SELF-REPORTED DRUG ALLERGIES IN SURGICAL
POPULATION IN SERBIA
Jelena Veličković1,2, Ivan Palibrk1,2, Bojana Miljković1, Dejan Veličković2,3, Bojan Jovanović1,2, Vesna Bumbaširević1,2, Marija Djukanović1 and Vladimir Šljukić3
1Department of Anesthesiology, Clinical Centre of Serbia; 2University of Belgrade, School of Medicine; 3Clinical Department of Digestive Surgery, Clinical Center of Serbia, Belgrade, Serbia
SUMMARY – History of drug allergy is of major concern during perioperative period. Medical records usually lack documents confirming the stated allergy. This study aimed to investigate the prevalence of self-reported drug allergies and their characteristics in adult Serbian surgical popu-lation, and to analyze their influence on drug prescription during perioperative period. The study enrolled patients scheduled for general surgery during a one-year period at a tertiary care hospital. They were questioned using a structured questionnaire about the existence of drug allergy and its nature. Medical records were examined after discharge to assess medical prescription during hos-pitalization. Of 1126 patients evaluated during the study period, 434 (38.5%) reported a total of 635 drug reactions. The most common allergy claim was to antibiotics (68%), nonsteroidal antiin-flammatory drugs (16.4%) and iodine (3.9%). Women, urban residents and herbal drug consumers were more likely to state an allergy. The majority of reported reactions were cutaneous (72%) and respiratory (34%), while anaphylaxis was reported by 3.2% of patients. Only 38 (8.7%) patients had previously undergone any allergology testing. Retrospective chart review revealed that 26 (6%) pa-tients were administered the drug to which they had reported allergic reaction in the past, with no adverse effects. Drug allergies are frequently self-reported in surgical population in Serbia, which is in contrast to a very low rate of explored and documented allergies. In order not to deny an effective treatment or postpone a surgery, health care practitioners should pay more attention to an accurate classification of adverse drug reactions.
Key words: Drug hypersensitivity; Hypersensitivity; Drug-related side effects and adverse reactions; Surveys and questionnaires; Surgery department, hospital; Serbia
Correspondence to: Assist. Prof. Jelena Veličković, MD, Depar-tment of Anesthesiology, Clinical Centre of Serbia, Koste Todo-rovića 6, 11000 Belgrade, Serbia
E-mail: lelavelickovic@gmail.com
Received March 26, 2015, accepted August 24, 2015
Introduction
Information regarding the history of allergies is contained in every medical record. It is obtained by almost every health care provider being in contact with patient at any level of health care. Since patients are exposed to a variety of drugs during perioperative period, a history of drug hypersensitivity is of major concern in surgical and anesthetic practice1.
Drug hypersensitivity reactions (DHR) represent adverse effects of drugs taken at a dose tolerated by normal subjects2.DHR comprise approximately
10%-15% of all adverse drug reactions. According to the nomenclature recommended by the World Allergy Organization, drug allergies are defined as hypersen-sitivity reactions with clearly defined immune back-ground3.Most of the patients are unaware of that fact,
so it is clear that they label any unexpected or adverse drug effect as ‘allergic reaction’4.Furthermore, medical
records usually include only the patient’s statement on the existence of drug allergy and the implicated drug but not details about previous reaction or allergology diagnostic work up, making the reliability of such
data questionable. Literature data reveal that both under-reporting and over-diagnosis of DHR (due to inappropriate use of the term ‘allergy’) are present in clinical practice, which might have consequences on treatment choices and influence the quality of care5,6.
Low rate of reporting of adverse drug reactions to pharmacovigilance agencies makes the problem even more difficult to control7,8.
The aim of our survey was to assess the prevalence of self-reported drug allergies in adult surgical popu-lation in Serbia, to explore their characteristics and investigate to what degree they influence drug pre-scription during perioperative period.
