Dedi Rachmadi, Engkie A Djauharie, Dany Hilmanto, Nanan Sekarwana
Department of Child Health
Faculty of Medicine Universitas Padjadjaran-Rumah Sakit Dr. Hasan Sadikin Bandung
Absract
Dengue hemorrhagic fever (DHF) is the dengue virus infection characterized by plasma leakage as a result of
increased vascular permeability. Consequently, it will influence renal function especially in dengue shock syndrome (DSS). The aim of this study was to assess glomerular filtration rate (GFR) in DHF and DSS. A descriptive study
with cross sectional design was performed in all DHF children who were admitted to Department of Child Health
Dr. Hasan Sadikin Hospital Bandung, from October 2003 to January 2004. Diagnosis of DHF was confirmed
by WHO criteria. The patients were divided into DHF group (grade I and II) and DSS group (grade III and IV).
Glomerular filtration rate was calculated by Schwartz formula from creatinine serum level. The distribution of sex, age, and nutritional status were using chi-square test and the proportion of GFR was used t test. From 68 subjects, 41 (60%) were diagnosed as DHF and 27 (40%) as DSS. There were no significant difference in distribution of sex, age, and nutritional status between DHF and DSS group, each p value was >0.05. Mean GFR in all subjects, DHF, and DSS group were 155.9±47.8, 152.3±49.2, and 161.3±45.9, consecutively. The proportion of GFR between DHF and DSS group was 137.50 (94.8–1318.2) vs. 155.38 (89.2–261.9), p=0.322. In conclusions, all subjects have normal GFR, there is no difference of GFR between DHF and DSS group. [MKB. 2011;43(2S):44S–7]. Key words: Dengue hemorrhagic fever (DHF), dengue shock syndrome (DSS), glomerular filtration rate (GFR)
Fungsi Ginjal pada Demam Berdarah Dengue Anak
AbstrakDemam berdarah dengue (DBD) merupakan infeksi virus dengue, ditandai dengan kebocoran plasma akibat peningkatan permeabilitas vaskular. Berkurangnya aliran darah ke ginjal akan mempengaruhi fungsi ginjal,
terutama pada sindrom syok dengue (SSD). Tujuan penelitian ini untuk menilai laju filtrasi glomerulus (LFG)
pada DBD dan SSD. Penelitian deskriptif dengan rancangan potong silang pada penderita DBD yang datang ke
Departemen Ilmu Kesehatan Anak RS Dr. Hasan Sadikin Bandung, periode Oktober 2003–Januari 2004. Diagnosis
DBD berdasarkan kriteria WHO. Subjek dibagi dalam grup DBD (derajat I dan II) dan SSD (DBD derajat III dan
IV). Penilaian LFG dihitung dari kadar kreatinin serum dengan rumus Schwartz. Perbandingan distribusi jenis
kelamin, usia, dan status nutrisi pada kedua kelompok menggunakan uji chi-kuadrat, sedangkan untuk proporsi
LFG dengan uji t. Dari 68 subjek, grup DBD 41 (60%) dan grup SSD 27 (40%). Tidak ada perbedaan distribusi jenis kelamin, usia, dan satus nutrisi antara grup DBD dan SSD, masing-masing dengan nilai p>0,05. LFG rata-rata grup gabungan, DBD, dan DSS berturut-turut 155,9±47,8; 152,3±49,2; dan 161,3±45,9. Proporsi LFG antara grup DBD dan SSD 137,50 (94,8–131,82) vs 155,38 (89,2–26,9), p=0,322. Simpulan, semua subjek penelitian mempunyai LFG normal dan tidak ada perbedaan antara DBD dan SSD. [MKB. 2011;43(2S):44S–7].
Kata kunci: Laju filtrasi glomerulus (LFG), demam berdarah dengue (DBD), sindrom syok dengue (SSD)
Korespondensi: Dr. Dedi Rachmadi, dr., Sp.A(K), M.Kes, Departemen Ilmu Kesehatan Anak Fakultas Kedokteran Universitas Padjadjaran-Rumah Sakit Dr. Hasan Sadikin, jalan Pasteur No. 38 Bandung 40163, telepon (022) 2035957,
Introduction
Dengue virus infection clinically manifests as dengue fever (DF), dengue hemorrhagic fever (DHF) or dengue shock syndrome (DSS). Dengue hemorrhagic fever (DHF) and DSS are the severe manifestation of dengue virus infection characterized by plasma leakage as a result of increased vascular permeability. Following this leakage, hypovolemic and decrease renal blood perfusion occurs as a consequence of a plasma
volume loss. Consequently, it will influence glomerular filtration rate (GFR) especially in
severe DHF (grade III and IV).
