Evaluation Use of Totally Implantable Vascular Access Port for Chemotherapy
During Five Years in Sanglah General Hospital-Denpasar
Wayan Wahyu Sutrisna1, Gede Budhi Setiawan, IBM Surya Wisesa, Putu Anda Tusta Adiputra.2
1
General surgery resident, Udayana Medical Faculty/Sanglah General Hospital Denpasar,Indonesia 2
Surgical Oncology Consultant, Subdivision of Surgical Oncology, Udayana Medical Faculty/ Sanglah General Hospital Denpasar,Indonesia
Abstract
Background: Chemotherapy is generally administered intravenously, which poses a risk of extravasation. Administration of chemotherapy through central venous access with Totally Implantable Vascular Access Port (TIVAP) or known as the chemo port implantation in Bali are uncommon. The purpose of this retrospective descriptive study to evaluate the results of the implantation of chemo port that we did during the year 2011-2015 in Sanglah General Hospital Denpasar.
Method :This study is a retrospective descriptive study of all patients implanted TIVAP over the years 2011- 2015 in Sanglah General Hospital Denpasar.
Result :The total patients admisterated for TIVAP for five year is 70 patient and mostly women (78,5%). Breast carcinoma is the most cases 48 patient (68,5%). The difficulty peripheral venous access is the most indications to do impalantation 46 patients (65,5%) and type vesicant chemotherapy is the second 24 patient (34,2%). Area location where implantation located mostly in the upper chest 63 patient (90%) and operation techniques most used is the percutaneous access to the right internal jugular vein 30 patients (42,8%).
Conclusion: Totally Implantable Vascular Access Port (TIVAP) for chemotherapy at present are a safe enough, means for the administration of chemotherapy regiment or other substances, in view of the low number of complications observed in this study.
7
Background
Majority Chemotherapy regiment were administered intravenously, which had a risk of extravasation. Despite the incidence are rare, but it can cause risk serious tissue damage, especially certain the type of vesicant. Vesicant chemotherapy administration through central venous access is a standard of care in developed countries. Administration of chemotherapy through central venous access with Totally Implantable Vascular Access or better known as the chemo port implantation in Indonesia, especially in Bali are uncommon. The purpose of this retrospective descriptive study to evaluate the results of the implantation of chemo port that we did during the year 2011-2015 in Sanglah General Hospital Denpasar. The use of Totally Implantable Venous Access Devices (TIVAPs) had made changed the way of care and quality of life for cancer patients underwent treated with chemotherapy. TIVAPs represent a confort situation when long-term venous access is needed, especially for administration of cytotoxic medications or intravenous targeted agents in cancer patients over a long period of time [1]. The current controvesies regarding TIVAP application in clinical practice includes the insersion site (internal, external jugular and subclavian vein) and the insertion technique (open, percutaneous or with ultrasound guidance). Many expert suggesting Cephalic vein approach has the advantage of safety and low incidence of early complications but it is affected by a high rate of failure[2]. Subclavian vein approach are located in an easy accessible area but they are affected by a relatively high risk of thrombosis, vein stenosis, catheter fatigue and they have the highest risk of pneumothorax at insertion [3].
The internal jugular approach is the preferred for tunnelled infusion catheter with the lowest incidence of venous thrombosis [4]. Usually percutaneus techniques through the Seldinger technique are preferred [5-7] but in some cases surgeons prefer the open approach in the cephalic or subclavian vein. Early complications include: pneumothorax, hemothorax, air embolism, accidental arterial puncture, cardiac arrhythmia, pericardial tamponade and brachial plexus injury [6,7]. Delay complications include: bloodstream infection, thrombosis, catheter dysfunction, rupture, migration or embolisation, “pinch-off” syndrome, superior vein cava erosion and perforation, extravasation, pocket infection and port inversion [8].
The improvement of the technique and the implanted devices led to a decreased rate of potential life threatening complications. The aim of this study was to evaluate the results of the implantation of chemo port that we did during the year 2011-2015 in Sanglah General Hospital Denpasar.