Materials and Methods
The survey was conducted during a one-year period (from April 2011 till March 2012) at the Department of Anesthesiology, Clinical Center of Serbia, Bel-grade. It enrolled consecutive adult patients scheduled for elective general surgery. Patients were questioned by their anesthetists during routine pre-anesthetic visit whether they had any allergy to report. Anesthe-tists had to complete a formatted questionnaire based on the European Network of Drug Allergy (ENDA) questionnaire adapted to perioperative needs and Ser-bian population (Fig. 1)9. The questionnaire contained
questions about the nature of previous allergic reac-tions, previous diagnostic work-up, and also recorded patient demographic and clinical data. An average time for completion of the questionnaire was 5 to 10 minutes. Medical records were examined afterwards to see whether the drugs prescribed conflicted with those self-reported as allergies. The term ‘allergy’ was used deliberately instead of ‘hypersensitivity’ since it is understandable and used by most patients.
Database was created and statistical analyses were performed using the SPSS software version 17.0. The level of statistical significance was set at p<0.05. For descriptive analysis data were expressed as proportions with their 95% confidence interval (CI) or means ± stan-dard deviations. Logistic regression analysis was carried out to determine risk factors for allergy self-reporting.
Results
During the study period, a total of 1126 patients, 627 (55.7%) men and 499 (44.3%) women, age range
19-83 (mean 58.9±15.5) years were evaluated. The ma-jority of patients were residents of urban areas (n=977; 86.8%) whereas 149 (13.2%) were from rural areas. Comorbidities were reported by 885 (78.6%) patients and 663 (58.8%) of them were treated with chronic therapy. In addition, 368 (32.7%) patients reported regular use of various herbal medications or dietary supplements, while 75 (6.7%) patients were diagnosed with a defined allergic disease (such as asthma, aller-gic rhinitis, chronic urticaria, etc.).
We found that 434 (38.5%) patients considered themselves allergic to at least one drug and they re-ported a total of 635 reactions. The most frequently implicated drugs were antibiotics, being responsible for 68% of the reported adverse events. Penicillins were involved in 302 (47.6%) reactions and they were by far the most commonly addressed allergens. Other antibiotics to which allergic reactions were frequently reported were sulfonamides (14.3%), cephalosporins (12.9%), macrolides (5.0%), tetracyclines (1.9%), and others (such as vancomycin or quinolones, 2.4%). Re-garding other drugs designated as responsible for al-lergic reaction, nonsteroidal antiinflammatory drugs (NSAIDs) were involved in 104 (16.4%) reactions, iodine in 25 (3.9%), contrast medium in 13 (2.1%), angiotensin-converting enzyme (ACE) inhibitors in 7 (1.1%), atropine in 4 (0.7%), calcium antagonists in 5 (0.8%), local anesthetics in 2 (0.3%), and latex in 3 (0.5%) reactions. Two patients reported allergic re-action to an undetermined anesthetic and it was not possible to identify whether the implicated event was to an intravenous anesthetic, muscle relaxant, an opi-oid, or some other drug (Fig. 2). These patients were referred for preoperative allergology testing (skin-prick tests), which revealed no allergy to the tested battery of agents for use during general anesthesia and perioperative period.
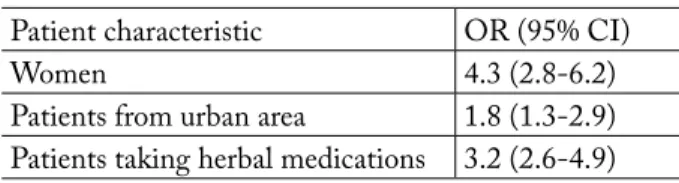
Logistic regression analysis revealed that women (OR=4.3, 95%CI=2.8-6.2), patients from urban areas (OR=1.8, 95%CI=1.3-2.9) and those regularly taking Table 1. Predictors of self-reported drug allergy
Patient characteristic OR (95% CI)
Women 4.3 (2.8-6.2)
Patients from urban area 1.8 (1.3-2.9)
herbal drugs (OR=3.2, 95%CI=2.6-4.9) were signifi-cantly more likely to claim a drug allergy (Table 1).
