Low ankle brachial index predicts new vascular events
and functional outcome after 1 year in patients with
non-cardioembolic stroke: our experience and review
J. Alvarez-Sab
ın
a, M. Quintana
a, E. Santamarina
a, O. Maisterra
aand A. Gil-N
u
~
nez
b aNeurovascular Unit, Department of Neurology, Universitat Autonoma de Barcelona, Hospital Vall d’Hebron, Barcelona; and bStroke Unit, Department of Neurology, Hospital Universitario Gregorio Maranon, Universidad Complutense, Madrid, Spain~
Keywords:
ankle brachial index, atherothrombotic stroke, outcome, recurrence, stroke
Received 7 June 2013 Accepted 26 July 2013
Background and purpose: The ankle brachial index (ABI) has been defined as an important factor associated with vascular events. Our objective was to analyze the prognostic value of the ABI as a predictive factor of new vascular events and func-tional status at 1 year in patients with non-cardioembolic ischaemic stroke.
Methods: A prospective, longitudinal, observational and multicenter study was per-formed, including consecutive patients≥50 years old who had suffered from a non-cardioembolic ischaemic stroke. Pathological ABI (PI) was defined when the value was≤0.9. The logistic regression model, survival analysis and the Cox proportional hazard regression model were used to identify factors independently associated with functional outcome and occurrence of new vascular events, including recurrent stroke.
Results: In all, 977 patients were evaluated. The mean age was 69.19.5 years. 40.5% patients had PI. Stroke recurrence and new vascular events global rates were 9% and 20% respectively at 1 year. PI was independently associated with new vas-cular events [hazard ratio 1.764 (1.274–2.444), P =0.001]. A cut-off point of ABI≤0.8 (14% vs. 7%,P =0.002) independently predicted stroke recurrence in an adjusted regression model [hazard ratio 1.807 (1.102–2.963),P=0.019]. PI was also associated with functional dependence [odds ratio 1.490 (1.011–2.196),P= 0.044]. Conclusions: In non-cardioembolic ischaemic stroke patients, PI was an indepen-dent predictive factor of new vascular events and functional outcome after 1 year of follow-up.
Introduction
Stroke is the largest single cause of long-term disabil-ity in adults and one of the main causes of mortaldisabil-ity [1]. Recurrence after an ischaemic stroke or transient ischaemic attack (TIA) frequently leads to additional mortality or disability [2]. Although the average annual rate of recurrent stroke has declined substan-tially over the last few decades due to the cumulative advances in secondary prevention [3], about a quarter of strokes are still recurrent [4].
The functional prognosis after a year of follow-up in stroke patients has been assessed in some studies [5–9], giving values of functional independence from 63% to 70% at 1 year. With regard to possible
fac-tors associated with functional prognosis in stroke patients at 1 year, in most studies stroke severity was found to be a constant variable [6–8,10]. However, other factors have been defined: age [6,7,10], presence of previous stroke [8,10], blood glucose levels [11] and baseline C-reactive protein [11].
In the general population, low ankle brachial index (ABI) (<0.9) is associated with an increased risk of global mortality, vascular mortality, coronary disease and stroke [12]. In ischaemic stroke patients [13] ABI is significantly lower compared with the general popu-lation, and its prognostic value has been analyzed in a few studies of ischaemic stroke, although all reports show a wide variability. Most of them have reported that ABI ≤0.9 increases the risk of suffering new vas-cular events [14–18] and is also related to mortality [17,19]. However, the association with stroke recur-rence remains less clear. Moreover, the role of ABI in predicting long-term functional status in stroke Correspondence: J. Alvarez-Sabın, Department of Neurology,
patients is not well known. No studies have assessed the actual effect of ABI on long-term functional status (1 year) in patients with stroke. The only data were published by Kim et al. [20], showing that an ABI≤0.9 independently predicted poor outcome [modified Rankin scale (mRS) > 2] at 3 months of follow-up.
The main objective of our study was to evaluate ABI as a predictive factor of functional outcome and new vascular events, including recurrent stroke, in patients who had recently suffered from a non-cardio-embolic ischaemic stroke.
