VoI 7, No 3, JuIy - September 1998 Rotational atherectomy and angiop las ty
r33
Treatment of
complex and 66undilatable"
coronary
stenosis
using rotational
atherectomy
\ilith
adjunctive or
complementary balloon angioplasty
Teguh
SantosoAbstrak
Diselidiki 32 penderita yang memPunyai kelninan pembuluh koroner kompleks dengan ciri-ciri morfologik dimana angioplasti koroner kanvensional ( PTCA) akan tidak memberi hasil baik, seperti stenosis ostial, lesi beikapur, Iesi panjang
dan difus, Iesi
isinotik
^tau lesi yang tidak dapat dilewati atau diperlebar dengan balon. Ke-32 penderita ini menjalani7i tindal*n,
dim.ana rotablnsi dan adjunctive atau complementary PTCA dilakukan padaj3
pembuluh darah untuk memperbàiki50
lesi koroner. Lokasi ;esi umumnya (87'5Vo) pada pembuluh left anterior descending artery.Terdapat 19 lesi tipe 82 (38,0Voi dan3l
lesi tipe C (62,080). pTCA konvensional
juga dilakukan pada 22 lesi. Dari ke-32 penderita tersebut, t9 prta dan 13 wanita. (Jmur berkiiar 42 sampai 79 tahun. Kebanyakan mempunyai angina kelas CCS
III
atau IV. Fraksi ejeksi adalah 507o pada 17 pendertta (53,IVo), 30-50Vo pada I0 penderita 6jJE"),
dan
30Vo pada 5penderin
(15,68ù. Pada 3 penderita diperlukan pemasangan intra-aortic balloon pumpinguntuk stabilisasi
hemodinamik. Tujuh penderita (21,9Eo) mempunyai penyakit satu pembuluh, tS (SS,IE") mempunyai penyakit dua pembuluh dan 6 ( l8,7Vo) mempunyai penyakit tiga pembuluh. Angka keberhasilan angiografik dan proseduril I0ô Vo.'Hasit yang baik imumnya dicapai setelah dilakakan PTCA pasca rotablnsi. Stenosis koroner yang kompleks dan tidak dapat di-dilntasi masih dapat diobati dengan rotablasi yang diikuti dengan PTCA.Abstract
We studied 32 patients who had complex lesions
or
morphologic characteristics associated withpoor
outcome utilizing conventional PTCA, such as ostial stenosis, calcified lesions, long or diffuse lesions, restenotic lesionsor
Lesions which can not be crossed or dilnted with a balloon. These 32 patients underwent 72 proceduresin which rotational atherectomy and adjuncrive
or complementary PTCAwereperformedin 33 vessels to treat 50lesions. Theywere mainly (87.5Vo) in the left anteriordescendiig coronary artery' According to modffied ACC/AHA lesion classification, there were 19 type B2 lesions (38.0Vo) and3l type
C
lesiois (62.0Vo). Plain balloon angioplasty was also performed in additional 22 lesions .Of the 32 patients, 19 were mnle and 13 femate. Their ages ranged from 42 to 79 years. The majority presented with Canadian Cardiovasculai Society angina classIII
or IV. The left ventriculareiectionfractionwas
507oin
17 pati.ents (53.1 Eo), 30 - 50% inl0
patients (31.3Vo)and
3dVo in 5 patients (I5.6qo).In 3 patients
rotational atherectomy was performedwith the aid of intra-aortic balloon pumpingfor hemodynamic stàbi1zation. single vessel disease was Present
in
7 patients (21.9Vo), double vessel diseasein
19 patients (59.4Vo) andtriple
vessel diseasein
6 patients (lg.77o). Angiographic and procedural success rates were l00Vo. However, largely, success criteriawàs achieved after adjunctive orcomplemen-tary
PTCA had been performed. Complex and "undilatable" coronary stenosis may be treated withrotational
atherectomy and adjunctive or complementary PTCA.Keywords
: Coronary artery
disease, angioplasty, atherectomy.INTRODUCTION
optimal results include:
(a) ostial
lesions,
(b)
sig-nificant calcification,
(c)
long, narrow or
diffuse
disease, (d) lesions crossable
with wire, but
noballoon could
follow,
and
(e)
lesions crossable
with
wire and
balloon
that
do not yield to high
pressures. Such lesionswould
ordinarily
require coronary
bypasssurgery
or they may
even
be so diffuse
as
to be
in-operable.134 Santoso
Rotational
atherectomy
is
atechnique that selectively
ablates and
pulverizes inelastic, fixed,
atheromatoustissue
into microparticles, which
are smaller than redblood cells