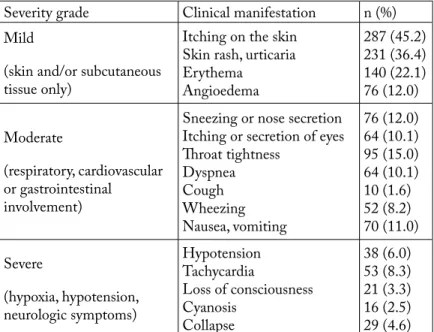
The most common clinical manifestations recalled by patients were cutaneous (72%), respiratory (34%), cardiovascular (18%) and gastrointestinal (11%), all of them being rather mild than severe. Anyway, 36 (3.2%) patients reported previous anaphylactic reac-tion with various presentareac-tions (Table 2).
Out of 635 self-reported allergic reactions, 80 (12.6%) occurred during the past year, 58 (9.1%) dur-ing the past 10 years, 208 (32.7%) reactions occurred 10-20 years before, while in the majority of cases (n=289; 45.5%) the claimed allergic reaction had oc-curred more than 20 years before.
Oral administration of drug preceded self-report-ed allergic reaction in 152 (23.9%) cases, while 483 (76.1%) reactions followed the parenteral route of drug administration. According to the patients’ an-swers, 432 (68.0%) reactions occurred at a healthcare institution, whereas 203 (32.0%) took place at home, usually after oral administration of the drug.
Almost 98% of study subjects (425/434) had com-pletely avoided the suspected agent thereafter. Only 38 of 434 (8.7%) patients with self-reported drug al-lergy underwent further allergology investigation and in 18 (4.1%) it was requested by the anesthetist prior to surgery. In 12 patients, the reported allergy was confirmed by allergology testing.
Questionnaire analysis showed that in 42.5% (270/635) of cases, anesthesiologists judged the re-ported drug allergy to be certain or probable, which was based on the responses about previous diagnostic work-up or reported symptoms highly suggestive of an allergy. The remaining self-reported allergies were associated with lower probability (possible, doubtful, unrelated) of a true allergic reaction as estimated by the attending anesthesiologist. The self-reported his-tory of allergy was noted in the official anesthesia chart, irrespective of this estimation.
Medical records after patient discharge revealed that 26 (6.0%) patients were administered a drug to which they claimed to be allergic during their hospital stay, with no adverse reactions. Antibiotic prophylaxis with cephalosporins was administered to 82% of the patients with reported allergy to penicillin and to 86% of those without reported allergy (p>0.05), with no adverse events recorded.
Discussion
The prevalence of self-reported drug allergy in our survey was 38.5%. Most studies performed in inpa-tients showed a higher incidence of self-reported al-lergies, ranging from 25% to 39%, than surveys con-ducted in the general population, where the prevalence was 7.8%-9.7%10-13.
