Attention-Deficit Disorder and Conduct Disorder in
Girls: Evidence for a Familial Subtype
Stephen V. Faraone, Joseph Biederman, and Michael C. Monuteaux
Background: The frequent comorbidity between atten-tion-deficit/hyperactivity disorder (ADHD) and conduct disorder (CD) raises the possibility that ADHD1CD is a distinct and separate condition.
Methods:We tested hypotheses about patterns of familial association between ADHD, CD, oppositional defiant disorder (ODD) and adult antisocial personality disorder (ASPD). Using family study methodology in a sample of girls, we found 11 children with diagnoses of ADHD1CD, 39 with ADHD1ODD, and 90 with ADHD only. These were compared with 122 non-ADHD, non-CD control probands. Familial risk analysis was utilized.
Results:Relatives of each ADHD proband subgroup were at significantly greater risk for ADHD, and the relatives of ADHD-only subjects were at a greater risk of ODD than relatives of control subjects. Also, rates of CD were elevated among relatives of ADHD1CD probands only, and the coaggregation of ADHD and the antisocial disor-ders could not be accounted for by marriages between ADHD and antisocial spouses. Both ADHD and antisocial disorders occurred in the same relatives more often than expected by chance.
Conclusions:These findings suggest that ADHD with and without antisocial disorders may be etiologically distinct disorders and provide evidence for the nosologic validity of ICD-10 hyperkinetic conduct disorder. Biol Psychia-try 2000;48:21–29 © 2000 Society of Biological Psychiatry
Key Words:ADHD, conduct disorder, oppositional defi-ant disorder, family– genetic, risk factors
Introduction
A
n obstacle to the successful classification of attention-deficit/hyperactivity disorder (ADHD) is the fre-quently reported comorbidity between ADHD and conductdisorder (CD; Caron and Rutter 1991). This overlap has been consistently found in clinical samples in studies of children with ADHD and children with CD (Biederman et al 1987, 1991c; Hinshaw 1987; Loeber et al 1990; Milich et al 1987; Schachar and Tannock 1995) and in follow-up studies of ADHD children (Gittelman et al 1985). Taylor (1994) noted that the comorbidity between ADHD and CD raises a key nosologic question: Are these two disorders best seen as co-occurring yet separate entities or, does their consistent co-occurrence signal the presence of a separate category of disorder? The former approach was taken by the American DSM-IV (American Psychiatric Association 1994), whereas the latter has been recognized with the separate category of hyperkinetic conduct disor-der used by the World Health Organization’s ICD-10 (World Health Organization 1988). The differences be-tween the two systems underscore the need for further nosologic research.
As discussed in detail by Caron and Rutter (1991), comorbidity can occur for many reasons. It can be an artifact in clinical samples, because people with multiple disorders are more likely to seek help than those with only one disorder. In epidemiologic studies, screening tests can exaggerate comorbidity, because comorbid disorders are more likely to exceed the test’s threshold for detection. Comorbidity may also signal errors in the nosology used to define the disorders. If two disorders are actually the extremes of dimensional traits, then the choice of the threshold for defining the disorders will influence the degree of observed comorbidity. Also, overlapping diag-nostic criteria can lead to spurious comorbidity. Our empirical study of this latter issue, however, suggests that this effect cannot account for most comorbidity in ADHD (Milberger et al 1995). Comorbidity might also indicate that a nosologic subdivision of syndromes is not appropri-ate or that one disorder is an early manifestation or a component of the other.
Elsewhere, we have argued that methods from genetic epidemiology can clarify the etiologic relationships among comorbid disorders (Biederman et al 1990b, 1991a, 1991b; Faraone et al 1991a, 1991b). In previous work, we first showed that the familial coaggregation of DSM-III-defined attention deficit disorder (ADD) and CD was consistent with the ICD-10 formulation of
From Pediatric Psychopharmacology Unit, Psychiatry Service, Massachusetts General Hospital (SVF, JB, MCM), the Department of Psychiatry, Harvard Medical School (SVF, JB), Harvard Institute of Psychiatric Epidemiology and Genetics, Department of Psychiatry, Harvard Medical School at Brockton– West Roxbury Veterans Affairs Medical Center and Massachusetts Mental Health Center (SVF), and the Department of Epidemiology, Harvard School of Public Health (MCM), Boston, Massachusetts.
Address reprint requests to Stephen V. Faraone, Ph.D., Harvard Medical School, Pediatric Psychopharmacology Unit (ACC 725), Massachusetts General Hos-pital, Fruit Street, Boston MA 02114.
Received April 7, 1999; revised December 17, 1999; accepted December 22, 1999.
hyperkinetic conduct disorder (Faraone et al 1991b). We then replicated that result in an entirely different sample of children using DSM-III-R criteria (Faraone et al 1995, 1997, 1998).