and
fieely
pass through the capillaries.s'6Compared
to PTCA, the
final
result
is
an expanded,circular arterial lumen
with
a
smooth,
polished,
lessthrombog_enic surface,
which is free
of significant
dis-section.5'6 The technique appears to bewell
suitedfor
certain
type
B/
C
lesions, such
asostial, calcified
or
long
lesions and "undilatable lesions." Rotational
atherectomy is not recommended
for
usein
thrombus
containing lesions, degenerated saphenous vein grafts
and very
long lesions (i.e. more than 25 mmin
length).oThe use
of
rotational
atherectomy as
a
stand
alonedevice
has been evaluatedin
severalsingle and
multi-center studies.T-9Lower
success and highercomplica-tion
rates are
noted, however,
with
increasing lesion
complexity
such
astype
C
lesions and
particularly in
diffuse
diseas".6'10tfrè
useof rotational
atherectomyfollowed bv
PTCA
has been nerformedwith
remark-ableclinical
,u"""rr.6'7'9'10
'It,"
purposeof
this
study was to evaluate theefficacy
and safetyofthis
strategyin
patients
with
complex
and"undilatable"
coronary
lesions.MATERIALS
AND METHODS
The
Rotational Atherectomy
Device
(Rotablator)
The
Rotablator
System (Heart
Technology, Inc.
Bel-levue,
WA)
consistsof
a reusable consolewhich
con-trols
and monitors therotational
speedof
a disposableadvancer.
The
advancer consists
of
an
elliptical-shaped brass
burr
coatedwith
5to
l0
u diamond chipsbonded
to
aflexible drive
shaft.
It
is
powered
with
acomprised
nitrogen-driven turbine
that
spinsthe burr
over the guidewire
at 160,000
to
190,000revolutions-per-minute (rpm). Burr
diameters range
from
1.25 to2.5 mm.
A
300cm exchange
length guide
wire
allows
passage
of
sequentially increasing burr
diametersover
the sameguide
wire.
Patients
The
study group consisted
of
32 patients undergoing
33
rotational atherectomy procedures
followed
by
bal-loon angioplasty.
All
patients had significant coronaryartery
diseasewith all
lesions having
>
70Vo stenosis.All
patients had complex lesions or morphologic char-acteristics associatedwith
poor
outcomeutilizing
con-ventional
PTCA,
such as
ostial
stenosis,
calcified
lesions,
long
or
diffuse
lesions, restenotic lesions or
lesions which can
not
be
crossed
or
dilated
with
aMed J Indones
balloon.
Patients
with
unprotected
left
main
disease,visible
thrombus
or old
degeneratedvein
grafts were
excluded.
In
3patients
with
a leftventricular
ejection
fraction
of
<30Vo,
intra-aortic balloon
counter
pulsa-tion
was applied
for
cardiac support
while
rotational
atherectomy procedure was carried out.
Procedure
Pre-procedure medications
included
nitrates, calcium
antagonist (unless contra-indicated),
aspirin
andticlopidine.
Procedural medications
included
heparin,intracoronary nitrates and verapamil.
Ten
thousandinternational units
of
heparin were given
at thebegin-ning ofthe
procedure and thenhourly
as needed to keepthe
ACT >
350 msec.
Liberal
dosesof
intracoronary
nitrates were
utilized
throughout
the procedure
to
prevent
coronary
spasm.
During
right
coronary
or
dominant
left
coronary
rotational
atherectomy,
atem-porary
transvenous pacemaker
was
inserted
prior
to
initiating
the procedure.A
flexible 0.009 inch guide wire
with
a 0.017
inch
spring
tip
was advanced
though
the
guiding
catheteracross the
lesion
andpositioned
well
distal in
thetarget
vessel.The
rotating burr is slowly
advancedover
theguide wire
and
through the lesion
while spinning
at16,000
to
190,000
rpm.
Several
passeswere
usually
required
until burr
advancement was resistance
free,
each pass
lasting
5
-
45
seconds depending
on
the lesion characteristics. Wepreferred
to use smallerburr
and upsized as necessary
until
adequatedebulking
was achieved.After
rotational atherectomy, réireat
angiog-raphy was
performed
andadjunctive
PTCA
was
usedto achieve
aresidual
stenosisof
less than 50Vo.An
electrocardiogram
was
obtained
before
and after
the procedure and repeated every day or when needed.