Dengue hemorrhagic fever is a sporadic fever disease, which is characterized by hemorrhage, tends to produce shock and might death.1,2 Capillary
damage allows fluid, electrolyte, and protein to leak into extravascular spaces. This internal redistribution of fluid results in hemoconcentration
and hypovolemia. Hemoconcentration in DHF
patients occur more than 20%.1 Shock is the most
feared complication for DHF patients.3 Shock in
DHF is caused by hypovolemia, and hypovolemia will cause a decrease of cardiac output which in
turn will decrease renal blood flow (RBF). This
reduce in RBF from hypovolemia means that the
fluid balance control system does not work well,
it will lead to renal dysfunction and even acute kidney injury.4
In recent years there has been an increasing report of unusual manifestation of dengue viral infection including renal system involvement. Renal involvement in several cases has been reported usually accompanied with acute kidney injury with or without shock, hemolysis, rhabdomyolysis, and sepsis.3,5 There are a few reports about renal
function in patients with dengue hemorrhagic fever (DHF). Renal dysfunction is manifested by an increase in serum creatinine concentration. Even so, the duration needed from hypovolemia to renal dysfunction is uncertain.4 This study will assess
and wantto know the difference renal function by
examining creatinine level in patients with DHF and DSS when diagnosed for the first time.
Methods
This was an analytic descriptive study with a cross sectional design. The amount of sample
was based on a confidence interval of 95% and a power test of 80%. The subject of this study
were all pediatric DHF patients hospitalized at the Pediatric Department of Dr. Hasan Sadikin Hospital Bandung, from October 2003 to January 2004.
The subject of DHF was fulfilled by WHO
clinical and laboratory criteria, whose parents willing to join and sign the informed consent. The
exclusion criteria for this study were the patients had already received intravenous fluid therapy
by the time DHF was diagnosed, children with dehydration due to diarrhea and vomiting and those with renal disease.
All subjects’ identity was filled, including the general characteristics of name, age, sex, address,
and nutritional status. Dengue hemorrhagic fever
patients were classified as DHF or DSS group. The
serum creatinine concentration was measured by the Jaffe method on admission (from Outpatient or Pediatric Emergency Department) and then the
GFR was calculated by the Schwartz formula.
Ethical approval for this study was obtained from the Ethic Committee of the Faculty Medicine of Padjadjaran University/Dr. Hasan Sadikin Hospital Bandung.
The distribution of sex and nutritional
status in both groups were compared using chi-square test, while the age, length of fever before admitted to hospital, and hematocrit using t test. Data analysis was conducted descriptively for
mean and standard deviation. To compare GFR
value means between DHF and DSS groups were used t test, and p values <0.05 were considered to
indicate statistical significance. Statistic package for social sciences (SPSS) 17.0 computer program
was used to analyze data from this study.
Results
A total number of 68 children with DHF and DSS fulfilled the enrollment criteria.