Data from other groups also favored a familial distinc-tion between ADHD with CD (ADHD1CD) and other ADHD children. Stewart et al (1980) found alcoholic or antisocial disorders to be more frequent among fathers of unsocialized, aggressive, hyperactive boys compared with fathers of boys who were only hyperactive. Lahey et al (1988) reported higher rates of antisocial disorders, de-pression, and substance abuse among relatives of ADHD1CD probands compared to other ADHD pro-bands. In another study, the mothers of ADHD1CD children were found to have higher rates of psychopathol-ogy than the mothers of ADHD children (Lahey et al 1989). In a study by Frick et al (1991), parents of ADHD1CD children had higher rates of childhood hy-peractivity, CD, and substance use than parents of ADHD children. August and Stewart (1983) reported that, among hyperactive children, a family history of hyperactivity predicted more symptoms of CD in the child and a greater risk of CD to siblings.
Notably, Szatmari et al (1993) confirmed the familial coaggregation of ADHD and CD in a population based, epidemiologic, family study, as did Silberg et al (1996) in a population-based twin study. The twin study found that the genes influencing variation in hyperactivity scores were also responsible for variation in conduct problems. Between 76% and 88% of the correlation between hyper-activity and conduct scores were attributed to genes. It further concluded that the results were consistent with the existence of a biologically based group of children who manifest both hyperactivity and conduct disturbances. Further evidence that the ADHD1CD subgroup may be etiologically meaningful comes from a study showing differences in serotonergic functioning between aggres-sive and nonaggresaggres-sive ADHD children (Halperin et al 1994).
Overall, these data suggest that, from a familial perspec-tive, ADHD children with CD may be etiologically dis-tinct from those without CD. Although persuasive, these prior studies have examined predominantly male samples. Thus, we do not know if prior finds generalize to female ADHD patients. We cannot assume generalizability, given that CD is known to have gender-specific features in ADHD children. Notably, a meta-analysis by Gaub and Carlson (1997) suggested that, compared with boys, girls with ADHD tend to have lower rates of conduct disorder. We recently confirmed that in a large case-control study of girls (Biederman et al 1999).
The main hypothesis of this report posits ADHD1CD to be a distinct familial subtype (i.e., an entirely separate
condition from ADHD without CD as regards familial risk factors). This hypothesis predicts high rates of ADHD in relatives of both ADHD1CD and ADHD without CD children, but that CD should be increased only among relatives of ADHD1CD children. It also predicts that ADHD and CD should cosegregate among the relatives of ADHD1CD children (i.e., among relatives of children with ADHD1CD, the presence of one disorder should predict the other; cases of ADHD without CD and CD without ADHD should be rare).
We focus on this main hypothesis because it has been supported in our prior studies of ADHD and CD among families ascertained through boy probands (Faraone et al 1991b, 1995, 1997, 1998). Our prior studies also ruled out alternative hypotheses that must be considered in genetic epidemiologic studies (Faraone et al 1999; Faraone and Tsuang 1995; Pauls et al 1986a, 1986b; Reich et al 1972, 1979). Thus, we also sought to see if the alternative hypotheses could be ruled out in our sample of girl probands.
Alternative hypothesis one posits that ADHD and CD are etiologically independent but co-occur because of nonrandom mating. This explains comorbidity by assum-ing that the spouses of ADHD individuals have higher rates of CD than spouses of non-ADHD individuals. If that were true, then children of ADHD parents would be at increased risk for CD. This hypothesis differs from our main hypothesis, because it predicts that ADHD and CD should not cosegregate among the relatives of ADHD1CD probands and that there should be an associ-ation between ADHD diagnoses in one parent and CD diagnoses in the other parent.
Additional alternative hypotheses assume that the famil-ial transmission of ADHD and CD follows a multifactorfamil-ial polygenic (MFP) model. The MFP model assumes that both disorders arise from the same pool of familially transmissible etiologic factors (e.g., genes, familial adver-sity; Faraone et al 1999). Alternative hypothesis two states that ADHD1CD requires more familially transmissible etiologic factors (e.g., genes, familial adversity) for its expression compared with ADHD without CD. It predicts that relatives of ADHD1CD probands will have higher rates of ADHD and higher rates of CD (Faraone et al 1999). This would be consistent with the idea that ADHD1CD is a severe form of ADHD. For example, if a polygenic system (or a series of adverse familial environ-mental events) causes these disorders, then alternative hypothesis two would predict that the number of genes (or familial adverse events) required to express ADHD1CD is greater than the number required to express other cases of ADHD.
without CD share common familial etiologic factors; but, in contrast to alternative hypothesis two, alternative hypothesis three assumes that the two groups differ because of nonfamilial environmental effects. This predicts similar rates of ADHD and CD among the relatives of ADHD1CD and other ADHD probands. For example, if a polygenic system (or a series of adverse familial environmental events) causes these disorders, then an equal risk to relatives across sub-groups would suggest that the number of genes (or familial adverse events) required for each subgroup is the same. If that is so, then differences between groups must be owing to nonfamilial causes.