Serum cardiac
enzymes
(creatine kinase
--
CK
andCK-MB)
were measured 4 and 24 hours afteratherec-tomy
or
until
abnormal
valuesreturned to baseline.
Definitions
Angiographic
success was defined asachievement
of
a
final
diameter stenosis
of
less than
50Vo
and
aVol 7, No 3, JuIy - September 1998
twjce
the
normal
values
with
no new Q-waves
on theelectrocardiogram. Non-Q
wavemyocardial infarcti
onwas
not
categorized
asmajor complication,
becauseclinically
it
did
not
appear
to
cause
significant
per-manent sequel.
RESULTS
Baseline
characteristics
Of
the 32patients,
19 weremale
and 13female.
Their
agesranged
from 42
to
79
years
(mean
age64
+
9years). The majority
presented
with
Canadian
Car-diovascular Society angina
classIII
or
IV.
More
thanhalf
had
a history of
hyperlipidemia.
The left
ventricular ejection
fraction
was>
50Voin l7 patients
(53.1 Vo),30
-
50Voin
10patients
(3l.3Vo)
and<
30Voin
5 patients(I5.6Eo).In
3of
these 5 patientsrotational
atherectomy
wasperformed
with
the aid ofintra-aortic
balloon
pumping
for
hemodynamic
stabilization
(Table
1).Single vessel disease was present
in
7 patients(2l.9Vo),
double
vessel diseasein
19patients
(59.4Vo) andtriple
vessel diseasein
6patients
(l8.7qo) Qable
2). These32 patients underwent 72 procedures
in which
rotational
atherectomy
andadjunctive or
complemen-tary
PTCA
were performed
in
33
vesselsto
treat
50 lesions.They were
mainly
(87 .5Vo)in
theleft
anterior
descending
coronary artery. According
to
modified
ACC/AHA
lesion classification,
therewere
19typeB2
lesions
(38.0Vo) and31 type C lesions
(62.0Vo).Plain
balloon
angioplasty was
alsoperformed
in
additional
22lesions
(Tables
2
and3).
The
lesion length
wasmore than20 mm
in
26 patients(31 lesions,
or
8l.2Vo);
themajority
being
on thethird
or moreof
theentire length
of left
anterior
descendingcoronary artery
course. Threepatients
hadcritical
os-tial
left
anterior
descending
coronary artery
lesion,
where adjunctive
or complementary PTCA
hadto
beperformed
with
autoperfusion balloon
catheters
in
which part
of
the balloon
was
in
the
left
main
stem,completely obstructing
flow
to
the
left
circumflex
coronary artery.
Calcium
wasangiographically
detec-table
in
47 lesions
(94.0Eo)(Table
3).Outcome
Angiographic
success
was achieved
in all
lesions
(700Vo)
in
which
rotational
atherectomy
was
used.However, largely,
successcriteria
were met
after
ad-junctive
or
complementary PTCA
had been
per-formed. Plain
balloon
angioplasty, performed
todilate
Rotational atherectomy and
angioplasty
135non-atherectomized
lesions were successfulin all.
pro-cedural
success
was
also achieved
in all
patients(Table
4).Six
patients,
5of
whom
hadlong
andcalcified
lesion
of
more than 20
mm,
developed
spasm.In
2
patientsthis led
to
complete
vessel
closure. However,
in
all
casesspasm
could be overcome after
intracoronary
nitrate administration andlor
adjunctive
PTCA.
None
of these
6
patients sustained an acute
myocardial
in-farction.
Three patients had
small
intimal disruption
(type
B).
Since such dissection
was
always
benign, they
were managedin
mannersimilar
topatients
without
dissec-tion. In
onepatient
with
long,
calcified
lesion;
adjunc-tive PTCA with
a pressureof
5
atmospheres created aspiral luminal
filling
defect (typeD)
necessirating stenrimplantation. This laterpatient
was dischargedwithout
complication. Two
patients had dissection that led
toimpaired
flow
(type
F).
They were
successfully
managedwith
repeatballoon
dilatation.
One patient
with
along (
20
mm), calcified
lesion
in
theleft
anterior
descendingcoronary artery
developedocclusion
of
big
septal
perforator and
diagonal
branches aswell
as ano-reflow
phenomenon.
A
non-Q-wave anterior
wall
infarction and
mild left
heartfailure
ensued.
The patient
responded
promptly
andnicely
to
medical
management.
She
remained
asymptomatic
at afollow-up period
of
7months.