Method
This study is a retrospective descriptive study of all patients implanted TIVAP over the years 2011- 2015 in Sanglah Hospital Denpasar. Patient distribution recorded and divided according to gender, diangnosis, port location, implantation procedure, indication, and certain complications. Routine as a standart preoperative evaluation included medical history and physical examination, focusing on possible anatomic pitfalls (cervical or mediastinal adenopathy, chest wall tumours, previous neck or thoracic surgery), body habitus, previous vascular access placements and complications. Laboratory consisted in full blood count and haemostat functions. Several condition were not allowed for TIVAP placement are platelet count < 80.000/mm3, INR > 1.5, neutrophil count <1000/mm, fever or sepsis.
Implantation techniques.
Devices were implanted in the operating room, using maximal sterile linen-drapping, under local anaesthesia, administering Lidocaine 1%. If necessary, giving premedication with midazolam 0.01-0.035 mg/kg (1–3 mg) in case of patient anxiety. A profilactic antibiotic given as single dose of Cefazoline 2 g was administered intravenously before the procedure. In order to prevent clot formation and catheter blockage, TIVAP were flushed with 20 ml heparinized saline solution concerntration of 50 U/ml heparin with 100 ml saline. Standard protocol was to flush all the devices with heparinized saline solution after use and on a monthly outpatient basis. There were three different techniques were used for implantation, devices were placed using either a cephalic vein cut-down or a blind percutaneous approach based on anatomic landmarks. The choice of insertion technique was at the discretion of the surgeon[1,2].
8
A single incision was made in the upper anterior chest wall along the delto-pectoral groove as first described by Heimbach and Ivey [3]. The cephalic vein was identified and isolated between 2 vessel loops. The catheter was then directly inserted into the cephalic vein through a transverse venotomy. The distal cephalic vein was tied off. The reservoir was inserted superficially into a subcutaneous pocket, with the device located just inferior to the skin incision. Additional postoperative radiographs were performed to confirm positioning of the tip of the catheter at the cavo-atrial junction.
“Blind” percutaneous technique.
The preferred access site was the subclavian vein (SV). The internal jugular vein (IJV) was chosen when SV cannulation was contraindicated for anatomic pitfalls. A Seldinger technique was used to access the vein with dilators and peel away sheaths for the insertion. In case of subclavian vein cannulation, the site of puncture was at the inferior border of the clavicle, between the middle and the lateral third of it, directed toward the fingertip pressed firmly into the suprasternal notch. The needle passed beneath the inferior margin of the clavicle in a horizontal plane and directed toward the anterior margin of the trachea at the level of the suprasternal notch (4). The internal jugular vein was cannulated at the top of the triangle between the sternal and clavicular head of the sternocleidomastoid muscle, advancing the needle through the skin at a 45° angle in the direction of the omolateral nipple. Usually 2 incisions were necessary: a small incision at the catheter exit site from the skin and a second larger incision for location of the implantable access device. A subcutaneous tunnel was made to pass the catheter from 1 incision to the other. Post operative radiograph to confirmed the position of the catheter at the cavo-atrial junction and for the presence of complication such as pneumothorax(6).
Result
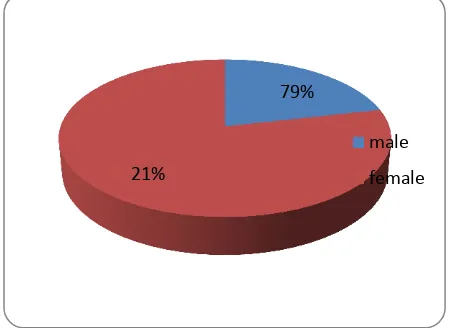
The total patients admisterated for TIVAP for five year is 70 patient and mostly female (78,5%), and male 21 % .
Table 1. Distribution of patients gender administrated TIVAP 2011-2015
Gender
n
%
Male
15
21
Female
55
79
Distribution of patients gender administrated TIVAP 2011-2015
Indication for TIVAP as well knows were ; Chemotherapy, Antiviral therapy, Parenteral nutrition, Blood tranfusion/sample, and Pain management/paliative(epidural), but recently in Bali the most favourable indication were difficulty peripheral venous access and the second indication was type of vesicant chemotherapy. This related to goverment regulation of national public insurance. The difficulty pheriperal
79%
21%
male
9
vanous accces is the most indications to do impalantation 46 patients (65,5%) and type vesicant chemotherapy is the second 24 patient (34,2%).