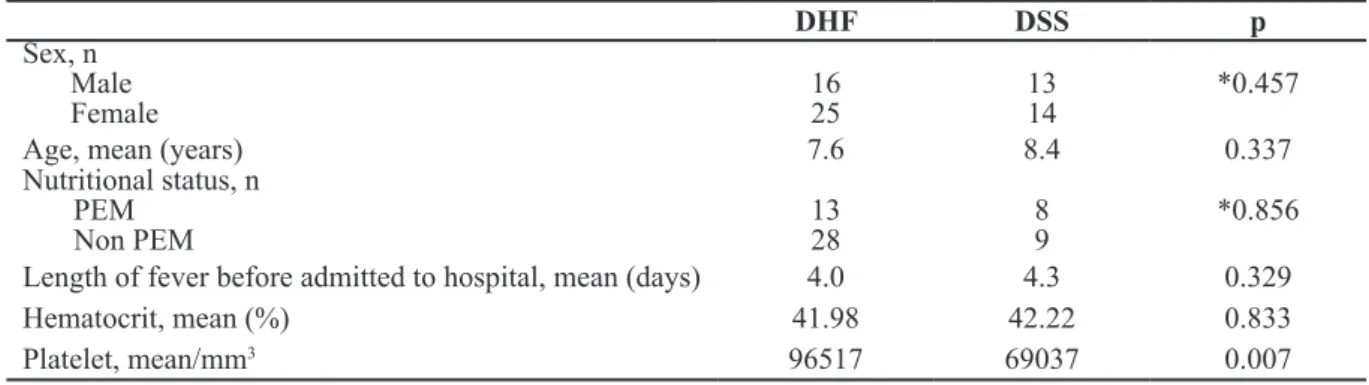
Statistical analysis shows there were no
difference in distribution of sex, age, and
nutritional status, length of fever before admitted to hospital and hematocrit from both DHF and DSS groups. The difference of platelet count
in DHF and DSS was significant (Table 1). All subjects had normal GFR. There was no difference of mean GFR between DHF and DSS
group (Table 2).
Discussion
The World Health Organization criteria for
dengue hemorrhagic fever are fever (2–7 days),
minor or major hemorrhagic manifestations, thrombocytopenia (<100,000/mm3), and objective
evidence of increased capillary permeability (hematocrit increased >20%). Dengue shock syndrome should fulfill these criteria plus
hypotension or narrow pulse pressure (<20 mm
Hg).1,3 All of these features were present in our
described patient studies.
The GFR is clinically important because it
is a measurement of renal function. Measuring serum creatinine is a simple test and it is the most commonly used indicator of renal function.6
Creatinine, as a waste product of metabolism, is
not reused by the body and is normally excreted exclusively by the kidney. Creatinine is also
produced naturally by the body (creatinine is a break-down product of creatine phosphate,
which is found in muscle). It is freely filtered by
the glomerulus, but also actively secreted by the peritubular capillaries in very small amounts such that creatinine clearance overestimates actual
GFR by 10–20%.6 Serum creatinine concentration
will be affect by the following variables: sex, age,
weight, nutritional status, and race.7 In this study
shows there were no difference in distribution of
sex, age, and nutritional status from both DHF
and DSS groups.
The results of this study found that GFR
of DHF and DSS patients were within normal
values according to age and sex. There was no difference in GFR between DHF and DSS patients, p=0.322 (Table 2). It was not in
accordance with the theory that hypovolemia occurred in DHF and DSS patients may caused a major circulation disturbance in all organs including kidney.4,5 Hypovolemia that occurred in
DHF and DSS would cause a decrease in cardiac output which in turn will decrease renal blood
flow (RBF). In more severe cases when degree of plasma leakage is to greater extent, the patients
will have clinical signs of shock. In contrast with our study, the previous studies from small series of patients or case reports. Tanphaichitr et al7 found one case of transient azotemia and
one case of acute renal failure (ARF) among
17 patients with DHF. Mendez and Gonzales8
found 1.6% of (ARF) among 617 children with DHF in Colombia. Lee et al9 reported 4.9% of
ARF in 81 Chinese patients suffering from DHF/
DSS and Abboud10 reported 5% of ARF in DHF.
Other studies, there were eight cases of acute
kidney injury (AKI) reported in patients with
DF5,11 and DSS.3,12 More recently, there were 15
cases of nephropathy dengue has been reported.13
Mostly dengue infection induced renal injury accompanied with syok, rhabdomyolysis, and hypotension. Chotmongkol and Sawanyawisuth14
reported of dengue infection induced renal injury, there was a case of dengue infection induced glomerulonephritis without shock, hypotension, or rhabdomyolysis.
It was assumed that the hypovolemia or shock in our study was so brief that the decreased RBF does not persist, so the circulation system can function well causing no renal damages. It was probably caused by the short lived hypovolemia in DHF patients and the renal autoregulation system causing the kidney as the last organ to be affected by hemodynamic dysfunction.15
According to Vogt and Avner,4 the time needed
from hypovolemia to cause renal dysfunction is still uncertain.
There were no reduces and differences of GFR
in DHF and DSS patients at the time of diagnosis.
