Attention-Deficit/Hyperactivity Disorder in Adults:
An Overview
Stephen V. Faraone, Joseph Biederman, Thomas Spencer, Tim Wilens,
Larry J. Seidman, Eric Mick, and Alysa E. Doyle
To assess the validity of adult attention-deficit/hyperactiv-ity disorder (ADHD), we reviewed clinical, family, psy-chopharmacologic, neurobiological, and outcome studies. We found multiple reports describing adults with clinical features highly reminiscent of the childhood ADHD. These adults, who are impulsive, inattentive, and restless, have the clinical “look and feel” of ADHD children. As with their childhood counterparts, many adults with ADHD suffer from antisocial, depressive, and anxiety disorders. They also show clinically significant impairments— histo-ries of school failure, occupational problems, and traffic accidents. Studies of biological features show correspon-dences between child and adult cases of ADHD. Both show familial aggregation and a characteristic profile of neuropsychologic deficits; an emerging neuroimaging lit-erature suggests that abnormalities in the same brain regions underlie both the child and adult forms of the disorder. Although these converging lines of evidence support the validity of ADHD in adults, follow-up studies of ADHD children have yielded ambiguous results. This ambiguity is in part due to differences in how researchers define the persistence of ADHD, a problem that suggests future research focus on how best to diagnose ADHD in adulthood. Biol Psychiatry 2000;48:9 –20 © 2000 Soci-ety of Biological Psychiatry
Key Words: Attention-deficit/hyperactivity disorder,
di-agnostic validity, developmental psychopathology
Introduction
S
ome researchers have asserted that because ADHD usu-ally remits in adulthood (Hill and Schoener 1996), adult ADHD should be rare and of little concern to the practicing clinician. Others have claimed many cases of ADHD persist into adulthood (Barkley 1997; Faraone, in press; Spencer et al 1994b). They stress the diagnostic continuity of ADHDthroughout the life span and assert that clinically referred adults have the same syndrome that has been so well validated in pediatric cases. To be clear, this debate addresses the diagnosis of retrospectively diagnosed childhood onset ADHD, when the childhood diagnosis has been made through retrospective accounts and the current presentation shows a continuation of the syndrome into adulthood. Pro-ponents of ADHD as a valid adult diagnosis do not suggest that ADHD arises de novo in adulthood.
Resolving the debate about adult ADHD will benefit both clinicians and researchers. If the diagnostic continuity of child and adult ADHD can be established, clinicians will have a foundation for generalizing the vast pediatric ADHD research literature to adult patients. Because effec-tive treatment plans presuppose accurate diagnoses, clini-cians need to know if adults who present with what appears to be childhood onset ADHD truly have the disorder. Diagnostic accuracy is paramount for all disor-ders, but it is even more important for ADHD, which is frequently accompanied by substance abuse and usually treated with stimulants.
Clarifying diagnostic continuity will also allow a gen-eralization of research results from adults to children. This direction of generalization is especially important for research that may be considered acceptable in adults but premature or unethical in children. Examples include functional imaging with radioactive isotopes and the testing of new drugs. In the latter case, having a valid diagnosis of adult ADHD would allow researchers to show efficacy in adults and then use that information to justify trials in children.
This article addresses the validity of adult ADHD using the validity criteria of Robins and Guze (1970). In their view, the validity of any psychiatric disorder derives not from a single study, but from a pattern of consistent data. For psychiatric disorders, standard validation criteria in-clude clinical correlates, family history, treatment re-sponse, laboratory studies, course, and outcome.
Clinical Correlates
The DSM-IV recognizes three subtypes of ADHD: a predominantly inattentive subtype, a predominantly
hyper-From the Pediatric Psychopharmacology Unit, Massachusetts General Hospital (SVF, JB, TS, TW, EM, AED), the Department of Psychiatry, Massachusetts Mental Health Center (LJS), and the Department of Psychiatry, Harvard Medical School (SVF, JB, TS, TW, LJS, EM, AED), Boston, Massachusetts. Address reprint requests to Stephen V. Faraone, Ph.D., Harvard Medical School, Pediatric Psychopharmacology Unit (ACC 725), Massachusetts General Hos-pital, 15 Parkman Street, Boston MA 02114-3139.
Received December 20, 1999; revised March 24, 2000; accepted March 28, 2000.
active-impulsive subtype, and a combined subtype (Amer-ican Psychiatric Association 1994). These categories ac-knowledge clinical heterogeneity and reflect a change in emphasis from earlier definitions that stressed motoric symptoms to the current nosology, which emphasizes deficits in the regulation of cognitive function. These changes have particular relevance to adult ADHD because hyperactive symptoms diminish at a greater rate than do inattentive symptoms (Biederman et al 2000). As in children, some adults with a predominantly inattentive subtype who were previously not diagnosed are now given full diagnostic status. Because this is a relatively new change, much of the extant literature on adult ADHD employed the older definition and reflects what would now be called combined type ADHD.
Studies of adult ADHD have clearly documented the syndrome of inattention, impulsivity, and hyperactivity that are the defining features of the disorder at any age. Downey et al (1997), for example, documented these core features of ADHD among patients attending an adult ADHD clinic. Notably, they found a high correlation between the patients’ rating of ADHD symptoms and those made by independent observers, which suggests that the patients were validly reporting the nature of their symptoms.
In a family study of children with ADHD, Biederman et al (1990) examined the nonreferred adult relatives of ADHD children. Among the relatives meeting criteria for childhood-onset ADHD, more than two thirds reported current levels of ADHD symptoms within the severe range found in clinically referred children. Other studies have documented the defining feature of ADHD in referred adults (Biederman et al 1993; Millstein et al 1997), surveys of college students (Heiligenstein et al 1998, 1999; Heiligenstein and Keeling 1995), participants in treatment protocols (Spencer et al 1995), and surveys of adults (Murphy and Barkley 1996a).
Because there is a general consensus that the defining features of ADHD occur among adults, it is worthwhile to ask if ADHD seen in adults is associated with other features of childhood ADHD which, although not diag-nostic, commonly accompany the disorder. We here focus on two such features: the characteristic pattern of psychi-atric comorbidity seen in juvenile ADHD and the clini-cally significant impairments that warrant treatment of ADHD symptoms.
Do ADHD Adults Show Psychiatric Comorbidity?
Both clinical and epidemiologic studies show that, among children, ADHD frequently co-occurs with antisocial, mood, and anxiety disorders (Biederman et al 1991).
Similar findings have been seen in studies of adult ADHD. Borland and Heckman (1976) reported high rates of antisocial personality, anxiety, depressive, and substance use disorders among adults with adult ADHD. Morrison et al (1980a, 1980b) showed that, compared with psychiatric control subjects, outpatient ADHD adults had higher rates of antisocial personality disorder.