Severity grade Clinical manifestation n (%)
Mild
(skin and/or subcutaneous tissue only)
Itching on the skin Skin rash, urticaria Erythema Angioedema 287 (45.2) 231 (36.4) 140 (22.1) 76 (12.0) Moderate (respiratory, cardiovascular or gastrointestinal involvement)
Sneezing or nose secretion Itching or secretion of eyes Throat tightness Dyspnea Cough Wheezing Nausea, vomiting 76 (12.0) 64 (10.1) 95 (15.0) 64 (10.1) 10 (1.6) 52 (8.2) 70 (11.0) Severe (hypoxia, hypotension, neurologic symptoms) Hypotension Tachycardia Loss of consciousness Cyanosis Collapse 38 (6.0) 53 (8.3) 21 (3.3) 16 (2.5) 29 (4.6) n (%) = number (%) of reported reactions
Table 2. Frequency of clinical
manifestations reported by patients and their severity grading
Fig. 1. History of allergy questionnaire used in the survey (translation from Serbian language). ALLERGY QUESTIONNAIRE
Protocol No:____________ Date: ______________ PATIENT:
Name______________________ Date of birth:______________________Age:_____________years Sex: M F Residence: Urban Rural Occupation:__________________________
PERSONAL HISTORY:
Diagnosis:______________________ Comorbidities: Y N ____________________________ Chronic therapy: Y N ______________________________________________ ASA:__________ Herbal medication or dietary supplement consumption: YN
Allergic diseases (asthma, pollinosis, atopic dermatitis, food allergy, chronic urticaria, etc.): Y N
HISTORY OF DRUG ALLERGY: Do you have drug allergy to report? YN
Suspected drug(s):___________________________________________________________________ Clinical manifestation of reported reaction
Cutaneous: Gastrointestinal and respiratory: Neurologic: Cardiovascular
Maculopapular rash Nose discharge and sneezing Paresthesia Tachycardia
Erythema Throat tightness Loss of consciousness Hypotension
Urticaria Itching or eye discharge Tinnitus Collapse
Angioedema Dyspnea Vertigo Arrhythmia
Pruritus only Cough Other Anaphylaxis
Other Wheezing Other
Nausea, vomiting Diarrhea
Management following drug reaction: No therapy Immediate treatment I don’t remember Where did drug allergy take place? Health care institution Home Other
Route of administration of suspected drug Oral Muscular Intravenous TopicalI don’t know
When did the allergic reaction happen? During the last 10 years 10-20 years ago More than 20 years ago Have you taken the suspected drug after the allergic reaction? Y N I don’t know
Have you taken a similar drug (that could cross react) after the allergic reaction? Y N I don’t know Have you undergone any allergology testing after the reaction? Y N
Which? Skin tests Blood analysis Provocation tests Other I don’t know
Probability of allergic reaction based on history and documentation:Certain Probable Possible Doubtful Unrelated/Not assessable
In agreement with other studies, antibiotics ac-counted for the majority of putative allergies in the present study. It is noteworthy that antibiotic consump-tion in Serbia is among the highest in Europe, and until recently antibiotic purchase was not restricted by country policy, making these drugs easily available for self-medication. The average antibiotic consumption in Europe is around 20 DDD/1000 inhabitants per day, while in Serbia it was 33.1 DDD/1000 inhabitants per day in 200614.The high antibiotic utilization may in
part explain the frequency of self-reported allergies to antibiotics. Beta-lactams and antibiotics with greater historical use had a higher ‘allergy prevalence’ in our survey. Previous studies have reported the suspected prevalence of allergy to penicillin to be between 0.7% and 8% of the general population15.Our data revealed
an even higher prevalence, probably due to over-re-porting since the majority of diagnoses were based solely on clinical history and patient judgment. The second most frequent allergy reported in our study was to NSAIDs, which is of concern to the anesthetists since these drugs are part of a common postoperative analgesic protocol. NSAIDs rarely cause true allergic reactions but are commonly involved in various type A adverse drug reactions, which are dose predictive such as nausea, gastrointestinal intolerance or pru-ritus16. Anyway, the use of aspirin and NSAIDs is
rarely accompanied by idiosyncratic adverse reactions, some of which can be extremely serious, e.g., toxic epidermal necrolysis, Stevens-Johnson syndrome or aseptic meningitis17. Since a specific IgE to NSAIDs
has not been identified, these hypersensitivity reac-tions are called anaphylactoid and are clinically indis-tinguishable from anaphylactic reactions18.Due to the
high benefit of aspirin use in primary and secondary prevention of coronary artery disease, several desensi-tization protocols for patients with hypersensitivity to aspirin and NSAIDs have been proposed19.Patients
in our survey typically designated a particular agent to be responsible for allergy with reported previous safe use of other NSAIDs. Other drugs of impor-tance during perioperative period where marked less frequently, with the exception of iodine radiocontrast media and latex. Allergies to anesthetic agents were mentioned extremely rarely and were always a subject of special attention.
In accordance with other studies, female
prepon-derance in allergy reporting was observed in our sur-vey as well19,20. Although data from human studies are
lacking, sex hormones might play a role since the ef-fect of estrogens on mast cell activation and allergic sensitization has been confirmed in animal studies21.