Table 1 Characteristics of DHF and DSS
DHF DSS p
Sex, n
Male
Female 1625 1314 *0.457
Age, mean (years) 7.6 8.4 0.337
Nutritional status, n PEM
Non PEM 1328 89 *0.856
Length of fever before admitted to hospital, mean (days) 4.0 4.3 0.329
Hematocrit, mean (%) 41.98 42.22 0.833
Platelet, mean/mm3 96517 69037 0.007
p = t test, *chi-square test
Table 2 GFR in DHF and DSS GFR (n=41)DHF (n=27)DSS Combination(n=68) p* Mean (SD) Median Range 152.30 (49.20) 137.50 94.88–318.21 161.31 (45.88) 155.38 89.17–261.90 155.88 (47.77) 141.89 89.17–318.21 0.322 *Mann Whitney test
The affect of hypovolemia in renal function could not be determined based on serum creatinine level at the time the diagnosis of DHF was
confirmed. Creatinine will not be raised above the normal range until 60% of total kidney function
is lost.6 To ascertain the renal function in DHF
and DSS patients, a more accurate examination
is necessary and repeated that measurement during the course of the illness is needed. Further
study with serial GFR and serum creatinine level
evaluation is needed to make the natural history of DHF and DSS clear. We concluded that there
are no increases and differences of GFR on DHF
and DSS patients at the time of diagnosis.
References
1. World Health Association. Dengue guideline
for diagnosis, treatment, prevention, and control. 3rd edition. Geneva: World Health
Association; 2009.
2. Gibbons RV, Vaughn DW. Dengue: an
escalating problem. BMJ. 2002;324:1563–6.
3. Karakus A, Banga N, Voorn GP, Meinders AJ.
Dengue shock syndrome and rhabdomyolisis.
Neth J Med. 2007;65:78–81.
4. Vogt BA, Avner ED. Renal failure. In:
Behrman RE, Kliegman RM, Arvin AM,
eds. Nelson textbook of pediatrics. 17th ed.
Philadelphia: WB Saunders Co. 2004. p.
1767–71.
5. Nair VR, Unnikrishnan D, Satish B, Sahadulla MI. Case report acute renal failure in dengue fever in the absence of bleeding manifestations or shock. Infect Dis Clin
Pract. 2005;13:142–3.
6. Friedman A. Laboratory assessment and investigation of renal function. In: Avner
ED, Harnon WE, Niaudet P, Yashikawa N,
editors. Pediatric nephrology. 6th ed. Berlin
Heidelberg: Springer-Verlag. 2009. p. 491–
504.
7. Tanphaichitr VS, Chonlasin R, Suwantol
L, Pung-Amritt P, Tachavanich K, Yogsan
S, et al. Effect of red blood cell
glucose-6-phosphate dehydrogenase deficiency on
patients with dengue hemorrhagic fever. J
Med Assoc Thai. 2002;85(Suppl. 2):S522–9. 8. Mendez A, Gonzalez G. Dengue haemorrhagic
fever in children: ten years of clinical
experience. Biomedica. 2003;23:180–93.
9. Lee IK, Liu JW, Yang KD. Clinical
characteristics and risk factors for con-current bacteremia in adults with dengue
hemorrhagic fever. Am J Trop Med Hyg. 2005;72:221–6.
10. Abboud O. Tropical acute renal failure.
3rd Congress of Nephrology in Internet.
(accessed January 2007). Available from:
http:/www.uninet.edu/cin2003/conf/aboud. html.
11. Wiersinga WJ, Scheepstra CG, Kasanardjo
JS, de Vries PJ, Zaaijer H, Geerlings SE.
Dengue fever-induced hemolytic uremic
syndrome. Clin Infect Dis. 2006;43:800–1.
12. Davis JS, Bourke P. Rhabdomyolysis associated with dengue virus infection. Clin
Infect Dis. 2004;38:e109–11.
13. Kimmel PL, Moore J Jr. Viral
glomerulonephritis. In: Schrier RW, editor.
Disease of the kidney and urinary tract. 8th
edition. Philadelphia: Lipincott Williams and Wilkins; 2007. p. 1478–80.