Table 2. Patient distribution according to indication of TIVAP
Indication
N
%
Difficult pheriperal
vanous acces
46
66%
Vesicant
24
34%
Patient distribution according to indication of TIVAP
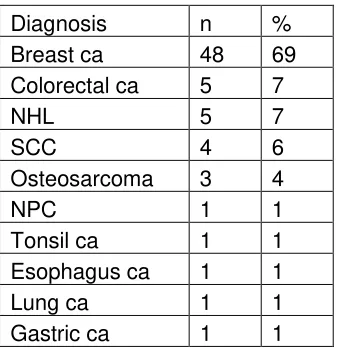
Breast carcinoma was the major case of malignancy were administrated TIVAP Breast carcinoma. Total breast carcinoma patient administrated TIVAP during 2011-2015, 48 patient (69%), followed by colorectal carcinoma, NHL , and sarcoma patient.
Table 3. Patient distribution according to diagnosis
Diagnosis
n
%
Breast ca
48
69
Colorectal ca
5
7
NHL
5
7
SCC
4
6
Osteosarcoma
3
4
NPC
1
1
Tonsil ca
1
1
Esophagus ca
1
1
Lung ca
1
1
Gastric ca
1
1
Patient distribution according to diagnosis
66% 34
difficulty pheriperal venous acces
10
Area location where implantation located mostly in the upper chest 63 patient (90%) and left upper chest 7 patient (10%).
Table 4. Area implantation located
Port location
n
%
Right upper chest
63
90
Left upper chest
7
10
Area implantation located
69%
7% 7%
6% 4%
breast ca
colorectal ca
NHL
scc
90% 10%
Chart Title
right upper chest
11
TIVAP was implanted into the contralateral side to avoid the radiotherapy area
Operation techniques most used is the percutaneous access to the right internal jugular vein 30 patients (43%), right subclavian vein 23 patient (33%), right cephalica 10 patient (14%), left subclavian 4 patient (6%) and left cephalica 3 patient (4%).
Table 5. Patient distribution according to surgical approach.
Approach
n
%
Right subclavian vein
23
33%
Right internal jugular vein
30
43%
Right cephalika vein
10
14%
Left subclavian vein
4
6%
12
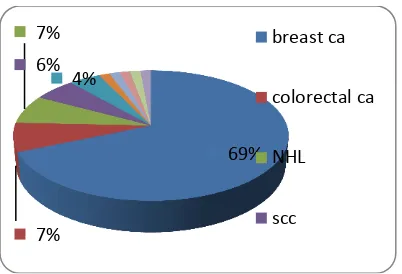
TIVAP implantation procedure. US-guided IJV (V) surgical procedure (A, B). Lines were drawn to create the anatomical landmark, surgical incision, and puncture site (C). Insertion of a continuous infusion needle (D).
33% 43%
14% 6%
4%
right subclavian vein
right internal jugular vein
right cephalika vein
13
Catheter tip and port location. X-ray examination for catheter tip location (A). CT showing location of port and catheter (B).
Certain complication of TIVAP insertion in view number are 8 patient (11%), there were blocking , infections, and disconected.
Table 6. TIVAP Complication
Complication
n
%
Blocking
3
4
Infections
3
4
Disconnected
2
3
TIVAP Complication
n; blocking;
3; 37%
n; infection s; 3; 38% n;
disconec ted; 2;
25% blocking
infections
14
Complications of hematoma (A) and infection (B).Discussion
The totally implantable vascular access port (TIVAP) system was first performed by Dr. Niederhuber in 1982. The main purpose of a TIVAP in clinical practice is to provide a secure and comfortable route for cytotoxic drugs for patients with malignancies and intravenous parenteral nutrition solutions [1,7]. In this study, we evaluated the consequences of using a TIVAP in cancer patients, since 5 years there were a few cases on the use of a TIVAP in Bali regarding the US-guided implantation approach through the Cephalica vein, SCV, and IJV [5].