Biederman et al (1993) studied 84 clinically referred ADHD adults, 140 ADHD children, 43 nonreferred ADHD adult relatives of those ADHD children, and 248 adult relatives of normal control children. The two ADHD adult groups did not differ significantly in rates of comor-bid psychiatric disorders. Compared with control subjects, ADHD adults had significantly higher rates of antisocial personality, substance use disorders, anxiety disorders, enuresis, stuttering, and speech and language disorders. In an expanded sample, Biederman et al (1994) used gender-stratified analyses to show that ADHD adults of both genders had significantly higher lifetime rates of major depression, oppositional disorder, drug dependence, ago-raphobia, and social phobia.
Subsequent studies have consistently shown ADHD adults to have elevated rates of antisocial and substance use disorders (Downey et al 1997; Heiligenstein et al 1999; Murphy and Barkley 1996b) and anxiety and mood disorders (Downey et al 1997; Heiligenstein et al 1999; Shekim et al 1990), whereas others have not shown such comorbidity (Murphy and Barkley 1996b).
indicated by histories of school failure and impaired performance on neuropsychologic measures.
Is Adult ADHD Clinically Significant?
If adult ADHD is a clinically significant disorder, then ADHD adults should show functional impairments in multiple domains. Several studies suggest this is so. In an early study, Borland and Heckman (1976) compared ADHD adults with their non-ADHD siblings. The ADHD adults had lower socioeconomic status, more work diffi-culties, and more frequent job changes. Morrison et al (1980a, 1980b) compared ADHD adults with psychiatric control adults matched for age and gender. The ADHD adults had fewer years of education and lower rates of professional employment. Similarly, other researchers have shown that among patients with substance use disorders, ADHD predicts social maladjustment, immatu-rity, fewer social assets, lower occupational achievement, and high rates of separation and divorce (Alterman et al 1982; De Obaldia and Parsons 1984; Eyre et al 1982; Tarter 1982; Wilens et al 1998). Murphy and Barkley (1996b) compared 172 ADHD adults with 30 non-ADHD adults. The ADHD adults reported more psychologic maladjustment, more speeding violations, and more fre-quent changes in employment. Compared with the non-ADHD adults, more non-ADHD adults had had their drivers license suspended, had performed poorly at work, and had quit or been fired from their job. Moreover, the ADHD adults were more likely to have had multiple marriages. Barkley et al (1996a) evaluated the motor vehicle driving knowledge, skills, and negative driving outcomes of older teens and young adults with ADHD. The ADHD young adults showed no deficits in driving knowledge, yet compared with control subjects, they had elevated rates of speeding citations, suspended licenses, crashes, and crashes causing bodily injury. They were more likely to be rated by themselves and others as having poorer driving habits. In addition, a computer-simulated driving test showed the young adults with ADHD to have more crashes, scrapes, and erratic steering.
Given that academic underachievement is a well-known correlate of ADHD in childhood (Hinshaw 1992), ADHD adults ought to have histories reflecting school problems. Several studies have shown this to be so. Biederman et al (1993; 1994) showed that compared with control adults, ADHD adults had significantly higher rates of repeated grades, tutoring, placement in special classes, and reading disability. Similarly, Murphy and Barkley (1996b) showed that ADHD adults had histories marked by poorer educa-tional performance and more frequent school disciplinary actions against them. Notably, in addition to showing an increased likelihood of having a history of school failure,
Seidman et al (1998) showed that this could not be accounted for by age, learning disabilities, psychiatric comorbidity, or gender.
Some data suggest that the school problems faced by ADHD children and adolescents continue into the college years. Heiligenstein and Keeling (1995) studied 42 college students with ADHD. Presenting problems included learn-ing disability and academic underachievement. In another college-based study, Heiligenstein et al (1999) showed that ADHD students had lower mean grade point averages, were more likely to have been on academic probation, and had more academic problems.
In summary, the clinical features of ADHD in adults correspond to those seen in ADHD children, but one area of discrepancy between adult and juvenile samples of ADHD is the differing proportion of male to female diagnoses. Juveniles with ADHD are more likely to be boys than girls (Gaub and Carlson 1997), but this gender differential is less pronounced in adult ADHD samples (Gualtieri et al 1985; Mattes et al 1984; Wender et al 1985; Wood et al 1976). One explanation for this discrepancy is that compared with ADHD boys, ADHD girls are less likely to be severely conduct disordered and hence are less likely to be clinically referred (Gaub and Carlson 1997). It is possible that such referral biases are less salient for adults who, unlike children, can refer themselves for treatment.
A second area of discrepancy between child and adult ADHD is in the rates of substance use disorders. Despite the increased rates of substance use disorders in ADHD adults, several studies did not find significantly increased rates of substance use among ADHD adolescents (August et al 1983; Biederman et al 1997; Gittelman et al 1985). This discrepancy is in part due to the natural course of substance use, which increases in adulthood. In fact, one report shows that, although ADHD adults have increased rates of substance use in adulthood, their retrospective reports suggested they did not have increased rates in adolescence (Biederman et al 1995). Another consider-ation is that many clinically referred ADHD adults had not had treatment during childhood and adolescence. One longitudinal study shows that ADHD subjects who did not receive pharmacologic treatment were at a significantly increased risk for substance use, which suggests that medication status affects the link between ADHD and substance use (Biederman et al 1999).
Family History
and the children of ADHD adults should show an in-creased risk for ADHD. Many case-control family studies show that the former prediction is true. The parents of ADHD children are more likely to have ADHD than are the parents of non-ADHD children (Faraone and Bieder-man 1994).
In contrast to the many family studies of ADHD in childhood, there are only two small family studies of adult ADHD. Both of these produced the same intriguing result: the risk of ADHD among children of ADHD adults was much higher than the risk for ADHD among relatives of children with ADHD (Biederman et al 1995; Manshadi et al 1983). In the study by Manshadi et al (1983), 41% of the siblings of the adult ADHD probands were diagnosed with ADHD compared with no siblings of non-ADHD control subjects. Similarly, Biederman et al (1995) found a 57% prevalence of ADHD among children of ADHD adults, which was much higher than the 15 percent prevalence of ADHD among siblings of ADHD children.
The high familial loading of adult ADHD suggests that genes (or other familial risk factors) may play a smaller role in the etiology of remitting ADHD than they do for persistent ADHD. This idea has been tested in two ways. A prospective study examined 140 ADHD boys and 120 non-ADHD boys at a baseline assessment and completed a 4-year follow-up study. By midadolescence, 85% of the ADHD boys continued to have the disorder. The preva-lence of ADHD was significantly higher among the relatives of persistent ADHD probands compared with relatives of remitted ADHD probands (Biederman et al 1996). Parents of persistent ADHD probands were 20 times more likely to have ADHD than were parents of control subjects, whereas parents of nonpersistent ADHD probands showed only a fivefold increased risk. Similarly, siblings of persistent ADHD probands were 17 times more likely to have ADHD than were siblings of control subjects, whereas siblings of nonpersistent ADHD pro-bands showed only a fourfold increased risk (Faraone et al 2000). A retrospective study compared ADHD adolescents having retrospectively reported childhood onset ADHD with ADHD children. The relatives of adolescent probands had higher rates of ADHD compared with the relatives of child probands (Biederman et al 1998). Taken together, these data suggest that, when ADHD persists into adoles-cence and adulthood, it is highly familial This work suggests that future studies attempt to determine if there are clinically meaningful differences in childhood between ADHD patients who continue to be symptomatic in adulthood and those who go into remission.