Methods
A prospective, longitudinal, observational and multi-center study was performed, including basal data of patients referred to 121 different hospitals from rural or urban areas in Spain. Each investigator included a maximum of 10 consecutive ≥50-year-old patients suf-fering from a non-cardioembolic TIA or ischaemic stroke and admitted to a neurology department. Patients were included in the study at discharge. The average time between stroke and inclusion in the study was 7.2 days. All participants signed an informed consent form. The study was approved by the local ethics committee, Vall d’ Hebron Hospital Institutional Review Board.
Transient ischaemic attack and ischaemic stroke eti-ology were classified according to the TOAST criteria [21]. The risk factors considered in the study were the same as defined in previous reports [22]. Basal neuro-logical status on admission was evaluated using the NIH Stroke Scale (NIHSS) [23]. Follow-up assessment at 1 year was performed via telephone interviews with the patients or their next of kin. The mRS [24,25] was evaluated to assess the functional status of the patient. mRS ≤2 indicated no functional dependence. New vascular events were defined as a composite of coro-nary heart disease (corocoro-nary death, myocardial infarc-tion, stable or unstable angina and coronary revascularization), cerebrovascular events (ischaemic stroke, hemorrhagic stroke and TIA), peripheral artery disease (intermittent claudication and lower extremity arterial revascularization) and vascular death.
In the present study demographic data, cerebrovas-cular risk factors, previous vascerebrovas-cular disease, previous pharmacological treatment, blood pressure (BP) mea-surement, weight and height and also blood test results were collected.
To calculate the ABI, systolic BP (SBP) was mea-sured using a Doppler probe in both the humeral and posterior tibial arteries. Right ABI was calculated
from the SBP of the right leg divided by the maxi-mum SBP of the arms and in the same way left ABI (SBP left leg/maximum SBP of the arms), taking the smallest value of them as the valid ABI. A pathologi-cal ABI (PI) was defined as a value ≤0.9 [26]. A lower cut-off point of ABI (≤0.8) [27] was also explored in order to better predict the evolution of these patients.
Statistical analysis
The analyses were performed with the use of SPSS 15.0 software for Windows.
In the descriptive analysis, categorical data are shown as frequencies (%)and quantitative data as mean standard deviation or median (interquartile range), the latter in the case of numerical variables that were not close to a normal distribution.
Statistical significance for intergroup differences was assessed by Pearson’s chi-squared for categorical vari-ables and the Student’s t test or Mann Whitney U test for continuous variables. Multivariate analysis
using a logistic regression model was done to deter-mine factors independently associated with PI.
Survival curves and tables were used to analyze the rate of vascular events, stroke recurrence and mortal-ity during follow-up. Survival analysis was performed with the Kaplan Meier method, using the log-rank test to determine variables associated with a higher risk of new vascular events and mortality.
Finally, multivariate analysis using forward stepwise Cox regression [presented as hazard ratio (HR) with 95% confidence interval (CI)] was used to identify fac-tors independently associated with risk of new vascu-lar events, stroke recurrence or mortality; a forward stepwise logistic regression analysis was also per-formed to find independently associated factors of functional dependence or death (mRS >2) at 1 year [presented as odds ratio (OR) with 95% CI]. All fac-tors associated in univariate analysis were included in the multivariate models. HR and OR for continuous variables are per 1 unit increase.
P values<0.05 were considered statistically
signifi-cant for all tests.
Results
Initial visit
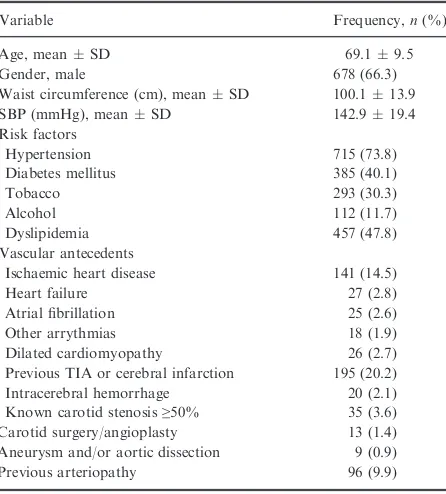
In all, 977 patients were included; 66.7% were male. The median age was 69.19.5 years. Main baseline characteristics including risk factors and previous vas-cular events are shown in Table 1. 18.5% of patients had suffered a TIA. With regard to etiology, athero-thrombotic etiology was the most prevalent (57.2%)
©2013 The Author(s)
European Journal of Neurology©2013 EFNS
followed by lacunar stroke (29.7%), undetermined (12.5%) and 0.5% of unusual cause.