The primary goal of this report is to test our main hypothesis and the alternatives listed above. Also, any examination of the association between ADHD and CD must also consider that some ADHD children have oppo-sitional defiant disorder (ODD) but not CD. Lahey et al’s review of longitudinal studies showed that ODD is a heterogeneous condition (Lahey et al 1994). Some ODD children progress to CD, but others do not (Loeber and Keenan 1994). For example, our follow-up study de-scribed two subtypes of ODD associated with ADHD— one that is prodromal to CD and another that was not likely to progress into CD in later years (Biederman et al 1996). These ODD subtypes had different correlates, course, and outcome.
Our prior family studies of the association between ADHD, CD, and ODD provided ambiguous evidence for the status of ADHD1ODD boys who did not have CD (Faraone et al 1991b,1997). Our family study of boys with DSM-III ADD showed that the relatives of ADD1ODD probands were at a higher risk for ADD and for one or more antisocial disorders than the relatives of ADD probands but at a lower risk than the relatives of ADD1CD probands (Faraone et al 1991b). This suggested that the ADHD1ODD boys were, in terms of familial risk, intermediate between ADHD-only and ADHD1CD boys. In contrast, our larger study of DSM-III-R ADHD boys showed that as regards the prevalence of ADHD, CD, and ODD among relatives, the ADHD1ODD boys were more similar to the ADHD-only boys than the ADHD1CD boys (Faraone et al 1997). These data suggested that ADHD1ODD children who did not onset with CD before adolescence were nosologically different from those who develop CD.
Given these uncertainties about the nosological status of ADHD children who have ODD but not CD, in this report we stratified our ADHD sample into three groups: ADHD1CD, ADHD1ODD, and ADHD only. This al-lowed for comparisons among relative groups that would determine if, from a familial perspective, ADHD1ODD was more similar to ADHD1CD or ADHD only.
Methods and Materials
Subjects
An overview of this sample has been previously published (Biederman et al 1999). Female children and adolescents 6 –18 years of age were eligible for the study. We studied two groups of index girls: 140 ADHD probands and 122 non-ADHD comparisons. These groups had 417 and 369 first degree biolog-ical relatives, respectively. No ethnic or racial groups were excluded from the study. Potential girl probands were excluded if they had been adopted, or if their nuclear family was not available for study. We excluded girls if they had major senso-rimotor handicaps (paralysis, deafness, blindness), psychosis, autism, inadequate command of the English language, or a Full Scale IQ less than 80. All of the ADHD girls met full DSM-III-R diagnostic criteria for ADHD at the time of the clinical referral; at the time of recruitment they all had active symptoms of the disorder. All subjects older than 12 gave written informed consent for participation. Parents gave written informed consent for participation of children under 12, and these children partic-ipated only if they assented to the study procedures.
We identified psychiatrically referred females from lists of consecutive ADHD patients from the pediatric psychopharma-cology clinic at the Massachusetts General Hospital (MGH). Pediatrically referred ADHD females were identified from lists of children having evidence of ADHD in the computerized medical record of a health maintenance organization (HMO). Within each setting, we selected normal control subjects from lists of outpatients at pediatric medical clinics.
Procedures
Because this study had begun prior to the finalization of DSM-IV criteria for ADHD, we used DSM-III-R– based structured inter-views to ascertain and diagnose subjects but supplemented our interviews with questions that would allow us to make DSM-IV diagnoses. Psychiatric assessments of probands and their siblings were made with the Kiddie Schedule for Affective Disorders and Schizophrenia (epidemiologic version [Kiddie-SADS-E]; Orvas-chel 1985). Diagnoses were based on independent interviews with the mothers and direct interviews with the child. Children younger than 12 years of age were not interviewed directly. Diagnostic assessments of parents were based on direct inter-views with each parent using the Structured Clinical Interview for DSM-III-R (SCID; Spitzer et al 1990). To assess childhood diagnoses in the parents, we administered an addition to the SCID, consisting of unmodified modules from the Kiddie-SADS-E covering childhood DSM-III-R diagnoses.
parents signed a written consent form for participation in the study.
Interviews were conducted by raters with undergraduate de-grees in psychology who had been trained to high levels of inter-rater reliability. The training consisted of familiarization with psychiatric nosology and the structured interviews. Raters-in-training first observed interviews carried out by experienced raters and clinicians. Raters were supervised by the principal investigator (JB). Kappa coefficients of agreement were com-puted between raters and three experienced psychiatrists, each board certified in both child and adult psychiatry, who listened to audiotaped interviews made by the raters. Based on 173 inter-views, the mediankwas 0.86. Theks were 0.99 for ADHD, 0.93 for conduct disorder, 0.80 for multiple anxiety disorders, 0.83 for major depression, and 0.94 for bipolar disorder.