A potential confound clouds the interpretation of family studies of adult ADHD. The parents of ADHD children are usually aware of the ADHD symptoms in their child. That knowledge may bias them to report ADHD symptoms in
themselves. If so, then the rates of ADHD among adult relatives of ADHD children would be spuriously high. To test this idea, Faraone et al (1997) compared the preva-lence of symptoms between 26 ADHD adults who had ADHD children and 49 ADHD adults who did not. Because the sensitivity of individual symptoms was nearly identical between groups, the authors concluded that adults with ADHD children are not biased to overreport the symptoms of ADHD in themselves.
Treatment Response
An overwhelming amount of data from close to 200 controlled clinical trials unequivocally documents the efficacy of stimulant medications in the treatment of children and adolescents with ADHD (Spencer et al 1996). Because approximately 70% of ADHD children show a therapeutic response to stimulant medication, some re-searchers have looked to studies of stimulant drugs in adult ADHD in the hope that a clear-cut response to stimulant medication would clarify the validity of adult ADHD.
Four initial studies examined a total of 137 adult ADHD patients (Gualtieri et al 1985; Mattes et al 1984; Wender et al 1985; Wood et al 1976). They found an average response rate of 50%, substantially less than the 70% response rate seen for ADHD children. Spencer et al (1995) hypothesized that the lower response rate in adults was due to insufficient dosing. They noted that the mean daily weight-corrected dose of methylphenidate in these studies of adult ADHD patients was 0.6 mg/kg per day, which was much lower than the 1.0 mg/kg per day commonly used in the treatment of ADHD children (Wilens and Biederman 1992). To test this hypothesis, Spencer et al (1995) completed a double-blind, placebo-controlled study of methylphenidate for adult ADHD that achieved an average daily dose of 1.0/mg/kg. The re-sponse rate of the stimulant-treated patients (74%) was similar to that seen among ADHD children and was significantly greater than the 4% rate seen for placebo. Methyphenidate has also been shown to be effective for adult cocaine abusers who have ADHD (Levin et al 1998). Equally consistent with the pediatric literature, trials of two other stimulants, the mixed amphetamine compound Adderall (Spencer et al 1999) and magnesium pemoline (Heiligenstein et al 1996; Wilens et al 1999), document a similar separation from placebo in adults with ADHD as has been seen in pediatric studies.
Then, in a retrospective study of 25 referred ADHD adults treated with DMI, 68% of patients showed a moderate response at mean doses of 180 mg daily (Wilens et al 1995). These data led Wilens et al (1996) to conduct a randomized, 6-week, placebo-controlled study of DMI at a target daily dose of 200 mg in 41 adult patients with DSM-III-R ADHD. They found significant reductions of ADHD symptoms in DMI-treated patients compared with placebo-treated patients. Using predefined criteria for response, 68% of DMI-treated subjects and no placebo-treated subjects were positive responders. This response rate was identical to that previously documented for pediatric ADHD using an identical design (Biederman et al 1989). Response to DMI was independent of dose, level, gender, or lifetime psychiatric comorbidity with anxiety or depressive disorders. In addition to DMI, another nor-adrenergic-specific compound, tomoxetine, also separated from placebo in a pilot-controlled study of adults with ADHD (Spencer et al 1998). Taken together, these studies in adults show that medications with documented anti-ADHD activity in pediatric anti-ADHD also work equally well in adults with ADHD, providing further evidence for the syndromatic continuity between the juvenile and adult diagnoses.
Laboratory Studies
Although there is no laboratory test of ADHD for either children or adults, laboratory measures provide useful clues about the etiology of adult ADHD and its validity as an outcome of the childhood disorder. This section exam-ines three laboratory approaches that have been applied to adult ADHD: molecular genetics, neuropsychologic as-sessment, and neuroimaging.
Molecular Genetic Studies
Molecular genetics is providing new laboratory-based methods to examine ADHD. Studies of children have already found evidence for the involvement of several genes in the etiology of ADHD: the D2 dopamine receptor gene, the dopamine-beta-hydroxylase gene, the dopamine transporter (DAT) gene, and the D4 dopamine receptor gene (Faraone and Biederman 1999). The data for the D4 receptor are especially compelling because the gene vari-ant associated with ADHD is known to mediate a blunted response to the neurotransmitter dopamine, which is one of the hypothesized causes of ADHD (Asghari et al 1995). Notably, Faraone et al (1999) showed that this variant of the D4 gene is also associated with ADHD in families ascertained through ADHD adults.
Neuropsychologic Studies
ADHD children and adolescents show impaired perfor-mance on tasks assessing vigilance, motoric inhibition, executive functions (such as organization, planning, and complex problem solving), and verbal learning and mem-ory (Barkley et al 1992; Seidman et al 1997). Several studies suggest that these problems are also seen among ADHD adults. Notably, neuropsychologic studies have consistently found ADHD adults to be impaired on mea-sures of vigilance using the continuous performance test (Barkley et al 1996b; Buchsbaum et al 1985; Downey et al 1997; Gansler et al 1998; Gualtieri et al 1985; Holdnack et al 1995; Klee et al 1986; Seidman et al 1998). These studies also have shown ADHD adults to be impaired in other functions known to affect ADHD children. These include perceptual-motor speed as assessed by the digit symbol and coding tests (Buchsbaum et al 1985; Gualtieri et al 1985; Holdnack et al 1995; Klee et al 1986; Silverstein et al 1995); working memory as assessed by digit span tests (Barkley et al 1996b; Holdnack et al 1995; Kovner et al 1998); verbal learning, especially semantic clustering (Downey et al 1997; Holdnack et al 1995; Katz et al 1998; Seidman et al 1998); and response inhibition as assessed by the Stroop Color-Word Test (Katz et al 1998; Lovejoy et al 1999; Taylor and Miller 1997).
For example, Holdnack et al (1995) reported that ADHD adults exhibited significantly slower reaction time to stimuli in the continuous performance task (a measure of vigilance). The ADHD adults also showed slower psychomotor speed and worse scores on the California Verbal Learning Test (CVLT). Downey et al (1997) examined a cohort of patients attending an adult ADHD clinic. These patients were impaired on the CVLT and on several measures of attention. Seidman et al (1998) com-pared 64 unmedicated ADHD adults with 73 non-ADHD control subjects. Compared with control subjects, adults with ADHD were significantly impaired on measures of vigilance, semantic encoding for CVLT verbal memory, and written arithmetic. Age, learning disabilities, psychi-atric comorbidity, and gender could not account for these impairments.