Mean ABI was 0.92 0.21; 40.5% of patients had PI. After performing a logistic regression analysis, fac-tors independently associated with PI were established stroke, atherothrombotic etiology, previous arteriopa-thy (defined as previous physician diagnosis of periph-eral arterial disease), SBP, waist perimeter, age, tobacco, coronary revascularization, previous stroke and intermittent claudication.
Follow-up
A total of 836 patients were evaluated 1 year after the index stroke. Of these, 166 (19.8%) patients suffered from some type of vascular event during follow-up: 72 of them had stroke, 53 had an ischaemic heart disease event and 41 showed episodes of intermittent claudica-tion. Recurrence rates of vascular events in these patients were 7.7% (5.9–9.5%), 12.7% (10.5–14.9%) and 19.7% (17–22.4%) at 3, 6 and 12 months respec-tively. In Fig. 1 it can be seen that individuals with PI had more vascular events during follow-up. Thus, in patients with PI, the rate of vascular events within the first year was 27% compared with 14% in the normal ABI group (log-rank, P <0.001). Table 2 shows the variables significantly associated with occurrence of new vascular events. The results of the Cox regression showed, as independent predictors of new vascular
events, PI [1.764 (1.274–2.444), P =0.001], athero-thrombotic stroke [1.817 (1.274–2.591), P= 0.001], previous ischaemic heart disease [1.953 (1.350–2.826), P <0.001] and higher SBP [1.011 (1.003
–1.019),
P =0.006].
With regard to stroke recurrence, it was present in 72 patients during follow-up. Recurrence rates were 2.6% (1.5–3.7%), 5% (3.5–6.5%) and 8.9% (6.9– Table 1 Demographic and risk factor profile
Variable Frequency,n(%)
Age, meanSD 69.19.5
Gender, male 678 (66.3)
Waist circumference (cm), meanSD 100.113.9
SBP (mmHg), meanSD 142.919.4
Risk factors
Hypertension 715 (73.8)
Diabetes mellitus 385 (40.1)
Tobacco 293 (30.3)
Alcohol 112 (11.7)
Dyslipidemia 457 (47.8)
Vascular antecedents
Ischaemic heart disease 141 (14.5)
Heart failure 27 (2.8)
Atrial fibrillation 25 (2.6)
Other arrythmias 18 (1.9)
Dilated cardiomyopathy 26 (2.7)
Previous TIA or cerebral infarction 195 (20.2) Intracerebral hemorrhage 20 (2.1) Known carotid stenosis≥50% 35 (3.6) Carotid surgery/angioplasty 13 (1.4) Aneurysm and/or aortic dissection 9 (0.9)
Previous arteriopathy 96 (9.9)
SBP, systolic blood pressure; TIA, transient ischaemic attack.
1.0
0.8
0.6
0.4
0.2
0.0
n = 836 n = 769 n = 721 n = 667 n = 570
ABI ≤0.9
Figure 1 Kaplan Meier curves comparing PI with new vascular events.
Table 2 Variables significantly associated with new vascular events during follow-up
Variables
New vascular events
P
No Yes
Age 68.99.4 70.69.4 0.030
Hypertension 72.4% 81.7% 0.023
Diabetes mellitus 39.6% 51.5% 0.007
Previous ischaemic heart disease
11.7% 24.8% <0.001
Previous antiplatelet treatment
34.2% 51.8% <0.001
Previous lipid-lowering therapy
27.6% 36.1% 0.038
Previous antidiabetic treatment
28.4% 40.4% 0.003
Peripheral vasodilators treatment
4.5% 10.8% 0.009
Systolic blood pressure 142.119.8 146.718.4 0.009 HDL (mg/dl) 46.013.4 43.112.9 0.017 Triglycerides 148.782.2 169.499.3 0.005
ABI 0.940.20 0.860.23 <0.001
Etiologic classification (TOAST)
Atherothrombotic 53.1% 72.2% <0.001
Lacunar 32.2% 22.2%
Undetermined 14.7% 5.6%
10.9%) at 3, 6 and 12 months respectively. The rate of recurrence at 1 year follow-up in patients with PI was 12% compared with 7% for the rest (log-rank, P =0.014), without achieving statistically significant
association after a Cox regression analysis [HR 1.603 (0.995–2.583), P= 0.052]. ABI≤0.8 more clearly increased the risk of a new stroke (14% vs. 7%, P =0.002) and emerged as an independent predictor
of stroke recurrence [1.807 (1.102–2.963), P= 0.019] in the multivariate analysis, as did the presence of pre-vious hypertension [2.193 (1.038–4.635), P= 0.040], age [1.039 (1.010–1.068), P= 0.007] and SBP [1.012 (1.000–1.024),P =0.045].