Patients from urban areas were more likely to claim a drug allergy in our population. Although it is ob-vious that air pollution in urban areas is responsible for a higher incidence of asthma in modern cities, we could not find valuable explanation for our finding. It also remains unclear why the self-reported allergies were three times more common among users of herbal medications. It is gender unrelated since we found no difference in the rate of herbal medication consump-tion between men and women. We made an assump-tion that some of them might cross-react with drugs and also that their concomitant use disabled distinc-tion of causal reladistinc-tion to putative allergy.
During questioning of our participants, we paid special attention to description of clinical features of the self-reported allergic reactions. As in the majority of reports, cutaneous reactions were the most com-mon presentation of stated allergy22,23. Other
symp-toms involving different sites were in the vast majority of cases mild and self-limited reactions. Meticulous analysis after completion of questionnaires revealed that in many cases the reported symptoms were well known adverse reactions to a drug believed to have caused an allergy. For example, reporting cough or an-gioedema was common in patients claiming an allergy to ACE inhibitors, or nausea and abdominal discom-fort in those with self-reported allergy to macrolides and tetracyclines. There was even a case of reporting a wanted and expected drug effect as an allergy, as in case of a patient reporting heavy sleepiness after diaz-epam consumption.
Diagnostic work-up in patients with hypersensitiv-ity drug reactions consists of detailed history taking, physical examination and laboratory testing imme-diately after reaction (total IgE, mastocyte tryptase, methylhistamine). Retrospective diagnosis after hy-persensitivity reaction is based on in vivo testing (skin tests), organ challenge tests, and in vitro testing (de-tection of allergen-specific IgE antibody and molec-ular-based allergy diagnosis)24,25.Skin tests represent
the cornerstone of identification of causative allergens and are regarded as the gold standard for detection of
IgE antibodies with demonstration of wheal and flare reaction. In practice, the rate of allergology tested subjects is far less than those with allergy claim.
A study conducted in the general population in Portugal demonstrated that about one half of partici-pants with stated allergy had undergone any diagnos-tic procedure; 22.7% of them were submitted to skin tests and 26% to blood analysis13. Analyzing surgical
population, Tamayo et al. report that two-thirds of patients were subjected to some allergy investigation and that in 66.7% the only diagnostic test was a skin prick test26. Our findings differ substantially, as only
38 (8.7%) patients had previous allergology testing with diagnosis confirmed in 12 of them. Bavbek et al. showed that just 3.2% of medical students in Turkey with self-reported hypersensitivity were referred to an allergologist27. We can assume that the results in
our survey could be explained by the low availability of allergology services in our country and the lack of guidelines for general practitioners covering this topic. Another reason might be the fact that clinical symp-toms in the majority of patients were mild, not caus-ing much worry and need for additional diagnosis.
The problem of an insufficient clinical character-ization of allergies in Serbia is reinforced by the fact that reporting adverse drug reactions is at a very low level. The official national institution for pharma-covigilance, the Agency for Medicine and Medical Devices of Serbia (ALIMS) announced that only 910 reports of adverse drug reactions were submitted in
2011 and only 102 in 200528. This fact probably
con-tributes to the over-reporting of drug allergies since all kinds of adverse reactions are labeled as allergies by patients and their health care practitioners.
Current guidelines of the European Society of Anaesthesiology on preoperative evaluation of the adult non-cardiac surgery patient suggest allergology testing only in patients with a positive clinical his-tory and those at risk of anaphylactic/anaphylactoid reaction during anesthesia29. In the absence of
diag-nostic work-up, facing with a patient claiming drug allergy, anesthesiologist must act as if the patient is really allergic, which means at least avoiding the claimed agent. Retrospective analysis of our practice revealed that 6% of our patients were administered the drug they marked as the causative agent for allergy. In most cases, the drug was antibiotic or analgesic and the most probable reasons for this malpractice were inadequately labeled allergy note in medical chart, or rejection of diagnosis of allergy by unconvincing patient history. Poor allergy documentation has been reported previously by other authors30.It is
interest-ing to note that none of the medical records examined in our survey contained a single description of a self-reported allergic reaction.