Neuroimaging Studies
It is difficult to compare the results of neuroimaging studies of juvenile and adult ADHD; whereas nearly all the juvenile studies have used structural imaging, all of the adult ADHD studies have used functional imaging. Struc-tural neuroimaging studies of ADHD juveniles suggest that circuitry involving prefrontal cortex, the striatum, cerebellum, and the corpus callosum are altered in ADHD (Castellanos 1997).
have primarily implicated frontal brain regions. In a positron emission tomography (PET) study of adult ADHD, Zametkin et al (1990) found reduced global and regional glucose metabolism in the premotor cortex and the superior prefrontal cortex. Although these findings were not fully replicated in a similar PET study of adolescents (Zametkin et al 1993), which used siblings of ADHD children as control subjects, they are consistent with brain single photon emission computed tomography (SPECT) imaging in ADHD adolescents (Amen et al 1993).
Ernst et al (1998) used PET with F18-DOPA to com-pare 17 ADHD adults and 23 healthy control adults. They used the ratio of the isotope concentration of specific regions to that of nonspecific regions to index DOPA decarboxylase activity and dopamine storage processes. Of three composite regions (prefrontal cortex, striatum, and midbrain), only the prefrontal cortex showed signifi-cantly lower F18-DOPA ratios in ADHD adults compared with control adults. The medial and left prefrontal areas were the most altered.
Anterior cingulate cortex (ACC), lying on the medial surface of the frontal lobe, has strong connections to dorsolateral prefrontal cortex. Bush et al (1999) used a Stroop task to compare ACC activation in ADHD and non-ADHD adults. In contrast to control subjects, the ADHD adults failed to activate the ACC. Notably, in the prior study by Zametkin et al (1990), cingulate cortex was one of only four (out of 60) regions evaluated that still showed regional hypoactivity after global normalization.
Because the stimulant medications are the treatment of choice for ADHD, several studies of ADHD adults exam-ined changes in brain metabolism due to stimulant admin-istration. They have not, however, produced consistent results (Ernst et al 1994; Matochik et al 1994; Matochik et al 1993). One study has used SPECT to assess dopamine transporter (DAT) activity in ADHD and control adults (Dougherty et al 1999). This study found DAT to be elevated by 70% in the ADHD adults compared with control adults, which is consistent with molecular genetic studies implicating DAT in ADHD (Faraone and Bieder-man 1999).
In summary, the available data suggest that ADHD adults show frontal dopaminergic hypoactivity. In con-trast, studies of adolescents show weaker results. Ernst et al (1998) offered two explanations of the differences between the adolescent and adult data. First, the adoles-cent samples studied may have been more heterogeneous than the adult samples. Whereas all of the adults had persistent ADHD, some of the adolescent cases might have remitted by adulthood. Thus, frontal dopaminergic hypoactivity may be associated with persistent ADHD
only. Alternatively, Ernst et al (1998) speculated that, because of brain maturation, the locus of ADHD’s dopa-mine abnormality might shift from the midbrain in child-hood to the prefrontal cortex in adults.
Course and Outcome
Do ADHD children grow up to become ADHD adults? If adult ADHD is a valid disorder, then follow-up studies of ADHD children should show that they grow up to become ADHD adults and that their persistence of ADHD symp-toms exceeds that seen in an appropriate control group. Prospective follow-up studies are not clouded by the ambiguities of retrospective reports. Thus, they are an essential for validating the adult ADHD diagnosis. If prospective studies do not find ADHD persisting into adulthood, then the ADHD diagnoses given to clinically referred adults would be suspect.
The idea that ADHD remits by adulthood was given credibility by Hill and Schoener (1996), who fit a math-ematic model to the rates of persistence reported by studies following ADHD children from childhood into adolescence or adulthood. Their model predicted an expo-nential decline in the rate of ADHD. It suggested that 99% of ADHD children would go into remission by the age of 20. Because the prevalence of ADHD in childhood is between 5 and 10%, their results predict that the preva-lence of ADHD in adulthood should range from 5 to 10 per 10,000 adults. Their paper, which concluded that ADHD essentially disappears in adulthood, generated some controversy because of some of its methodological features (Barkley 1997) and for its inconsistency with clinical studies suggesting adult ADHD to have a nonneg-ligible prevalence.
One problem with Hill and Schoener’s paper is that they only included studies that defined subjects as having persistent ADHD if they met full criteria for the disorder. This method counts as “remitted” former ADHD children who continue to have impairing symptoms despite failing to meet all diagnostic criteria (cases that DSM-IV would code as ADHD in partial remission). Thus, Hill and Schoener studied what Keck et al (1998) called syndro-matic persistence (i.e., the maintenance of full diagnostic status). They did not address symptomatic persistence (i.e., the maintenance of partial diagnostic status with impairment).
would seem much better than we know it to be from studies of symptomatic persistence.
Two prior studies suggest that studies of syndromatic persistence may underestimate the persistence of ADHD. Fischer (1997) observed 148 hyperactive children for 15 years. At a mean age of 21, self-reports from these subjects found only 3% meeting criteria for DSM-III-R ADHD. When Fischer used a psychometric criterion to define ADHD (symptoms exceeding the 93rd percentile of severity of the control group), 25% met criteria for ADHD. The clinical meaningfulness of the persistent ADHD symptoms was confirmed by parent reports sug-gesting that 42% of the grown-up ADHD children still met criteria for the disorder.
In a longitudinal study of ADHD boys, Biederman et al (2000) found that by age 19, 38% of children had the full ADHD diagnosis, 72% showed persistence of at least one third of the symptoms required for the diagnosis, and 90% showed evidence of clinically significant impairment. Consistent with these studies, other follow-up studies show that the persistence of ADHD into adulthood ranges from 4% to 80%, depending on the length of follow-up and the definition of persistence (Barkley 1998).
Arguing against the idea that ADHD disappears in adulthood is a report by Murphy and Barkley (1996a), using self-report rating scales to diagnose ADHD in 720 adults applying for drivers licenses. In this sample, 4.7% of adults met DSM-IV criteria for childhood onset ADHD. Similarly, Heiligenstein et al (1998) examined ADHD diagnoses and symptom scores among 448 college stu-dents not selected for any psychiatric diagnosis. Of these students, 4% met DSM-IV criteria for ADHD. Notably, these two studies agree with family studies that have examined the prevalence of ADHD among the parents of non-ADHD children. When examined together, these studies show that 7.5% of fathers and 3% of mothers of non-ADHD children have childhood-onset ADHD (Fara-one and Biederman 1999).