A committee of three psychiatrists, each board certified in both child and adult psychiatry, chaired by the principal investigator (JB) resolved all diagnostic uncertainties. The committee mem-bers were blind to the subjects’ ascertainment group, ascertain-ment site, all data collected from other family members, and all nondiagnostic data (e.g., psychological tests). Diagnoses were considered positive if, based on the interview results, DSM-III-R criteria were unequivocally met to a clinically meaningful degree. As suggested by others (Gershon et al 1982), we diagnosed major depression only if the depressive episode was associated with marked impairment. Because the anxiety disor-ders comprise many syndromes with a wide range of severity, we used two or more anxiety disorders as a useful summary variable. For children older than 12, data from direct and indirect inter-views were combined by considering a diagnostic criterion positive if it was endorsed in either interview.
In addition to psychiatric data, we assessed socioeconomic status (SES), with the Hollingshead–Redlich scale (Hollingshead 1975) and family intactness (divorce or separation of parents in family of origin).
Our analyses of sibling data avoided the statistical problems associated with correlated family data by using Huber’s (1967) formula as implemented in STATA (Stata Corporation 1992).
The formula is a “theoretical bootstrap” that produces robust statistical tests for both linear and logistic regression. To reduce the Type I error rate, all statistical tests were two tailed; we used the .01 level of statistical significance. Differences that were significant at the .05 level are discussed as marginally significant trends.
Results
Sociodemographic and Clinical Characteristics
We defined a subject as having a lifetime history of illness if a disorder was reported at the time of assessment. There were 11 girls with ADHD1CD, 39 with ADHD1ODD, and 90 with ADHD only. These were compared with 122 non-ADHD, non-CD control girls. There were 10 children with comorbid CD as well as ODD. These girls were included in the ADHD1CD group.
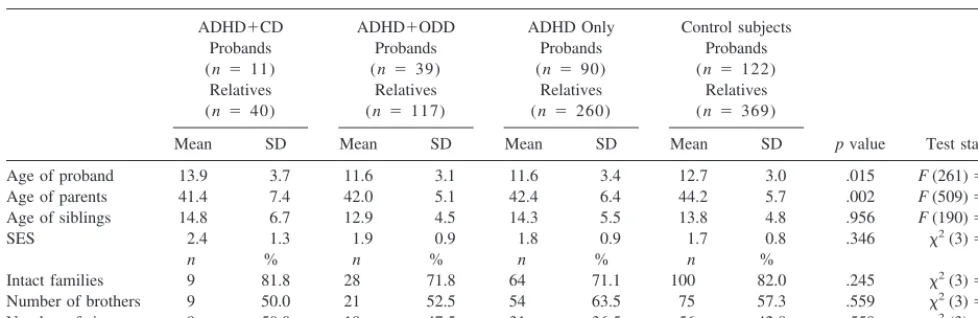
The groups did not significantly differ in age of pro-bands, age of siblings, SES, intactness of family, number of brothers or number of sisters (Table 1). There was a significant difference in the age of the parents, but pairwise comparisons between groups failed to yield any significant findings.
Familial Association between Antisocial Disorders and ADHD
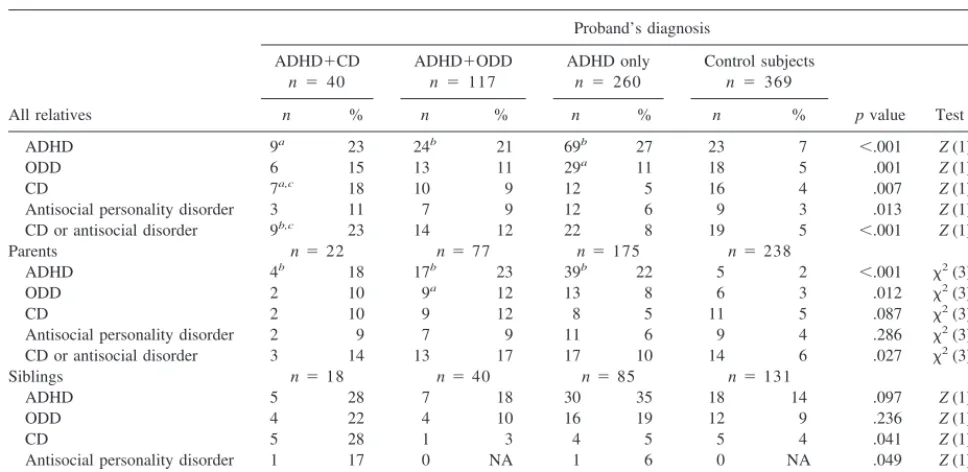
Relatives of the ADHD, ADHD1ODD, and ADHD1CD proband subgroups were at significantly greater risk for ADHD compared with relatives of controls (Table 2). Also, relatives of the ADHD subgroup were at signifi-cantly greater risk for ODD compared to control subjects. There were trends toward differences in the rates of ODD between the relatives of the ADHD1CD and ADHD1ODD subgroups and the relatives of controls, but Table 1. Demographic Characteristics of Sample at Baseline
ADHD1CD Probands (n 5 11) Relatives (n 5 40)
ADHD1ODD Probands (n 5 39)
Relatives (n5 117)
ADHD Only Probands (n 590) Relatives (n 5 260)
Control subjects Probands (n 5 122)
Relatives (n 5 369)
pvalue Test statistic
Mean SD Mean SD Mean SD Mean SD
Age of proband 13.9 3.7 11.6 3.1 11.6 3.4 12.7 3.0 .015 F(261)53.53
Age of parents 41.4 7.4 42.0 5.1 42.4 6.4 44.2 5.7 .002 F(509)54.96
Age of siblings 14.8 6.7 12.9 4.5 14.3 5.5 13.8 4.8 .956 F(190)50.00
SES 2.4 1.3 1.9 0.9 1.8 0.9 1.7 0.8 .346 x2(3)53.31
n % n % n % n %
Intact families 9 81.8 28 71.8 64 71.1 100 82.0 .245 x2(3)54.16
Number of brothers 9 50.0 21 52.5 54 63.5 75 57.3 .559 x2(3)52.07
Number of sisters 9 50.0 19 47.5 31 36.5 56 42.8 .559 x2(3)52.07
they were not significant (p 5 .021 and p 5 .013, respectively). Furthermore, compared with control sub-jects, only relatives of CD probands had increased rates of CD and the combined category CD or antisocial person-ality disorder (CD/ASPD). There was a difference in the rates of CD/ASPD between the ADD1ODD relatives and the control relatives, but it was not significant (p5.013). There were no significant differences found in the rates of ASPD alone among the relatives of the four subgroups.