Mortality was assessed, finding that 45 (5.4%) patients died during follow-up, 22 from vascular causes. Mortality rates in these patients were 1.7% (0.8–2.6%), 3.2% (2–4.4%) and 5.3% (3.8–6.8%) at 3, 6 and 12 months respectively. PI patients showed higher rates of mortality (6.8% vs. 4.3%, P =0.117), although with no statistically significant differences. Mortality prediction did not improve with ABI ≤0.8.
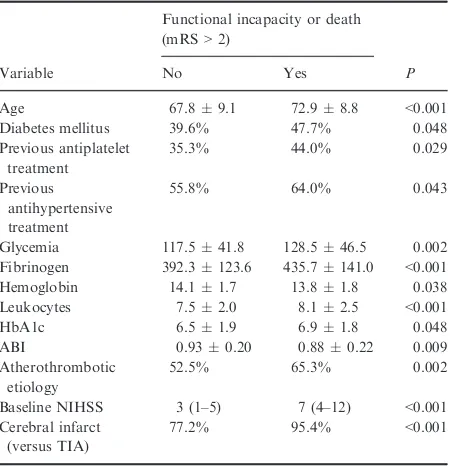
Finally, 26.5% of patients were functionally depen-dent or died (Rankin > 2) at 1 year. PI patients had poorer prognosis (32.6% vs. 22%,P =0.001). Table 3 shows the variables significantly associated with func-tional dependence or death. The result of logistic regression shows that PI independently predicted func-tional dependence or death at 1 year [1.490 (1.011–
2.196), P =0.044], as did age [1.076 (1.051–1.102), P <0.001], baseline NIHSS [1.194 (1.146–1.245),
P <0.001], established stroke [3.583 (1.563–8.213), P =0.003] and baseline levels of glucose [1.006
(1.002–1.011),P =0.004].
Discussion
The main findings of the present study were that low ABI in non-cardioembolic stroke patients predicted functional outcome at 1 year and increased the risk of vascular events, including recurrent strokes.
In our series, 40.5% patients had PI. This percent-age is five times the prevalence observed in the gen-eral population [28] and is considerably higher than in previous studies in stroke patients (Table 4). How-ever, these differences disappeared if studies with sim-ilar populations to ours were considered, with a prevalence ranging between 33.5% and 52.8% [14,29,30]. With regard to follow-up, the mortality rate was 5.4% and 20% presented a vascular event. Patients with PI had more vascular events (27% vs. 14%, P <0.001), similar to the majority of published studies (Table 4). The PATHOS study [29] did not find significant differences between PI and new vascu-lar events, although in this case only recurrent strokes or myocardial infarctions were considered as vascular events. Nonetheless, the PATHOS study was the only study in which no difference was found, in contrast to other follow-up studies where there were clear associations between PI and new vascular events after performing adjusted multiple regression analysis.
Stroke recurrence rate was 9% at 1 year. Patients with PI had a higher recurrence rate (12% vs. 7%, P =0.014), although there was no association in a
multivariate analysis. Agnelli et al.[29], Weimar et al. [14] and Busch et al. [17] did not find significant dif-ferences using the cut-off point of 0.9. Only Purroy et al.[15] and Senet al.[18] found significant
associa-tions with ABI ≤0.9 after performing adjusted mod-els. However, in our study a lower value of ABI (≤0.8) predicted recurrence more clearly (14% vs. 7%, P =0.002), and this value remained an independent
predictor after a multivariate analysis. This finding is similar to that observed in the Manzano study [27] where this ABI cut-off was defined as an independent predictor for stroke recurrence.