The IJV is located at the apex of the triangle formed by the heads of the sternocleidomastoid muscle and the clavicle. The subclavian vein crosses under the clavicle just medial to the midclavicular point [8]. These veins are invisible on the skin surface, and were therefore originally blindly punctured based on the operator’s experience. Image guidance can improve the accuracy of vascular puncture and virtually eliminates the risk of several complications reported with unguided placement such as pneumothorax, hemothorax, and nerve injury [9].
None of these complications occurred in patients who underwent US-guided placement. Under US visualization, the introducer needle is guided through the skin and into the vein. The IJV is difficult in obese patients and therefore conversion to the subclavian venous vein for TIVAP implantation is indispensable. In our department, all TIVAPs were implanted via the IJV or subclavian vein successfully. After implantation, chemotherapy and/or fluid administration were performed on the same day. Hematoma, blocking, and port disconnected are the most common mechanical complications during the insertion of central venous catheters. These three complications were observed in 8 (11%) patients, which is lower than in previous studies [5, 8,10].
15
The distance between the left IJV or the left subclavian vein to the junction of the right atrium and SVC is greater than on the right side. The catheter length inserted into the body from the left side is longer than that from the right, which may cause more complications. However, in our study, the difference between the complications of right and left sides was not significant.
The timing of TIVAP use is controversial. Nuriye et al. reported that chemotherapy administration immediately after a venous port catheter implantation appears safe without increased acute and chronic complications in an inpatient setting [11]. However, Narducci et al. found that a minimal interval of 8 days between placement of the TIVAP and its first use can reduce complications [11]. In our study, the overall complication rate of 11% was similar to the 10 to 20% complication rate reported for several large surgical series in which both chest and arm ports were placed [10]. Our results support clinical administration of TIVAP on the implantation day.
Conclusion
Totally Implantable Vascular Access Port (TIVAP) for chemotherapy at present are a safe enough, means for the administration of chemotherapy regiment or other substances, in view of the low number of complications observed in this study..
References
1. Vescia S, Baumgärtner AK, Jacobs VR, Kiechle-Bahat M, Rody A, Loibl S, Harbeck N: Management of venous port systems in oncology: a reviewnof current evidence. Ann Oncol 2008, 19:9–15.
2. Biffi R, Pozzi S, Agazzi A, Pace U, Floridi A, Cenciarelli S, Peveri V, Cocquio A, Andreoni B, Martinelli G: Use of totally implantable central venous access ports for high-dose chemotherapy and peripheral blood stem cell transplantation: results of a monocentre series of 376 patients. Ann Oncol 2004, 15:296–300.
3. Goldhirsch A, Wood WC, Gelber RD, Coates AS, Thürlimann B, Senn H-J: Meeting highlights: updated international expert consensus on the primary therapy of early breast cancer. J Clin Oncol 2003, 21:3357–3365.
4. Kreis H, Loehberg CR, Lux MP, Ackermann S, Lang W, Beckmann MW, Fasching PA: Patients’ attitudes to totally implantable venous access port systems for gynecological or breast malignancies. Eur J Surg Oncol 2007, 33:39–43.
5. Sonobe M, Chen F, Fujinaga T, Sato K, Shoji T, Sakai H, Miyahara R, Bando T, Okubo K, Hirata T, Date H: Use of totally implantable central venous access port via the basilic vein in patients with thoracic malignancies. Int J Clin Oncol 2009, 14:208–212.
6. Kurul S, Saip P, Aydin T: Totally implantable venous-access ports: local problems and extravasation injury. Lancet Oncol 2002, 3:684–692.
7. Lin Y-C, Chu C-H, Ou K-W, Chan D-C, Hsieh C-B, Chen T-W, Hsu H-M, Yu J-C: Use of a totally implantable access port through the external jugular vein when the cephalic vein approach is not feasible. Ann Vasc Surg 2011, 25:217–221.
8. McGee DC, Gould MK: Preventing complications of central venous catheterization. N Engl J Med 2003, 348:1123–1133.
9. Kusminsky RE: Complications of central venous catheterization. J Am Coll Surg 2007, 204:681– 696.
10. Barbetakis N, Asteriou C, Kleontas A, Tsilikas C: Totally implantable central venous access ports. Analysis of 700 cases. J Surg Oncol 2011, 104:654–656.