An
echocardiogram
performed
at
6
months' follow-up
revealed preservedleft ventricular function
andmini-mally
hypokinetic regional
wall
motion
in
the
areasupplied
by
the reference artery. Three other
patientsshowed
arise
of
cardiac enzymes
to 2 times
normal
levels, but
their electrocardiograms
didnot
significant-ly
change andtheir clinical
course wasuneventful.
There was no death and no
patient required
emergency bypasssurgery (Table
4).DISCUSSION
Although PTCA
using conventional
balloon
technol-ogy is still
the mainstay
of interventional cardiology,
in
patientswith
complex anatomy or
diffuse
diseaseit
is
associated
with a
lower
procedural
success
andhigher complication
rate.PTCA
in
rypeB2
andtype
CIesions
hasprimary
successrates
aslow
as 76Vo and6lVo
andcomplication
ratesof
l\Vo
and2lVo,
respec-tively.'''
In
more
recentreport the
success rates were 89 .5Vo and 90Vo,respectively,
for
type
B2
andtype
Cr36 Santoso
Table
l.
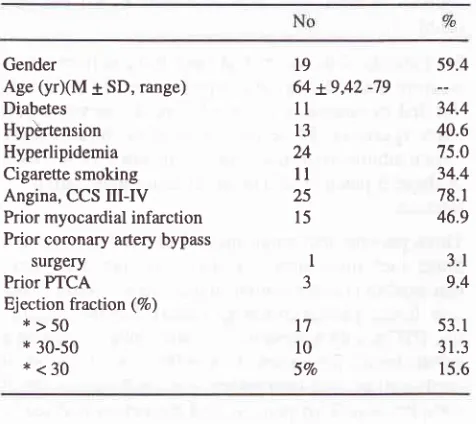
Clinical profile of 32 patients.Table 2. Extent of disease and number of procedures performed.
Med J Indones
Table 4. Success and complications
Success
- angiographic (per lesion) - procedural (per patient) Complications
- transient occlusive spasm
- dissection, type D - dissection, type F
- no reflow phenomenon
- non-Q-wave infarction
- Q-wave-infarction - Emergencybypass surgery - Death
6
I
2 1 4 18.7 3.1 6.2 3.1 12.583.2Vo,
_respectively,
for
types
A,
BI, BZ
and
C 4lesrons.'
In
the present study,
a
strategy
of
rotational
atherec-tomy followed
by
PTCA
was
employed
in
type
82
lesions
in
387oand
in
type C
lesions
in
62Voof
thepatients.
Despite
these adverse
morphologic
charac-teristics,
a
high
overall
success
rate
of
l\OVo
was
obtained. In
theERBAC
study, which
is arandomized
study comparing procedural
andangiographic
resultsof
excimer laser
angioplasty,
rotational
atherectomy
â:nd
PTCA
in
patientswith
native de-novo type B or
Clesions
suitableto all
the three techniques, stand alonerotational
atherectomy
resulted
in
better
procedural
success
(93Vo) as compared
with
PTCA
(84Vo)
andexcimer
laser angioplasty
(897r).10Recently, the
useof
rotational
atherectomy
followed
by
PTCA
at
low
inflation
pressure has beenincreasingly
demonstratedto provide
better
results
ascompared
to
stand
aloneprocedure.
Although
the
debulking effect is
lesssub-stantial, the angiographic results that
can beobtained
are
more
remarkable, particularly_
in
long
segmentalstenosis
with
diffuse atheroma.6'/'' The term
"com-plementary angioplasty" is
used
if
the balloon is
in-flated at a very
low
pressure
(0.5
to
2.5 atm)
after
rotational atherectomy
to
relieve
vasospasm
or
tosmoothen
a
satisfactorily atherectomized
segment.The term
"adjunctive angioplasry"
denotes a procedurein which
aballoon is
used atnormal or high
pressureafter rotational
atherectomy.
In
this
instance the
bal-loon is
usedto
salvage therotational atherectomy,
e.g.because
of no-reflow
phenomenon
or significant
dis-section
resulting in
abrupt
vesselclosure.' Our
result
was
similar
to the
success ratesreported
in
previous
investigations,
which
alsoincluded type
A
andtype B
lesionJ'g'I0
in
these reports, adjunctive
or
com-VoNo
Gender
Age (yrXM 1SD, range)
Diabetes Hypèrtension Hyperlipidemia Cigarette smoking Angina, CCS
III-ry
Prior myocardial infarction Prior coronary artery bypasssurgery Prior PTCA Ejection fraction (Vo)
* >50
*
30-50*<30
l9
64
+9,42
-79ll
t3 24ll
25l5
59.4 34.4 40.6 75.0 34.4 78.1 46.9 3.1 9.453.