Few studies have assessed the functional status of patients 1 year after suffering an ischaemic stroke [5,8,9], and the results range from 31% to 35% of patients with functional dependence. The percentages are slightly higher than in our study (26.5%), proba-bly because our study included patients with TIA. Table 3 Variables associated with incapacity or death (mRS>2) at
12 months
Variable
Functional incapacity or death (mRS>2)
P
No Yes
Age 67.89.1 72.98.8 <0.001
Diabetes mellitus 39.6% 47.7% 0.048
Previous antiplatelet
Glycemia 117.541.8 128.546.5 0.002
Fibrinogen 392.3123.6 435.7141.0 <0.001
Hemoglobin 14.11.7 13.81.8 0.038
Leukocytes 7.52.0 8.12.5 <0.001
mRS, modified Rankin scale; ABI, ankle brachial index; NIHSS, NIH Stroke Scale.
©2013 The Author(s)
European Journal of Neurology©2013 EFNS
Table 4 Ankle brachial index studies in ischaemic strokes
Study Patient selection
Number
of patients Obtaining ABIa
Prevalence ABI≤0.9
Follow-up time New vascular events Stroke recurrence
Functional prognosis and/
836 During admission 40.5% 1 year ABI≤0.9: 27% vs. 14%, P<0.001*
ABI≤0.9: 12% vs. 7%P=0.014 ABI≤0.8: 14% vs. 7%,P=0.002*
Mortality: 6.8% vs. 4.3%,
P=n.s.
mRS>2: 32.6% vs. 22%, P=0.001*
Agnelliet al.[29] (Italy 2006)
Non-cardioembolic ischaemic stroke
755 During admission 33.5% 1 year ABI≤0.9: 8.7% vs. 6%,
P=n.s.
ABI≤0.9: 3.2% vs. 2.4%,P=n.s.
Mortality: 5.1% vs. 3.2%,
P=n.s.
Weimaret al.[14] (Germany 2008)
Ischaemic stroke 852 During admission 52.8% 1.5 years ABI≤0.9: 10.4% vs. 5.5%, P=0.001*
Ischaemic stroke 204 Within 7 days of stroke onset
31% 2.3 years ABI≤0.9: 12.8% vs. 6.3%, P=0.03*
ABI≤0.9: 6.8% vs. 4.4%,P=n.s.
Mortality: 7% vs. 3%,
P=0.05
102 During first month 26% 2.1 years ABI≤0.9: 50% vs. 16%, P<0.001*
ABI≤0.9: 31% vs. 10%,P<0.001*
Mortality: 15.4% vs. 1.3%,
P<0.05
Purroyet al.[15] (Spain 2010)
Ischaemic stroke 116 During admission 24.1% 1.5 years ABI≤0.9: 50% vs. 17%, P<0.001*
ABI≤0.9: 32% vs. 14%,P<0.001*
–
Manzanoet al.[27] (Singapore 2012)
Ischaemic stroke 1311 Within 7 days of stroke onset
26% 1 year ABI≤0.8 vs. ABI>0.9: 19% vs. 11%,P=0.02*
ABI≤0.8 vs. ABI>0.9: 15% vs. 10%,P=0.06*
Mortality: 6% vs. 4%,
P=n.s.
Tsivgouliset al.[16] (Greece 2012)
1147 During admission 7.4% 1 year – – Mortality: 16.3% vs. 4.3%, P<0.001*
n.s., not statistically significant (P<0.05); PAD, peripheral arterial disease; mRS, modified Rankin scale. aMeasured in supine position after a 5-min rest.
*Statistically significant in a multivariate model.
Stroke severity was the most powerful predictor of functional outcome, just as in most studies evaluating disability 1 year after stroke [7,8,10]. Age was another factor that independently predicted functional status, as in Appleros et al. [7], Vemmos et al. [6] and Wei-mar et al[10]. As in Leonards study [11], glucose lev-els also predicted functional status at 1 year, in line
with the Kong et al. study [8] where diabetes was an
independent predictor after performing a multivariate model.