The relatives of ADHD1ODD and ADHD-only pro-bands did not differ in rates of ADHD, ODD, CD, or ASPD. In contrast, relatives of ADHD1CD probands had higher rates of CD and CD/ASPD compared with the ADHD only subgroup.
As Table 2 indicates, the pattern of results observed for the entire sample was also observed when the data were analyzed separately for parents and siblings. Because of the smaller sub-samples for these latter analyses, however, some comparisons did not attain statistical significance.
Nonrandom Mating and Cosegregation of ADHD, ODD, and CD
Our finding that the increased risk for CD among relatives was limited to families of ADHD1CD probands could occur if ADHD individuals had an increased likelihood of marriage with CD individuals. Rates of CD were similar
among fathers whose spouses did and did not have ADHD [12% vs. 10%;x2(1)50.21,p5.65]. Rates of CD were higher among mothers if their spouse had ADHD (7% vs. 2%), but the difference was not statistically significant [x2(1)53.0,p5.08]. Fathers whose spouse had ADHD had lower rates of ADHD, but this difference was not significant [6% vs. 12%,x2(1)5 1.0,p5.31]. Rates of ASPD in mothers were higher in those whose spouse has ADHD (4% vs. 1%), but again this was not a statistically significant difference [x2(1)5 3.2,p5.08].
If ADHD1CD probands carried two unrelated risk factors, one for ADHD and one for CD, ADHD and CD should be independently transmitted in the families of ADHD1CD probands. That is, relatives with ADHD should be at no greater risk for CD than those without ADHD. If, however, in the families of ADHD1CD probands, the degree of comorbidity in the relatives is greater than expected by chance, we use the term “coseg-regate” to indicate that the disorders are transmitted together, not independently (Pauls et al 1986a, 1986b). That was the case in our data; there was a substantial degree of cosegregation. Among relatives of ADHD1CD probands, 56% of the relatives diagnosed as ADHD also had CD, compared to 7% of the relatives who did not have ADHD [x2(1)5 11.2,p5 .001].
Our cosegregation findings are consistent with an addi-Table 2. Oppositional Defiant Disorder (ODD) and Conduct Disorder (CD) among Relatives of Attention-Deficit/Hyperactivity Disorder (ADHD) Girl Probands
All relatives
Proband’s diagnosis
ADHD1CD
n5 40
ADHD1ODD
n 5 117
ADHD only
n 5 260
Control subjects
n 5369
pvalue Test statistic
n % n % n % n %
ADHD 9a 23 24b 21 69b 27 23 7 ,.001 Z(1)54.8
ODD 6 15 13 11 29a 11 18 5 .001 Z(1)53.3
CD 7a,c 18 10 9 12 5 16 4 .007 Z(1)52.7
Antisocial personality disorder 3 11 7 9 12 6 9 3 .013 Z(1)52.5
CD or antisocial disorder 9b,c 23 14 12 22 8 19 5 ,.001 Z(1)54.0
Parents n522 n577 n5175 n5238
ADHD 4b 18 17b 23 39b 22 5 2 ,.001 x2(3)545.8
ODD 2 10 9a 12 13 8 6 3 .012 x2(3)511.0
CD 2 10 9 12 8 5 11 5 .087 x2(3)56.6
Antisocial personality disorder 2 9 7 9 11 6 9 4 .286 x2(3)53.8
CD or antisocial disorder 3 14 13 17 17 10 14 6 .027 x2(3)59.2
Siblings n518 n540 n585 n5131
ADHD 5 28 7 18 30 35 18 14 .097 Z(1)51.7
ODD 4 22 4 10 16 19 12 9 .236 Z(1)51.2
CD 5 28 1 3 4 5 5 4 .041 Z(1)52.0
Antisocial personality disorder 1 17 0 NA 1 6 0 NA .049 Z(1)52.0
CD or antisocial disorder 6a,c,d 33 1 3 5 6 5 4 .009 Z(1)52.6
Tests on all relatives and siblings by logistic regression with Huber’s Correction for correlated data; tests on Parents byx2. NA, not applicable.
