:
- subjective methods due to choice of rules - absence of any articulation of uncertainty Data type Prevalence
Name abbreviated
Cervical cancer screening
Indicator name Proportion of women between the ages of 30–49 screened for cervical cancer at least once, or more often, and for lower or higher age groups according to national
programmes or policies
Definition Proportion of women aged 30 - 49 who report they were screened for cervical cancer using any of the following methods: Visual Inspection with Acetic Acid/vinegar (VIA), pap smear and Human Papillomavirus (HPV) test.
Method of
estimation/calculation
- ℎ ℎ �
ℎ � �
- x %
Numerator Number of women aged 30-49 who report ever having had a screening test for cervical cancer using any of these methods: Visual Inspection with Acetic Acid/vinegar (VIA), pap smear and Human Papillomavirus (HPV) test.
Denominator All female respondents aged 30-49.
Preferred data sources Population-based (preferably nationally representative) survey Other possible data sources Facility based data
NCD Framework Risk factor exposure
Disaggregation Age, Sex, other relevant socio-demographic stratifiers where available Expected frequency of data
collection
At least every 5 years
Limitations Potential limitations include:
- bias through self-report, including mistakenly assuming any pelvic exam was a test for cervical cancer
- limited validity of survey instruments
Data type Prevalence
Related links http://www.who.int/chp/steps/en/
Frequently asked questions:
1. What is the comprehensive global monitoring framework?
The Global Monitoring Framework represents an agreement by Member States, adopted in the World Health Assembly in 2013, on a range of indicators and a set of voluntary global targets to track global progress in the prevention and control of noncommunicable diseases.
2. What are the components of the global monitoring framework?
The global monitoring framework has three components of assessment: mortality and morbidity, risk factor exposures, and national systems response needed to prevent and control NCDs.
3. What are the global targets?
Nine areas have been selected by Member States from the 25 indicators to be targets: one mortality target (previously agreed at the WHA in May 2012); six risk factor targets (harmful use of alcohol, physical inactivity, dietary sodium intake, tobacco use, raised blood pressure, and diabetes and obesity), and two national systems targets (drug therapy to
prevent heart attacks and strokes, and essential NCD medicines and technologies to treat major NCDs). The targets are both attainable and significant, and when achieved will represent major accomplishments in NCD and risk factors reductions.
4. How should countries set national targets?
Member States are strongly encouraged consider the development of national targets based on their own national situations, which build on the nine global voluntary targets. National targets may be more or less ambitious than the global ones, and national adaptation should be guided by: current performance in prevention and management of NCDs, current level of NCD-related mortality, risk factor exposure, and NCD oriented programmes, policies and interventions both planned and in place.
As a starting point Member States interested in setting national NCD targets are encouraged to consider the following: Are the targets and indicators included in the GMF all suitable in the national context?
Are there additional targets and indicators needed for the country?
Are the systems in place to track these 25 global indicators and report on nine global targets? And systems which track any new proposed ones?
What is the current level of exposure/mortality/service provision?
Are the reductions or coverage proposed for global targets appropriate in the national context or should they be more or less?
5. What needs to be done when there are multiple indicators for one target? If countries, choose different indicators how can the global reporting be made?
7. What is the reporting cycle? When should countries report, to whom and how?
WHO is mandated to prepare regular updates on the progress towards achieving the nine global NCD targets and the status globally in relation to the 25 indicators included in the Global Monitoring Framework. Interim reports against target achievement are scheduled for 2015 and 2020, with these reports sent to the World Health Assembly in 2016 and 2021.
To enable these reports to be as comprehensive as possible, Member States are strongly encouraged to submit data to WHO on a regular basis, as data becomes available, and ideally at least every 5 years, to enable analysis of the global status of NCD targets and indicators. For ease of data submission, WHO has prepared a template for reporting against the NCD indicators. This template is available upon request from WHO by contacting: [email protected]. 8. What is the reporting mechanism? Is there a template for reporting?
For ease of data submission, WHO has prepared a template for reporting against the NCD indicators. This template is available upon request from WHO by contacting: [email protected].
9. Should countries provide raw data or the summary estimate?
WHO would be pleased to receive either raw data to enable the age-standardized indicators to be calculated or
aggregate data for the relevant variables. Further guidance on this is provided in the reporting template available from WHO.
10. Is it mandatory for all countries to report on all 25 indicators? Or only just for the 9 targets and the country
selected indicators?
It is not mandatory for all countries to report on all 25 indicators, but Member States are strongly encouraged to provide information on the status of all relevant indicators they collect to enable a comprehensive reporting of global status. 11. Will WHO be using secondary data available from other databases and will generate global estimates?
In order to generate the global status of indicators and to facilitate reporting against the 9 global targets, WHO will produce comparable estimates of selected indicators. As with the previous round of estimates, and following WHO's quality standards for data publication, prior to the official release of these updated estimates, WHO will consult its Member States to review, comment and provide advice on the comparable estimates for the selected risk factors and to ensure that latest country data have been identified and used for production of the updated comparable estimates. 12. What is the approach for estimating global status if countries are not able to report?