Although there are no previous studies evaluating the association of ABI with long-term functional out-come (1 year of follow-up), our data regarding
prog-nosis are in concordance with Kim et al. [20]
(3 months of follow-up) where patients with PI had a
worse outcome, ABI ≤0.9 being an independent
pre-dictor of functional dependence after a multivariate analysis. In contrast, mortality was not significantly associated in our case, unlike previous studies, although the death percentage was higher in the PI group.
There were some limitations in our study. First, patients were selected consecutively in the stroke unit or neurology ward and included at discharge, so a selection bias is likely. Despite this limitation, it was not thought that the results could vary greatly as only a few patients with TIA or lacunar stroke could not be enrolled in the study because they were not admit-ted to hospital. Secondly, 141 patients had no follow-up information after discharge from hospital, so this may induce another selection bias. These patients did not return to the hospital and could not be contacted by phone. However, there were no differences in base-line characteristics (including ABI) between patients lost to follow-up and those completing the study (data not shown). Thirdly, the results could not be general-ized to other patient populations. Finally, it must be taken into consideration that, although ABI is a good predictor of outcome, other prediction methods such as the Essen Stroke Prediction Score are much less time consuming [14].
In conclusion, our results show a high prevalence (40.5%) of PI in patients in Spain with ischaemic stroke of non-cardioembolic origin. PI independently predicts the presence of new vascular events and func-tional dependence in these patients at 1-year follow-up. This finding, if confirmed in further studies, sug-gests that ABI might help in the identification of patients at the highest risk in whom a more intensive therapeutic intervention may be indicated.
Acknowledgements
This study was funded by Sanofi-Aventis.
Disclosure of conflicts of interest
The authors declare no financial or other conflicts of interest.
References
1. Lackland DT, Elkind MS, D’Agostino R, et al. Inclu-sion of stroke in cardiovascular risk prediction instru-ments: a statement for healthcare professionals from the American Heart Association/American Stroke Associa-tion.Stroke2012;43:1998
–2027.
2. Jørgensen HS, Nakayama H, Reith J, Raaschou HO, Olsen TS. Stroke recurrence: predictors, severity, and prognosis. The Copenhagen Stroke Study. Neurology 1997;48:891
–895.
3. Hong KS, Yegiaian S, Lee M, Lee J, Saver JL. Declin-ing stroke and vascular event recurrence rates in second-ary prevention trials over the past 50 years and consequences for current trial design.Circulation 2011; 123:2111–2119.
4. Lloyd-Jones D, Adams RJ, Brown TM,et al.; on behalf of the American Heart Association Statistics Committee and Stroke Statistics Sucbcommittee. Heart Disease and Stroke Statistics – 2010 Update. A report from the
American Heart Association.Circulation2010;121:e46–
e215.
5. Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project–1981–1986. 2. Incidence, case fatality rates and
overall outcome at one year of cerebral infarction, pri-mary intracerebral and subarachnoid hemorrhage. J Neurol Neurosurg Psychiatry1990;53:16
–22.
6. Vemmos KN, Bots ML, Tsibouris PK,et al.Prognosis of stroke in the south of Greece: 1 year mortality, functional outcome and its determinants: the Arcadia Stroke Regis-try.J Neurol Neurosurg Psychiatry2000;69:595
–600.
7. Appleros P, Nydevik I, Viitanen M. Poor outcome after first-ever stroke. Predictors for death, dependency, and recurrent stroke within the first year. Stroke 2003; 34: 122–126.
8. Kong FY, Tao WD, Hao ZL, Liu M. Predictors of one-year disability and death in Chinese hospitalized women after ischemic stroke.Cerebrovasc Dis2010;29:255–262.
9. Kang HJ, Stewart R, Park MS,et al.White matter hy-perintensities and functional outcomes at 2 weeks and 1 year after stroke.Cerebrovasc Dis2013;35:138
–145.
10. Weimar C, Kuith T, Kraywinkel K, et al.,for the Ger-man Stroke Data Bank Collaborators. Assessment of functioning and disability after ischemic stroke. Stroke 2002;33:2053
–2059.