Summary and Future Directions
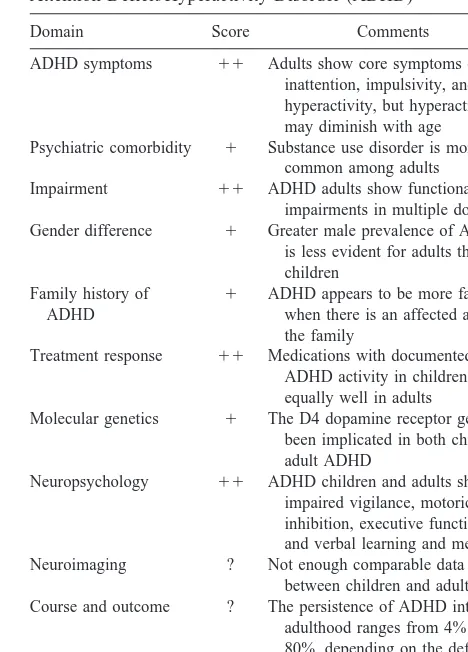
This article has examined the validity of adult ADHD using the validity criteria of Robins and Guze (1970): clinical correlates, family history, treatment response, laboratory studies, course, and outcome. Table 1 summa-rizes our review by giving each domain of study a score: 11 means that results strongly support the validity of adult ADHD,1means that results support the validity of adult ADHD, ? means that results are equivocal,2means that results do not support the validity of adult ADHD, and – means that results strongly argue against the validity of adult ADHD. As the table indicates, no domain was rated2or –, four were rated11, five were rated1, and
two were rated ?. The predominance of positive findings suggests that adult ADHD is a valid disorder, but because all areas are not strongly supportive, more work is needed to clarify this issue.
The clinical correlates of ADHD are similar for children and adults. ADHD adults are impulsive, inattentive, and restless. They have the clinical “look and feel” of ADHD children. Furthermore, like their childhood counterparts, many adults with ADHD suffer from antisocial, depres-sive, and anxiety disorders and show evidence of clinically significant impairments in histories of school failure, occupational problems, and traffic accidents. Treatment response studies show that the medications used to treat childhood ADHD are equally effective for adult ADHD.
Family studies provide strong support for the validity of adult ADHD: adult relatives of ADHD children are at increased risk for ADHD as are the child relatives of ADHD adults. Both childhood and adult ADHD show a characteristic profile of neuropsychologic deficits. More-over, an emerging neuroimaging literature implicates pre-frontal dopaminergic hypoactivity in adult ADHD.
Al-Table 1. Summary of Evidence for the Validity of Adult Attention-Deficit/Hyperactivity Disorder (ADHD)
Domain Score Comments
ADHD symptoms 11 Adults show core symptoms of inattention, impulsivity, and hyperactivity, but hyperactivity may diminish with age Psychiatric comorbidity 1 Substance use disorder is more
common among adults Impairment 11 ADHD adults show functional
impairments in multiple domains Gender difference 1 Greater male prevalence of ADHD is less evident for adults than for children
Family history of ADHD
1 ADHD appears to be more familial when there is an affected adult in the family
Treatment response 11 Medications with documented anti-ADHD activity in children work equally well in adults
Molecular genetics 1 The D4 dopamine receptor gene has been implicated in both child and adult ADHD
Neuropsychology 11 ADHD children and adults show impaired vigilance, motoric inhibition, executive functions, and verbal learning and memory Neuroimaging ? Not enough comparable data
between children and adults Course and outcome ? The persistence of ADHD into adulthood ranges from 4% to 80%, depending on the definition of persistence
though this is consistent with the putative role of dopamine in the etiology of ADHD (Faraone and Bieder-man 1998), much more work is needed to determine the evolution of ADHD’s dopamine abnormalities from child-hood to adultchild-hood.
These converging lines of evidence from studies of clinical correlates, family history, treatment response, and laboratory measures provide support for the validity of ADHD in adults. Nevertheless, some areas of ambiguity remain. The psychiatric comorbidity of ADHD adults raises questions about false positive diagnoses and diver-gent validity. Thus, we need follow-up studies of ADHD adults with comorbid disorders to determine if ADHD, the comorbid disorder, or both persist over time. We also need studies using psychiatric control subjects to determine if the clinical or neurobiological features of specific disor-ders vary between ADHD and non-ADHD adults.
Although false positive diagnoses are an issue for all disorders, the problem may be more acute for adult ADHD, given that many adult ADHD patients are self-diagnosed when the first seek clinical help. This situation occurs because adult ADHD has received much media attention. Thus, adults seeking to justify their life prob-lems with a diagnostic label may be biased to see ADHD symptoms in themselves. Future research could address this issue by comparing self-referred cases of adult ADHD with cases that are diagnosed in adults who seek help without already thinking they have ADHD. Until this issue is resolved, however, clinicians should take extra care in assessing the childhood onset, chronicity, and impairment of ADHD symptoms in self-diagnosed referrals.
Given that follow-up studies of ADHD children have yielded ambiguous results, more work is also needed to evaluate the long-term outcome of ADHD children. These studies should determine the clinical and neurobiological features that differentiate cases of ADHD that persist into adulthood from those who go into remission. Because the ambiguity of follow-up studies is in part due to differences in how researchers have defined the persistence of ADHD, future work should focus on how best to diagnose ADHD in adults. Two diagnostic questions require further atten-tion: 1) should the age at onset criterion of ADHD be modified? and 2) what type and number of symptoms should be required to define an adult as having ADHD?
Although DSM-IV requires ADHD to onset by age 7, recent papers have challenged the validity of this age-at-onset criterion (AOC). Barkley and Biederman (1997) noted that recall of age at onset had low reliability and that there was little empirical evidence for the AOC required by DSM-IV. The most comprehensive assessment of the AOC for ADHD was provided by the DSM-IV field trials (Applegate et al 1997), which showed that many subjects met symptom criteria for ADHD but did not satisfy the
AOC. Requiring an AOC of 7 reduced the accuracy of identifying currently impaired cases of ADHD and also reduced agreement with clinician judgments. The authors concluded that further research should evaluate the value of the AOC for ADHD and identified three alternative strategies: 1) drop the AOC; 2) drop the requirement that symptoms at the AOC are impairing, and 3) keep the impairment criterion but raise the AOC. They also noted that a separate AOC rule for the inattentive subtype should be considered.
Unlike the AOC, the demarcation of symptom thresh-olds for defining ADHD received much empirical support from the DSM-IV Field trials through extensive psycho-metric studies (Lahey et al 1994). Lahey and colleagues’ careful validation of symptom thresholds in children justifies the use of DSM-IV criteria when documenting the childhood onset of ADHD in adults, but we know little about the validity of DSM-IV symptom thresholds for diagnosing the current status of ADHD in an adult meeting DSM-IV criteria for childhood onset ADHD. The authors of DSM-IV did recognize the existence of clinically meaningful cases of ADHD that do not meet full criteria. These cases are included in the category of ADHD “in partial remission,” reserved for “individuals (especially adolescents and adults) who currently have symptoms but no longer meet full criteria.” Although clinically sensible, this category has not been validated with empirical studies. Thus, for adult ADHD, the question of appropriate diagnostic criteria is complex. It requires attention to the AOC and to the symptom threshold used to define case-ness. These uncertainties in the diagnosis of adult ADHD highlight a more general issue for psychiatry—the devel-opmental sensitivity of DSM-IV (Faraone, in press). DSM-IV accommodates developmental changes in the expression of ADHD in several ways. It cautions diagnos-ticians that, with maturation, symptoms become less con-spicuous. Older children may be restless and fidgety but not overly hyperactive. With age, inattention may predom-inate as tasks at school require increasing levels of attention (Millstein et al 1997). The DSM only counts symptoms that are inconsistent with the patient’s develop-mental level. Although few would argue with this latter point, there is little normative data to guide clinicians about the degree to which ADHD symptoms in adults are not consistent with their developmental level.
irritabil-ity, loss of interest, insomnia, and so forth. The problem with performances that are difficult in childhood is that they are often easy in adulthood. Thus, developmental changes may make it more difficult for ADHD children to meet criteria for ADHD as they get older.