It is estimated that 40% of patients who are al-lergic to penicillin cross react with cephalosporins, influencing the choice of antibiotic for antibacterial prophylaxis31. The fact that there was a high rate of
positive history of allergy to penicillin in our survey did not influence the perioperative antibiotic pre-scription with no adverse effects. Antibiotic prophy-laxis was administered to all patients and the choice of antibiotic was guided by hospital protocol. In pa-tients with self-reported allergies to antibiotics, the antibiotic was chosen on discretion of the attending anesthesiologist. Many patients with claimed allergy to penicillin had received cephalosporins after the reported reaction and it was sufficient to exclude the allergy to cephalosporins. In cases where no similar drug was taken after the allergic reaction, the choice was made based on the estimated probability of a true allergy and was mainly influenced by the severity of previous reaction and documented history of allergic diseases. The assignment of self-reported allergy to a group with a certain level of probability was not made for diagnostic purposes and it did not influence fur-Fig. 2. Frequency of self-reported drug allergies in study
population (% of reported reactions).
Iodine, 3.9% Contrast medium, 2.1% ACE inhibitors, 1.1% Atropine, 0.6% Latex, 0.5% Others, 7.4% Antibiotics, 68.0% NSAIDs, 16.4%
ther actions as part of the protocol. The intention of this survey was not to assess the frequency of drug allergies by confirming it with subsequent allergology testing. Our goal was rather to determine the magni-tude of drug allergy self-reporting and to highlight the problem of mislabeling the predictable adverse drug reactions as allergies.
The results of our study show that self-reported drug allergies are prevalent in adult surgical popula-tion in Serbia, which obliges all health care workers dealing with the patient during perioperative period to avoid the drug claimed to have caused an allergy. On the other hand, the majority of these reactions are poorly documented and the information obtained from patients is unreliable. It creates a significant problem of denying an effective treatment and faces clinicians with the lack of an appropriate substitute in a limited resource setting. More detailed preoperative history taking can help anesthesiologist assess the validity of a stated reaction and decide on the probability of a true allergy. General practitioners are encouraged to report adverse drug reactions to pharmacovigilance agencies and to refer patients with suspected allergies to aller-gology testing for accurate diagnosis of drug allergy.
References
1. Veličković J, Lađević N, Milaković B, Lađević-Likić I, Ugrinović Đ, Kalezić N. Preoperative evaluation of patients with history of allergy. Acta Chir Iugoslav. 2011;58(2):177-83.
2. Demoly P, Marinella V, Rebelo Gomes E, Romano A. Epide-miology and causes of drug hypersensitivity. In: Pichler WJ, editor. Chemical Immunology and Allergy. Basel: Karger; 2007. p. 2-17.
3. Johansson S, Bieber T, Dahl R, Friedmann PS, Lanier BQ , Lockey RF, et al. Revised nomenclature for allergy for global use: report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol. 2004;113:832-6.
4. Becker DE. Preoperative medical evaluation: Part I: General principles and cardiovascular considerations. Anesth Prog. 2009;56:92-103.
5. Backstrom M, Mjorndal T, Dahlqvist R. Under-reporting of serious adverse drug reactions in Sweden. Pharmacoepide-miol Drug Saf. 2004;13:483-7.
6. Messaad D, Sahla H, Benahmed S, Godard P, Bousquet J, Demoly P. Drug provocation tests in patients with history suggesting an immediate drug hypersensitivity reaction. Ann Intern Med. 2004;140:1001-6.
7. Walewska Zielecka B, Religioni V, Religioni M. Monitoring of adverse drug reactions – the new regulations in Poland. Prog Health Sci. 2013;3(2):165-70.