a
p#.01 vs. control subjects.
b
p#.001 vs. control subjects.
c
p#.01 vs. ADHD only.
d
tional finding: There were higher rates of CD among the nine ADHD relatives of ADHD1CD probands (56%), compared with the 93 ADHD relatives of other ADHD probands [13%;x2(1)510.7,p5.001] or the 23 ADHD relatives of control probands [9%;x2(1)58.3,p5.004].
Discussion
In a large set of families ascertained through ADHD girls, we tested competing hypotheses about patterns of familial association between DSM-III-R ADHD, CD, ODD, and ASPD. After stratifying the ADHD sample into those with CD (ADHD1CD), those with ODD (ADHD1ODD), and those with neither (ADHD), familial risk analyses revealed the following: 1) relatives of each ADHD proband sub-group were at significantly greater risk for ADHD than relatives of normal control subjects, 2) rates of CD were elevated among relatives of ADHD1CD probands only, 3) the coaggregation of ADHD and CD could not be accounted for by marriages between ADHD and antisocial spouses, and 4) both ADHD and CD occurred in the same relatives more often than expected by chance alone.
Our results support our main hypothesis, which posits that ADHD1CD is a familially distinct subtype. This hypothesis is consistent with the ICD-10 decision to retain hyperkinetic conduct disorder as a separate diagnostic category (World Health Organization 1988). Our rejection of the three alternative hypotheses generalizes the conclu-sions from our studies of ADHD boys (Faraone et al 1991b, 1995, 1997, 1998).
Because of the inferential limitations of family studies (Faraone and Tsuang 1995), we cannot determine if the familial etiology of ADHD1CD is genetic or environmen-tal. Since both genes (Faraone and Biederman 1994) and environment (Biederman et al 1995a, 1995b) have been implicated in the etiology of ADHD, further work is needed to see what role they might play in the familial transmission of comorbidity between ADHD and CD.
Notably, our results reject the alternative hypothesis, which attributes the differences between ADHD with and without CD to environmental factors not transmitted in families. This alternative incorrectly predicts equal rates of conduct disorder among the relatives of the three ADHD proband subgroups (Reich et al 1979). That is, if the familial causes of CD were the same in type and degree among ADHD subgroups, the familial risks to their relatives should not differ, but they did.
Furthermore, although these familial risks did differ, the pattern of differences rejected the idea that ADHD with and without CD share a common pool of familial etiolog-ical factors such that ADHD1CD requires more familially transmissible etiologic factors (e.g., genes, familial adver-sity) for its expression compared with ADHD alone. This
idea incorrectly predicts greater rates of ADHD among relatives of ADHD1CD probands. Although the lack of group differences in rates of ADHD could be owing to low statistical power (there were only 40 relatives in the ADHD1CD group), the actual rates were very similar (23% for relatives of ADHD1CD, 27% for relatives of ADHD only).
The low risk for CD among relatives of ADHD pro-bands without CD suggests that these propro-bands are qual-itativelydistinct from the probands with comorbid antiso-cial disorders instead of quantitatively different as assumed by the multifactorial model. That is, it may be the case that the ADHD probands without CD share no familial precursors with CD. This would further suggest that ADHD in the presence of a comorbid CD represents a distinct familial subtype of ADHD. If this is the case, ADHD and CD should cosegregate (i.e., not be indepen-dently transmitted) in the families of ADHD probands with antisocial disorders (Pauls et al 1986a, 1986b). That is exactly what we found: In the relatives of ADHD1CD probands, those with ADHD were at increased risk for CD, and this level of comorbidity was significantly greater than what was observed among the ADHD relatives of other ADHD probands.
The subsample of ADHD1ODD girls provided some intriguing results. We know from Lahey et al’s (1994) literature review that, although a large majority of CD children have prior histories of ODD, many ODD children do not go on to develop CD. This raises a question: Are there two types of ODD, one that progresses to CD and one that does not? The present study found only one statistically significant difference in familial rates of ill-ness between ADHD1ODD probands and either ADHD1CD or ADHD-only probands. The siblings of ADHD1CD probands had greater rates of the combined category CD or ASPD compared with siblings of ADHD1ODD probands (p, .01).