11. Leonards CO, Ipsen N, Malzahn U, Fiebach JB, Endres M, Ebinger M. White matter lesion severity in mild acute ischemic stroke patients and functional outcome after 1 year.Stroke2012;43:3046
–3051.
12. Heald CL, Fowkes FG, Murria GD, Price JF. Risk of mortality and cardiovascular disease associated with the ankle brachial index: systematic review.Atherosclerosis 2006;189:61–69.
13. Nakano T, Ohkuma H, Suzuki S. Measurement of ankle brachial index for assessment of atherosclerosis in patients with stroke.Cerebrovasc Dis2004;17:212–217.
©2013 The Author(s)
European Journal of Neurology©2013 EFNS
14. Weimar C, Goertler M, Rother J,€ et al., on behalf of the SCALA Study Group. Predictive value of the Essen Stroke Risk Score and Ankle Brachial Index in acute is-chaemic stroke patients from 85 German stroke units. J Neurol Neurosurg Psychiatry2008;79:1339–1343. 15. Purroy F, Coll B, Oro M, et al. Predictive value of
ankle brachial index in patients with acute ischemic stroke.Eur J Neurol2010;17:602
–606.
16. Tsivgoulis G, Bogiatzi C, Heliopoulos I, et al. Low ankle brachial index predicts early risk of recurrent stroke in patients with acute cerebral ischemia. Athero-sclerosis2012;220:407
–412.
17. Busch MA, Lutz K, R€ohl JE, Neuner B, Masuhr F. Low ankle brachial index predicts cardiovascular risk after acute ischemic stroke or transient ischemic attack. Stroke2009;40:3700
–3705.
18. Sen S, Lynch DR Jr, Kaltsas E, et al. Association of asymptomatic peripheral arterial disease with vascular events in patients with stroke or transient ischemic attack.Stroke2009;40:3472–3477.
19. Lee DH, Kim J, Lee HS, et al. Low ankle brachial index is a predictive factor for initial severity of acute is-chaemic stroke.Eur J Neurol2012;19:892–898. 20. Kim J, Lee DH, Cha MJ, et al. Low ankle brachial
index is an independent predictor of poor functional outcome in acute cerebral infarction. Atherosclerosis 2012;224:113
–117.
21. Adams HP Jr, Bendixen BH, Kappelle LJ,et al. Classifi-cation of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial. TOAST: trial of Org 10172 in acute stroke treatment.Stroke1993;24:35
–41. 22. Alvarez-Sabın J, Gil-Nu~nez A, Quintana M, Barbera G.
Prevalencia de enfermedad arterial periferica
asin-tomatica en pacientes con ictus isquemico no cardio-embolico.Neurologia2009;24:366–372.
23. Wityk RJ, Pessin MS, Kaplan RF, Caplan LR. Serial assessment of acute stroke using the NIH Stroke Scale. Stroke1994;25:362–365.
24. Rankin J. Cerebral vascular accidents in patients over the age of 60.Scott Med J1957;2:200–215.
25. Van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assess-ment of handicap in stroke patients. Stroke 1988; 19: 604–607.
26. Hiatt WR. Medical treatment of peripheral arterial dis-ease and claudication. N Engl J Med 2001;344: 1608
– 1621.
27. Manzano JJF, De Silva DA, Pascual JLR, Chang HM, Wong MC, Chen CPLH. Associations of ankle brachial index (ABI) with cerebral arterial disease and vascular events following ischemic stroke. Atherosclerosis 2012; 223:219–222.
28. Doobay AV, Anand SS. Sensitivity and specificity of the ankle brachial index to predict future cardiovascular outcomes: a systematic review.Arterioscler Thromb Vasc Biol2005;25:1463–1469.
29. Agnelli G, Cimminiello C, Meneghetti G, Urbinatis S, for the Ployvascular Atherothrombosis Observational Survey (PATHOS) Investigators. Low ankle brachial index predicts an adverse 1-year outcome after coronary and cerebrovascular events.J Thromb Haemost2006;4: 2599–2606.
30. Topakian R, Nanz S, Rohrbacher B, Koppensteiner R, Aichner FT; OECROSS Study Group. High prevalence of peripheral arterial disease in patients with acute ische-mic stroke.Cerebrovasc Dis2010;29:248