The performance-based diagnosis of ADHD is consis-tent with neuropsychologic models of ADHD that stress executive function impairment as a fundamental deficit in ADHD at all ages (Barkley and Biederman 1997; Penning-ton and Ozonoff 1996; Seidman et al 1998). These deficits include impairments in working memory (verbal and nonverbal), self-regulation (affect, motivation, and arous-al), and the ability to analyze behavior and synthesize novel responses. Barkley (1997) has written that a sense of time and flexible access to memory is required to analyze data of past consequences and to synthesize new patterns of behavior. These capacities allow an individual to move from reacting to immediate environmental concerns to pursue future, purposeful goals. Thus, executive function deficits are expected to lead to performance deficits, the nature of which will depend on the environmental chal-lenges faced by the patient. The administrative and mul-titasking demands faced by adults are qualitatively differ-ent from those faced by children, who function in more structured family and school settings. As opposed to tasks in early childhood that predominately require simple responses to focused demands, the demands of adulthood require juggling of competing tasks, independence, orga-nization, and planning. This suggests that future revisions of the DSM test a set of symptoms that are appropriate for the challenges faced by ADHD adults.
These considerations have led Barkley (1998) to sug-gest that ADHD be recast as a norm-referenced rather than a criterion-referenced diagnosis. From this perspective, we should deal with the diagnosis of ADHD as we do the construct of intelligence. We would not have adults complete the Wechsler Intelligence Scales for Children and then conclude that intelligence increases with age. Instead, we use different test batteries for different age groups and within a single battery; we consider a score high or low in reference to people of the same age. If this idea is correct, then the debate about adult ADHD will not be solved by a new slew of conflicting studies. Research needs to focus not only on the validity of the disorder, but also on the validity of the theoretic assumptions and empiric data that buttress the diagnosis.
This work was supported in part by National Institute of Mental Health Grants Nos. R01MH57934, R01HD37694, and R01HD37999 (SVF).
References
Alpert J, Maddocks A, Nierenberg A, O’Sullivan R, Pava J, Worthington J, et al (1996): Attention deficit hyperactivity disorder in childhood among adults with major depression.
Psychiatry Res 62:213–219.
Alterman AI, Petrarulo E, Tarter R, McGowan JR (1982): Hyperactivity and alcoholism: Familial and behavioral corre-lates. Addict Behav 7:413– 421.
Amen D, Paldi J, Thisted R (1993): Brain SPECT imaging. J Am
Acad Child Adolesc Psychiatry 32:1080 –1081.
American Psychiatric Association (1994): Diagnostic and
Sta-tistical Manual of Mental Disorders, 4th ed. Washington, DC:
American Psychiatric Association.
Applegate B, Lahey B, Hart E, Biederman J, Hynd G, Barkley R, et al (1997): Validity of the age of onset criterion for attention-deficit/hyperactivity disorder: A report from the DSM-IV field trials. J Am Acad Child Adolesc Psychiatry 36:1211–1221.
Asghari V, Sanyal S, Buchwaldt S, Paterson A, Jovanovic V, Van Tol HH (1995): Modulation of intracellular cyclic AMP levels by different human dopamine D4 receptor variants.
J Neurochem 65:1157–1165.
August GJ, Stewart MA, Holmes CS (1983): A four-year follow-up of hyperactive boys with and without conduct disorder. Br J Psychiatry 143:192–198.
Barkley R (1997): Age dependent decline in ADHD: True recovery or statistical illusion? ADHD Rep 5:1–5.
Barkley R, Murphy K, Kwasnik D (1996a): Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics 98:1089 –1095. Barkley R, Murphy K, Kwasnik D (1996b): Psychological
adjustment and adaptive impairments in young adults with ADHD. J Attention Disord 1:41–54.
Barkley RA (1998): Attention Deficit Hyperactivity Disorder: A
Handbook for Diagnosis and Treatment. New York:
Guil-ford.
Barkley RA, Biederman J (1997): Toward a broader definition of the age-of-onset criterion for attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 36:1204 – 1210.
Barkley RA, Grodzinsky G, DuPaul GJ (1992): Frontal lobe functions in attention deficit disorder with and without hyperactivity: a review and research report. J Abnorm Child
Psychol 20:163–188.
Biederman J, Baldessarini RJ, Wright V, Knee D, Harmatz J (1989): A double-blind placebo controlled study of desipra-mine in the treatment of attention deficit disorder: I. Efficacy.
J Am Acad Child Adolesc Psychiatry 28:777–784.
Biederman J, Faraone SV, Knee D, Munir K (1990): Retrospec-tive assessment of DSM-III attention deficit disorder in non-referred individuals. J Clin Psychiatry 51:102–106. Biederman J, Faraone SV, Milberger S, Curtis S, Chen L, Marrs
A, et al (1996): Predictors of persistence and remission of ADHD: Results from a four-year prospective follow-up study of ADHD children. J Am Acad Child Adolesc Psychiatry 35:343–351.
Biederman J, Faraone SV, Spencer T, Wilens T, Norman D, Lapey KA, et al (1993): Patterns of psychiatric comorbidity, cognition, and psychosocial functioning in adults with atten-tion deficit hyperactivity disorder. Am J Psychiatry 150: 1792–1798.
Biederman J, Faraone SV, Taylor A, Sienna M, Williamson S, Fine C (1998): Diagnostic continuity between child and adolescent ADHD: Findings from a longitudinal clinical sample. J Am Acad Child Adolesc Psychiatry 37:305–313. Biederman J, Mick E, Faraone SV (2000): Age dependent
decline of ADHD symptoms revisited: impact of remission definition and symptom subtype. Am J Psychiatry 157:816 – 818.
Biederman J, Newcorn J, Sprich S (1991): Comorbidity of attention deficit hyperactivity disorder with conduct, depres-sive, anxiety, and other disorders. Am J Psychiatry 148:564 – 577.
Biederman J, Wilens T, Mick E, Milberger S, Spencer T, Faraone S (1995): Psychoactive substance use disorder in adults with attention deficit hyperactivity disorder: Effects of ADHD and psychiatric comorbidity. Am J Psychiatry 152:1652–1658. Biederman J, Wilens T, Mick E, Spencer T, Faraone SV (1999):
Pharmacotherapy of attention-deficit/hyperactivity disorder reduces risk for substance use disorder. Pediatrics 104:e20. Biederman J, Wilens TE, Mick E, Faraone SV, Weber W, Curtis
S, et al (1997): Is ADHD a risk factor for psychoactive substance use disorders? Findings from a four-year prospec-tive follow-up study. J Am Acad Child Adolesc Psychiatry 36:21–29.