For the comparisons with ADHD1CD probands, non-significant differences could reflect low statistical power, given the small number of relatives in the ADHD1CD group (n 5 40). For example, although not statistically significant, there was a two-fold increase in the rate of CD in relatives of ADHD1CD compared with ADHD1ODD probands. For siblings, there was a nine-fold increase for CD. These differences would likely have attained signifi-cance in a larger sample. By contrast, we had adequate statistical power for comparisons between ADHD1ODD and ADHD-only families (ns5 117 and 260, respective-ly). This gives greater certainty to our finding of no differences between these two groups.
some of the ADHD1ODD children are similar to ADHD1CD children, whereas others are similar to ADHD-only children. Such heterogeneity in the ODD group would tend to blur distinction between it and the two other groups.
Because we did not examine a sample of CD children without ADHD, our results cannot determine whether the increased familial risk observed among relatives of ADHD1CD probands is due to the antisocial component of CD or to an interaction with the ADHD syndrome. The work of Lahey et al (1988) suggests that the comorbidity of ADHD and CD confers additional familial risk beyond that of CD alone. Their results clearly indicate that the risks for antisocial personality and substance abuse are greater among fathers of ADHD1CD probands, compared to those with either ADHD alone or CD alone. Children with ADHD1CD have also been shown to have a greater variety and severity of antisocial behaviors compared to children with CD alone (Walker et al 1987). Another group (Szatmari et al 1989) found that children with ADHD1CD appeared to represent a true hybrid disorder rather than one diagnosis or the other. Like ADHD children, the mixed group had more developmental delays than CD children, and like CD children, they had more psychosocial disadvantage than ADHD children. A review of the literature by Hinshaw (1993) concluded that chil-dren with ADHD1CD have an earlier age at onset of CD, are more aggressive, and have more persistent CD than other CD children.
The strength of our conclusions is further mitigated by some methodological limitations. Notably, the number of ADHD girls with CD was small, which limits the power of our analyses, because there were only 40 family members from ADHD1CD families, which were compared with the 117 members from ADHD1ODD families, the 260 mem-bers from ADHD-only families, and the 369 memmem-bers from control families.
Also, findings based on a clinical population should be interpreted with caution, because they may not generalize to other populations. Our diagnosis of ADHD, CD, and ODD among parents of probands relied on retrospective data, which may be subject to recall biases that may not be independent of the proband diagnosis. Although relatively little is known about the validity of these retrospective diagnoses, several studies have shown it possible to validly diagnose ADHD in adults (Biederman et al 1990a; Cantwell 1985; Conners 1985; Varley 1985; Wender et al 1985).
Another methodological shortcoming pertains to our assessments of psychopathology in children. Because they used both interviews with mothers and direct interviews of children, they may be subject to several potential con-founds. First, similarities between children within a family
could be exaggerated by using a common source of information. The direct interview of a family member could be biased if the reporter was aware of the proband’s diagnoses. Second, a halo effect (i.e., a bias toward reporting a second illness in the presence of another) could lead to an overestimation of the comorbidity between ADHD and antisocial disorders and the degree of cosegregation.
Although we have tested seven hypotheses, these do not exhaust the universe of plausible hypotheses. For example, hypotheses six and seven are rejected only if the factors that lead to a secondary disorder are independent of factors leading to that disorder in the absence of the primary disorder. Thus, our results should be interpreted cau-tiously. Replication by other groups would be very useful, as would the testing of these hypotheses in a twin sample. Despite these limitations, the data in this report can be considered as suggestive of a useful working hypothesis: that the combined syndrome of ADHD plus CD in girls may be familially distinct from ADHD without CD. This work generalizes findings from studies of boys and pro-vides some evidence for the nosologic validity of the ICD-10 category of hyperkinetic conduct disorder. Per-haps future revisions of the American DSM-IV should consider including this comorbid condition as a separate category.
This work was supported in part by Grants Nos. RO1 MH41314-07 (JB) and R01MH57934-0 (SVF) from the National Institute of Mental Health, Bethesda, Maryland.
References
American Psychiatric Association (1994):Diagnostic and Sta-tistical Manual of Mental Disorders,4th ed. Washington, DC: American Psychiatric Association.
August GJ, Stewart MA (1983): Familial subtypes of childhood hyperactivity.J Nerv Ment Dis171:362–368.
Biederman J, Faraone SV, Keenan K, Steingard R, Tsuang MT (1991a): Familial association between attention deficit disor-der and anxiety disordisor-ders.Am J Psychiatry148:251–256. Biederman J, Faraone SV, Keenan K, Tsuang MT (1991b):
Evidence of familial association between attention deficit disorder and major affective disorders.Arch Gen Psychiatry
48:633– 642.
Biederman J, Faraone SV, Knee D, Munir K (1990a): Retrospec-tive assessment of DSM-III attention deficit disorder in non-referred individuals.J Clin Psychiatry51:102–107. Biederman J, Faraone SV, Mick E, Williamson S, Wilens T,
Spencer T, et al (1999): Clinical correlates of attention deficit hyperactivity disorder in females: Findings from a large group of pediatrically and psychiatrically referred girls.J Am Acad Child Adolesc Psychiatry38:966 –975.
disorder a precursor to adolescent conduct disorder? Findings from a four-year follow-up study of children with ADHD.