8. Ilfat W, Shakeel S, Rahim N, Anjum F, Nesar S, Ghayas S. Pakistani physicians’ knowledge and attitude towards reporting adverse drug reactions. Afr J Pharm Pharmacol. 2014;8(14):379-85.
9. Demoly P, Kropf R, Bircher A, Pichler WJ. Drug hypersen-sitivity: questionnaire. EAACI interest group on drug hyper-sensitivity. Allergy. 1999;54:999-1003.
10. Peyriere H, Cassan S, Floutard E, Riviere S, Blayac JP, Hil-laire-Buys D, et al. Adverse drug events associated with hos-pital admission. Ann Pharmacother. 2003;37:5-11.
11. Jones TA, Como JA. Assessment of medication errors that involved drug allergies at a university hospital. Pharmaco-therapy. 2003;23:855-60.
12. Wyatt JP. Patients’ knowledge about their drug allergies. J Accid Emerg Med.1996;13:114-5.
13. Gomes E, Cardoso MF, Praca F, Gomes L, Marino E, Demoly P. Self-reported drug allergy in a general adult Por-tuguese population. Clin Exp Allergy. 2004;34:1597-601. 14. Divac N, Stevanović G, Pelemiš M, Prostran M. Antibiotic
consumption in Serbia during 2000-2006 period. Antimi-crob Agents. 2009;34 Suppl 2:S53.
15. Weiss ME, Adkinson NF. Immediate hypersensitivity re-actions to penicillin and related antibiotics. Clin Allergy. 1988;18:515-40.
16. McMahon AD, Evans JM, MacDonald TM. Hypersensitiv-ity reactions associated with exposure to naproxen and ibu-profen: a cohort study. J Clin Epidemiol. 2001;54:1271-4. 17. Namazy JA, Simon RA. Sensitivity to non-steroidal
an-ti-inflammatory drugs. Ann Allergy Asthma Immunol. 2002;89:542-50.
18. Ramanuja S, Breall JA, Kalaria VG. Approach to „aspirin al-lergy“ in cardiovascular patients. Circulation. 2004;110:e1-4. 19. Brown AF, McKinnon D, Chu K. Emergency department
anaphylaxis: a review of 142 patients in a single year. J Allergy Clin Immunol. 2001;108:861-6.
20. Hung OR, Bands C, Laney G, Drover D, Stevens S, Mac-Sween M. Drug allergies in the surgical population. Can J Anaesth.1994;41:1149-55.
21. Chen W, Mempel M, Schober W, Behrendt H, Ring J. Gen-der difference, sex hormones and immediate type hypersensi-tivity reactions. Allergy. 2008;63(11):1418-27.
22. Zilinskaite L, Tamasauskas D, Kvedariene V, Sitkauskiene B. Self-reported drug allergy in health care workers in conserva-tive and surgical medicine departments. J Investig Allergol Clin Immunol. 2012;22(5):357-62.
23. Brown SGA. Clinical features and severity grading of ana-phylaxis. J Allergy Clin Immunol. 2004;114:371-6.
24. Sanchez-Borges M, Ivancevich JC, Rodriguez-Perez N, Ansotegui J. Evidence based approaches to diagnosis and
management. In: Pawankar R, Canonica GW, Holgate ST, Lockey RF, Blaiss MS, editors. WAO White Book on Al-lergy. Milwaukee: WAO; 2013. p. 109-13.
25. Kelava N, Lugović-Mihić L, Duvančić T, Romić R, Šitum M. Oral allergy syndrome – the need of a multidisciplinary approach. Acta Clin Croat. 2014;53:210-9.
26. Tamayo E, Alvarez FJ, Castrodeza J, Yanez J, Arnaiz P, Lajo C, et al. Self-reported drug allergies and the diagnostic work-up in the surgical population. J Eval Clin Pract. 2010;16 (5):902-4.
27. Bavbek S, Erkekal FO, Celik GE, Gőnűllű I, Misirligil Z. Self-reported prevalence of hypersensitivity reactions against drugs among medical students: does awareness cause any dif-ference? Pharmacoepidemiol Drug Saf. 2011;20(2):154-61. 28. Medicine and Medical Devices Agency of Serbia [Internet].