Borland BL, Heckman HK (1976): Hyperactive boys and their brothers: A 25-year follow-up study. Arch Gen Psychiatry 33:669 – 675.
Buchsbaum MS, Haier RJ, Sostek AJ, Weingartner H, Zahn TP, Siever LJ, et al (1985): Attention dysfunction and psychopa-thology in college men. Arch Gen Psychiatry 42:354 –360. Bush G, Frazier JA, Rauch SL, Seidman LJ, Whalen PJ, Jenike
MA, et al (1999): Anterior cingulate cortex dysfunction in attention deficit/hyperactivity disorder revealed by fMRI and the counting stroop. Biol Psychiatry 45:1542–1552. Castellanos FX (1997): Toward a pathophysiology of
attention-deficit/hyperactivity disorder. Clin Pediatr 36:381–393. De Obaldia R, Parsons O (1984): Relationship of
neuropsycho-logical performance to primary alcoholism and self-reported symptoms of childhood minimal brain dysfunction. J Stud
Alcohol 45:386 –391.
Dougherty DD, Bonab AA, Spencer TJ, Rauch SL, Madras BK, Fischman AJ (1999): Dopamine transporter density is ele-vated in patients with ADHD. Lancet 354(9196):2132–2133. Downey K, Stelson F, Pomerleau O, Giordiani B (1997): Adult attention deficit hyperactivity disorder: Psychological test profiles in a clinical population. J Nerv Ment Dis 185:32–38. Ernst M, Zametkin A, Matochik J, Jons P, Cohen R (1998): DOPA decarboxylase activity in attention deficit hyperactiv-ity disorder adults. A [fluorine-18]fluorodopa positron emis-sion tomographic study. J Neurosci 18:5901–5907.
Ernst M, Zametkin A, Matochik J, Liebenauer L, Fitzgerald G, Cohen R (1994): Effects of intravenous dextroamphetamine on brain metabolism in adults with attention-deficit/hyperac-tivity disorder (ADHD). Preliminary findings.
Psychophar-macology 30:219 –225.
Eyre S, Rounsaville B, Kleber H (1982): History of childhood hyperactivity in a clinical population of opiate addicts. J Nerv
Ment Dis 170:522–529.
Faraone S, Biederman J (1994): Is attention deficit hyperactivity disorder familial? Harvard Rev Psychiatry 1:271–287. Faraone S, Biederman J, Mick E (1997): Symptom reports by
adults with attention deficit hyperactivity disorder: Are they influenced by attention deficit hyperactivity disorder in their children? J Nerv Ment Dis 185:583–584.
Faraone SV (in press): Attention deficit hyperactivity disorder in adults: Implications for theories of diagnosis. Curr Dir
Psychol Sci.
Faraone SV, Biederman J (1998): Neurobiology of attention-deficit hyperactivity disorder. Biol Psychiatry 44:951–958. Faraone SV, Biederman J (1999): The neurobiology of attention
deficit hyperactivity disorder. In: Charney DS, Nestler EJ, Bunney BS, editors. Neurobiology of Mental Illness. New York: Oxford University Press, 788 – 801.
Faraone SV, Biederman J, Monuteaux MC (2000): Toward guidelines for pedigree selection in genetic studies of atten-tion deficit hyperactivity disorder. Genet Epidemiol 18:1–16. Faraone SV, Biederman J, Weiffenbach B, Keith T, Chu MP, Weaver A, et al (1999): Dopamine D4 gene 7-repeat allele and attention deficit hyperactivity disorder. Am J Psychiatry 156:768 –770.
Fischer M (1997): The persistence of ADHD into adulthood: It depends on whom you ask. ADHD Rep 5:8 –10.
Gansler DA, Fucetola R, Krengel M, Stetson S, Zimering R, Makary C (1998): Are there cognitive subtypes in adult attention deficit/hyperactivity disorder? J Nerv Ment Dis 186:776 –781.
Gaub M, Carlson CL (1997): Gender differences in ADHD: A meta-analysis and critical review. J Am Acad Child Adolesc
Psychiatry 36:1036 –1045.
Gittelman R, Mannuzza S, Shenker R, Bonagura N (1985): Hyperactive boys almost grown up: I. Psychiatric status. Arch
Gen Psychiatry 42:937–947.
Gualtieri CT, Ondrusek MG, Finley C (1985): Attention deficit disorders in adults. Clin Neuropharmacol 8:343–356. Heiligenstein E, Conyers LM, Berns AR, Miller MA, Smith MA
(1998): Preliminary normative data on DSM-IV attention deficit hyperactivity disorder in college students. J Am Coll
Health 46:185–188.
Heiligenstein E, Guenther G, Levy A, Savino F, Fulwiler J (1999): Psychological and academic functioning in college students with attention deficit hyperactivity disorder. J Am
Coll Health 47:181–185.
Heiligenstein E, Johnston HF, Nielsen JK (1996): Pemoline therapy in college students with attention deficit hyperactivity disorder: A retrospective study. J Am Coll Health 45:35–39. Heiligenstein E, Keeling RP (1995): Presentation of unrecog-nized attention deficit hyperactivity disorder in college stu-dents. J Am Coll Health 43:226 –228.
Hill J, Schoener E (1996): Age-dependent decline of attention deficit hyperactivity disorder. Am J Psychiatry 153:1143–1146. Hinshaw SP (1992): Externalizing behavior problems and aca-demic underachievement in childhood and adolescence: Causal relationships and underlying mechanisms. Psychol
Holdnack JA, Moberg PJ, Arnold SE, Gur RC, Gur RE (1995): Speed of processing and verbal learning deficits in adults diagnosed with attention deficit disorder. Neuropsychiatry
Neuropsychol Behav Neurol 8:282–292.
Katz LJ, Wood DS, Goldstein G, Auchenbach RC, Geckle M (1998): The utility of neuropsychological tests in evaluation of Attention-deficit/hyperactivity disorder (ADHD) versus depression in adults. Assessment 5:45–52.
Keck P, McElroy S, Strakowski S, West S, Sax K, Hawkins J, et al (1998): 12-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am J
Psychiatry 155:646 – 652.
Klee S, Garfinkel B, Beauchesne H (1986): Attention deficits in adults. Psychiatr Ann 16:52–56.
Kovner R, Budman C, Frank Y, Sison C, Lesser M, Halperin J (1998): Neuropsychological testing in adult attention deficit hyperactivity disorder: A pilot study. Int J Neurosci 96:225–235. Lahey B, Applegate B, McBurnett K, Biederman J, Greenhill L, Hynd G, et al (1994): DSM-IV field trials for attention deficit hyperactivity disorder in children and adolescents. Am J
Psychiatry 151:1673–1685.
Levin FR, Evans SM, McDowell DM, Kleber HD (1998): Methylphenidate treatment for cocaine abusers with adult attention-deficit/hyperactivity disorder: a pilot study. J Clin
Psychiatry 59:300 –305.