14. Chotmongkol V, Sawanyawisuth K. Case report dengue hemorrhagic fever with
encephalopathy in an adult. Am J Trop Med Hyg. 2004;35:160–3.
15. Greenbaum LA. Pathophysiology of body
fluids and fluid therapy. In: Behrman RE,
Kliegman RM, Jenson HB, editors. Nelson
textbook of pediatrics. 17th ed. Philadelphia:
WB Saunders Co; 2004. p. 191–245.
Dzulfikar D. Lukmanul Hakim, Wiwin Winiar, Herry Garna
Departemen Ilmu Kesehatan Anak, Fakultas Kedokteran, Universitas Padjajaran-Rumah Sakit Dr.
Hasan Sadikin Bandung
Abstrak
Virus dengue dapat menyebabkan infeksi pada semua kelompok usia dengan manifestasi klinis beragam mulai dari asimtomatik, ringan, sampai berat yang biasanya merupakan kasus fatal. Dengue berat ditandai dengan kebocoran plasma, hemokonsentrasi, dan gangguan hemostasis. Penelitian ini bertujuan untuk mengetahui karakteristik penderita dengue berat yang dirawat di ruang Pediatric Intensive Care Unit (PICU) RS Dr. Hasan Sadikin sejak Januari 2009 sampai Desember 2010. Penelitian dilakukan secara retrospektif deskriptif berdasarkan data dari rekam medis penderita. Sebanyak 21 penderita dengue berat dirawat selama 2 tahun, 15/21 penderita perempuan
dan 6/21 laki-laki, serta 5/21 anak meninggal dunia selama dirawat dengan sebab kematian tersering sindrom
syok dengue (SSD) dan kogagulopati intravaskular diseminata (KID). Sebagian besar penderita berusia 1−5 tahun
dengan status gizi baik. Hepatomegali ditemukan pada semua penderita dengan hematokrit rata-rata 38%. Pada penelitian ini, manifestasi klinis dengue berat berupa SSD (15/21), KID (11/21), ensefalopati (6/21), efusi pleura
(5/21), miokarditis (3/21), serta acute respiratory distress syndrome (3/21). Simpulan, dengue beratlebih banyak didapatkan pada anak perempuan, usia 1–5 tahun, serta status gizi baik. Manifestasi klinis dengue berat yang
dominan berupa syok, koagulasi intravaskular diseminata, dan ensefalopati. [MKB. 2011;43(2S):48S–52]. Kata kunci: Dengue berat, karakteristik, pediatric intensive care unit
Characteristic of Severe Dengue Hospitalized
in Pediatric Intensive Care Unit
Abstract
Dengue viral infections affect all age groups and produce a spectrum of clinical illness that ranges from asymptomatic to severe and occasionally fatal disease. Severe dengue characterized by plasma leakage, hemoconcentration, and hemostatic disorder. The aim of this study was to know the characteristic of severe dengue patients admitted to Pediatric Intensive Care Unit (PICU) Dr. Hasan Sadikin Hospital Bandung during January 2009 to December 2010. This was a retrospective descriptive study based on the data collected from the medical records.
Twenty-one severe dengue cases in two years was admitted 15/21 females and 6/21 males, and 5/21 of them died during
hospitalization because of dengue shock syndrome (DSS) and disseminated intravascular coagulation (DIC). Most of them were 1−5 years old with good nutritional status. Hepatomegaly was found in all cases with mean
hematocrit was 38%. In this research, the most manifestation of severe dengue were DSS (15/21), DIC (11/21), encephalopathy (6/21), pleural effusion (5/21), myocarditis (3/21), and acute respiratory distress syndrome (3/21).
In conclusions, severe dengue more common in girls, 1–5 years old, and well-nourished children. The most common clinical manifestation of severe dengue were shock, disseminated intravascular coagulation, and encephalopathy.
[MKB. 2011;43(2S):48S–52].
Key words: Characteristic, pediatric intensive care unit, severe dengue
Korespondensi: Dzulfikar Djalil, dr., Sp.A(K), M.Kes, Departemen Ilmu Kesehatan Anak Fakultas Kedokteran Universitas Padjadjaran-Rumah Sakit Dr. Hasan Sadikin, jalan Pasteur No. 38 Bandung 40163, Indonesia, telepon (022) 2035957,