Belgrade: ALIMS; c2005-2015 [cited 2015 Jan 18].
An-Sažetak
SAMOPRIJAVLJENE ALERGIJE NA LIJEKOVE KOD KIRURŠKIH BOLESNIKA U SRBIJI
J. Veličković, I. Palibrk, B. Miljković, D. Veličković, B. Jovanović, V. Bumbaširević, M. Djukanović i V. Šljukić
Podatak o alergiji na lijekove je od velikog značenja u perioperacijskom razdoblju, a medicinska dokumentacija obično ne sadrži dokumente koji potvrđuju prijavljenu alergiju. Cilj ovoga istraživanja bio je ispitati učestalost i značajke samo-prijavljenih alergija na lijekove od strane odraslih kirurških bolesnika u Srbiji i analizirati utjecaj takvog anamnestičkog podatka na propisivanje lijekova u perioperacijskom razdoblju. Studija je obuhvatila bolesnike podvrgnute elektivnim kirurškim intervencijama iz područja opće kirurgije tijekom jednogodišnjeg razdoblja u tercijarnoj zdravstvenoj ustanovi. Oni su ispitivani primjenom strukturiranog upitnika o postojanju alergija i njihovoj naravi. Medicinska dokumentacija je pregledana nakon otpusta iz bolnice kako bi se ispitalo propisivanje lijekova tijekom hospitalizacije. Od 1126 bolesnika evaluiranih tijekom studije, 434 (38,5%) ih je prijavilo ukupno 635 reakcija na lijekove. Najčešće samoprijavljene alergijske reakcije su bile na antibiotike (68%), nesteroidne protuupalne lijekove (16,4%) i jodni kontrast (3,9%). Samoprijavljivanje alergija je bilo češće kod žena, stanovnika urbanih područja i korisnika biljnih lijekova. Većinu prijavljenih reakcija su činile kožne (72%) i respiracijske (34%), dok je anafilaksu prijavilo 3,2% bolesnika. Samo 38 (8,7%) bolesnika je nakon reakcije podvrgnuto nekom alergološkom testiranju. Pregled povijesti bolesti je pokazao da je 26 (6%) bolesnika tijekom hospitalizacije primilo lijek na koji su prijavili alergijsku reakciju u prošlosti, što nije bilo praćeno neželjenim učincima. Samoprijavljivanje alergija na lijekove je veoma često kod kirurških bolesnika u Srbiji, što je u suprotnosti s niskom stopom ispitanih i dokumentiranih alergija. Kako se bolesnicima ne bi uskratila učinkovita terapija ili odlagala operacija, zdrav-stveni radnici bi trebali više pozornosti posvetiti preciznoj klasifikaciji neželjenih reakcija na lijekove.
Ključne riječi: Alergija na lijekove; Alergija; Lijekovi, popratni učinci i štetna djelovanja; Ankete i upitnici; Kirurški odjel, bolnički; Srbija
nual report of spontaneous adverse drug reaction reporting in 2011. [about 2 screens]. Available from: www.alims.gov.rs/ eng/pharmacovigilance/annual-reports/
29. De Hert S, Imberger G, Carlisle J, Diemunch P, Fritsch G, Moppett J, et al. Task Force on preoperative evaluation of the adult noncardiac surgery patient of the European Soci-ety of Anaesthesiology. Preoperative evaluation of the adult patient undergoing non-cardiac surgery: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol. 2011;28:684-722.
30. Khalil H, Leversha A, Khalil V. Drug allergy documentation – time for a change? Int J Clin Pharm. 2011;33:610-3. 31. Frigas E, Park MA, Narr BJ, Wolcheck GW, Danielson DR,
Markus PJ, et al. Preoperative evaluation of patients with his-tory of allergy to penicillin: comparison of 2 models in prac-tice. Mayo Clin Proc. 2008;83(6):651-7.