Lovejoy DW, Ball JD, Keats M, Stutts ML, Spain E, Janda L, et al (1999): Neuropsychological performance of adults with attention deficit hyperactivity disorder (ADHD): Diagnostic classification estimates for measures of frontal lobe/executive functioning. J Int Neuropsychol Soc 5:222–233.
Manshadi M, Lippmann S, O’Daniel R, Blackman A (1983): Alcohol abuse and attention deficit disorder. J Clin
Psychia-try 44:379 –380.
Matochik J, Liebenauer L, King A, Szymanski H, Cohen R, Zametkin A (1994): Cerebral glucose metabolism in adults with attention deficit hyperactivity disorder after chronic stimulant treatment. Am J Psychiatry 151:658 – 664. Matochik JA, Nordahl TE, Gross M, Semple WE, King AC,
Cohen RM, et al (1993): Effects of acute stimulant medica-tion on cerebral metabolism in adults with hyperactivity.
Neuropsychopharmacology 8:377–386.
Mattes JA, Boswell L, Oliver H (1984): Methylphenidate effects on symptoms of attention deficit disorder in adults. Arch Gen
Psychiatry 41:1059 –1063.
Millstein R, Wilens T, Biederman J, Spencer T (1997): Present-ing ADHD symptoms and subtypes in clinically referred adults with ADHD. J Attention Disord 2:159 –166.
Morrison JR (1980a): Adult psychiatric disorders in parents of hyperactive children. Am J Psychiatry 137:825– 827. Morrison JR (1980b): Childhood hyperactivity in an adult
psychiatric population: Social factors. J Clin Psychiatry 41:40 – 43.
Murphy K, Barkley R (1996a): Prevalence of DSM-IV symp-toms of ADHD in adult licensed drivers: Implications for clinical diagnosis. J Attention Disord 1:147–161.
Murphy K, Barkley RA (1996b): Attention deficit hyperactivity disorder adults: Comorbidities and adaptive impairments.
Compr Psychiatry 37:393– 401.
Pennington BF, Ozonoff S (1996): Executive functions and
developmental psychopathology. J Child Psychol Psychiatry 37:51– 87.
Ratey J, Greenberg M, Bemporad J, Lindem K (1992): Unrec-ognized attention-deficit hyperactivity disorder in adults pre-senting for outpatient psychotherapy. J Child Adolesc
Psy-chopharmacol 2:267–275.
Robins E, Guze SB (1970): Establishment of diagnostic validity in psychiatric illness: Its application to schizophrenia. Am J
Psychiatry 126:983–987.
Seidman LJ, Biederman J, Faraone SV, Weber W, Ouellette C (1997): Toward defining a neuropsychology of attention deficit-hyperactivity disorder: Performance of children and adolescents from a large clinically referred sample. J Consult
Clin Psychol 65:150 –160.
Seidman LJ, Biederman J, Weber W, Hatch M, Faraone SV (1998): Neuropsychological function in adults with attention-deficit hyperactivity disorder. Biol Psychiatry 44:260 –268. Shekim WO, Asarnow RF, Hess E, Zaucha K, Wheeler N
(1990): A clinical and demographic profile of a sample of adults with attention deficit hyperactivity disorder, residual state. Compr Psychiatry 31:416 – 425.
Silverstein SM, Como PG, Palumbo DR, West LL, Osborn LM (1995): Multiple sources of attentional dysfunction in adults with Tourette’s syndrome: Comparison with attention deficit-hyperactivity disorder. Neuropsychology 9:157–164. Spencer T, Biederman J, Wilens T (1994a): Tricyclic
antidepres-sant treatment of children with ADHD and tic disorders. J Am
Acad Child Adolesc Psychiatry 33:1203–1204.
Spencer T, Biederman J, Wilens T, Faraone S (1994b): Is attention deficit hyperactivity disorder in adults a valid disorder? Harvard Rev Psychiatry 1:326 –335.
Spencer T, Biederman J, Wilens T, Prince J, Hatch M, Jones J, et al (1998): Effectiveness and tolerability of tomoxetine in adults with attention deficit hyperactivity disorder. Am J
Psychiatry 155:693– 695.
Spencer T, Wilens T, Biederman J, Bostic J, Prince J, Gerard K, et al (1999, October): Efficacy and tolerability of a mixed amphet-amine salts compound in adults with attention deficit hyperac-tivity disorder. Paper presented at the 46th annual meeting of the American Academy of Child and Adolescent Psychiatry, Chi-cago.
Spencer T, Wilens T, Biederman J, Faraone SV, Ablon JS, Lapey K (1995): A double-blind, crossover comparison of methyl-phenidate and placebo in adults with childhood-onset atten-tion-deficit hyperactivity disorder. Arch Gen Psychiatry 52: 434 – 443.
Spencer TJ, Biederman J, Wilens T, Harding M, O’Donnell D, Griffin S (1996): Pharmacotherapy of attention deficit hyper-activity disorder across the lifecycle: A literature review.
J Am Acad Child Adolesc Psychiatry 35:409 – 432.
Tarter RE (1982): Psychosocial history, minimal brain dysfunc-tion and differential drinking patterns of male alcoholics.
J Clin Psychol 38:867– 873.
Taylor CJ, Miller DC (1997): Neuropsychological assessment of attention in ADHD adults. J Attention Disord 2:77– 88. Wender PH, Reimherr FW, Wood DR, Ward M (1985): A
controlled study of methylphenidate in the treatment of attention deficit disorder, residual type, in adults. Am J
Wilens T, Biederman J (1992): The stimulants. Psychiatr Clin
North Am 15:191–222.
Wilens TE, Biederman J, Mick E (1998): Does ADHD impact the course of substance abuse? Findings from a sample of adults with and without ADHD. Am J Addict 7:156 –163. Wilens TE, Biederman J, Mick E, Spencer T (1995): A
system-atic assessment of tricyclic antidepressants in the treatment of adult attention-deficit hyperactivity disorder. J Nerv Ment Dis 183:48 –50.
Wilens TE, Biederman J, Prince J, Spencer TJ, Faraone SV, Warburton R, et al (1996): Six-week, double-blind, place-bo-controlled study of desipramine for adult attention deficit hyperactivity disorder. Am J Psychiatry 153:1147– 1153.
Wilens TE, Biederman J, Spencer TJ, Frazier J, Prince J, Bostic
J, et al (1999): Controlled trial of high doses of pemoline for adults with attention-deficit/hyperactivity disorder. J Clin
Psychopharmacol 19:257–264.
Wood DR, Reimherr FW, Wender PH, Johnson GE (1976): Diagnosis and treatment of minimal brain dysfunction in adults: A preliminary report. Arch Gen Psychiatry 33:1453– 1460.
Zametkin A, Liebenauer L, Fitzgerald G, King A, Minkunas D, Herscovitch P, et al (1993): Brain metabolism in teenagers with attention-deficit hyperactivity disorder. Arch Gen
Psy-chiatry 50:330 –340.