I
31.3 15.6
50
10032
100I
J t7l0
5Vo No ExtentSingle vessel disease
Double vessel disease
Triple vessel disease
Rotational atherectomy + PTCA Number of vessels
Number of lesions Site
- left anterior descending artery - left circumflex artery - right coronary artery Additional PTCA in other sites
7 t9 6 JJ 28 2 3 22 21.9 59.4 18.7
1 03.1 50
87.5 6.2
9.4
Table 3. Morphology
of
50
lesions (33 target vesselsin
32patients) treated with rotational atherectomy and PTCA
No
Long lesion
-<lcm
-I
-2cm
->2cm
Calcified Ostial (LAD) Bifurcation Inegularities EccentricModerate-to-severe tortuosity Moderate-to-severe angulation Modified ACC/AHA Class :
[image:4.595.309.542.95.338.2] [image:4.595.48.286.106.318.2] [image:4.595.50.284.348.520.2] [image:4.595.50.284.554.738.2]Vol 7, No 3, JuIy - September 1998
plementa-ry
PTCA was
also performed
in
the
majority/'e or all
cases.sIn
our
study,
salvage
PTCA
to
treat no-reflow
phenomenon was done
in
onepatient.
The peak
bal-loon
pressure that was applied was
5
atm.
In
2
other
patients
with
abrupt
vessel
closure
because
of
vasospasm,
beside-intracoronary nitrates,
balloon
an-gioplasty
wasperformed
at a peakinflation
pressureof
4 - 5 atm.In
the restof
the patients,PTCA
was used tooptimize
the
result
of
rotational atherectomy.
Al-though
we tried to
uselow
pressures,9 patients
hadtheir balloons
inflated
to higher pressures of 6- l0
atm.In
thesepatients
therotational
atherectomymight
havenot
beenenough to debulk
thecalcified
lesions.ln
conclusion,
the presentstudy
suggests thatcomplex
and "undilatable" coronary
stenosis
may be
treatedwith
rotational
atherectomy and adjunctive
or
com-plementary
PTCA.
Further investigations
arerequired
toconfirm
our
findings.
REFERENCES
l.
DetreK,
Holubkov R, Kelsy S, et al. One-year follow-up results of the 1985-1986 National Heart, Lung, and Blood Institute's Percutaneous Transluminal Coronary Angioplas-ty Registry. Circularion 1989;80:421 -4282. Bentivoglio LG, Holubkov R, Kelsey SF, et al. Short and
long term outcome
of
percutaneous transluminal coronaryRotationaL atherectomy and
angioplasty l3j
angioplasty
in
unstable versus stable angina pectoris:
A reportof
the
1985-1986NHLBI pTCA
Registry. CarherCardiovasc Diagn 199 I ;23 :227 -238
3. Myler RK, Shaw RE, Stertzer SH, et al. Lesion morphology
and coronary angioplasty : Current experience and analysis. J Am Coll Cardiol 1992;19:1641-1652
4. Santoso
T,
et al. Lesion morphology and pTCA. Is ABC classification obsolete ? (abstr.).Asean Federation Congressof Cardiology, Bangkok, 1994, p 260
5. Farb
A,
RobertsDK,
PichardA,
et al.
Coronary artery morphologic features after coronary rotational atherectomy : Insights into mechanisms of lumen enlargement and em-bolization. Amer HeartI
1995:129 1058-10676. Reisman
M.
Guide to rotational atherectomy. physician'sPress : Birmingham, 1997.
7. Stertzer SH, Pomerantsev EV, Shaw RE, et al. Comparative study
of
the angiographic morphologyof
coronary arterylesions treated with PTCA, directional coronary atherectomy or high speed rotational ablation. Cathet Cardiovasc Diagn
1994:33:l-9
8. Sabri MN, Cowley MJ, DiSciasco G, et al. Immediare results
of interventional devices for coronary ostial narrowing with angina pectoris. Am J Cardiol 1994;73 122-125
9. Borrione M, Hall P, Almagor Y, et al. Treatment of simple
and complex coronary stenosis using rotational ablation followed by low pressure balloon angioplasty. Cathet
Car-diovasc Diagn 1993;30
:l3l
-137.10. Vandormael M, Reifart N, Preusler W, et al. Comparison of
excimer laser, rotablator and balloon angioplasty