J Am Acad Child Adolesc Psychiatry35:1193–1204. Biederman J, Milberger S, Faraone SV, Kiely K, Guite J, Mick
E, et al (1995a): Family-environment risk factors for attention deficit hyperactivity disorder: A test of Rutter’s indicators of adversity.Arch Gen Psychiatry52:464 – 470.
Biederman J, Milberger SV, Faraone S, Kiely K, Guite J, Mick E, et al (1995b): Impact of adversity on functioning and comorbidity in children with attention-deficit hyperactivity disorder.J Am Acad Child Adolesc Psychiatry34:1495–1503. Biederman J, Munir K, Knee D (1987): Conduct and opposi-tional disorder in clinically referred children with attention deficit disorder: A controlled family study.J Am Acad Child Adolesc Psychiatry26:724 –727.
Biederman J, Newcorn J, Sprich S (1990b): Comorbidity in attention deficit hyperactivity disorder. In: Task Force on DSM-IV, editor.Source Book for DSM-IV.Washington, DC: American Psychiatric Association, 145–162.
Biederman J, Newcorn J, Sprich S (1991c): Comorbidity of attention deficit hyperactivity disorder with conduct, depres-sive, anxiety, and other disorders.Am J Psychiatry148:564 – 577.
Cantwell DP (1985): Hyperactive children have grown up: What have we learned about what happens to them? Arch Gen Psychiatry42:1026 –1028.
Caron C, Rutter M (1991): Comorbidity in child psychopathol-ogy: Concepts, issues and research strategies.J Child Psychol Psychiatry32:1063–1080.
Conners CK (1985): Issues in the study of adolescent ADD-hyperactivity.Psychopharmacol Bull21:243–250.
Faraone SV, Biederman J (1994): Genetics of attention-deficit hyperactivity disorder. Child Adolesc Psychiatr Clin North Am3:285–302.
Faraone SV, Biederman J, Chen WJ, Milberger S, Warburton RM, Tsuang MT (1995): Genetic heterogeneity in attention deficit hyperactivity disorder: Gender, psychiatric comorbid-ity and maternal ADHD.J Abnorm Psychol104:334 –345. Faraone SV, Biederman J, Garcia Jetton J, Tsuang M (1997):
Attention deficit disorder and conduct disorder: Longitudinal evidence for a familial subtype.Psychol Med27:291–300. Faraone SV, Biederman J, Keenan K, Tsuang MT (1991a): A
family-genetic study of girls with DSM-III attention deficit disorder.Am J Psychiatry148:112–117.
Faraone SV, Biederman J, Keenan K, Tsuang MT (1991b): Separation of DSM-III attention deficit disorder and conduct disorder: Evidence from a family-genetic study of American child psychiatric patients.Psychol Med21:109 –121. Faraone SV, Biederman J, Mennin D, Russell R, Tsuang M
(1998): Familial subtypes of attention deficit hyperactivity disorder: A 4-year follow-up study of children from antiso-cial-ADHD families. J Child Psychol Psychiatry 39:1045– 1053.
Faraone SV, Tsuang D, Tsuang MT (1999):Genetics and Mental Disorders: A Guide for Students, Clinicians, and Research-ers.New York: Guilford.
Faraone SV, Tsuang MT (1995): Methods in psychiatric genet-ics. In: Tohen M, Tsuang MT, Zahner GEP, editors.Textbook in Psychiatric Epidemiology.New York: Wiley, 81–134.
Frick PJ, Lahey BB, Christ MG, Green S (1991): History of childhood behavior problems in biological relatives of boys with attention deficit hyperactivity disorder and conduct disorder.J Clin Child Psychol20:445– 451.
Gaub M, Carlson CL (1997): Gender differences in ADHD: A meta-analysis and critical review.J Am Acad Child Adolesc Psychiatry36:1036 –1046.
Gershon ES, Hamovit J, Guroff JJ, Dibble E, Leckman JF, Sceery W, et al (1982): A family study of schizoaffective, bipolar I, bipolar II, unipolar, and normal control probands.
Arch Gen Psychiatry39:1157–1167.
Gittelman R, Mannuzza S, Shenker R, Bonagura N (1985): Hyperactive boys almost grown up: I. Psychiatric status.Arch Gen Psychiatry42:937–947.
Halperin J, Sharma V, Siever L, Schwartz S, Matier K, Wornell G, et al (1994): Serotonergic function in aggressive and nonaggressive boys with attention deficit hyperactivity disor-der.Am J Psychiatry151:243–248.
Hinshaw S, Lahey B, Hart E (1993): Issues of taxonomy and comorbidity in the development of conduct disorder. Dev Psychopathol5:31– 49.
Hinshaw SP (1987): On the distinction between attentional deficits/hyperactivity and conduct problems/aggression in child psychopathology.Psychol Bull101:443– 463.
Hollingshead AB (1975): Four Factor Index of Social Status.
New Haven, CT: Yale Press.
Huber PJ (1967): The behavior of maximum likelihood estimates under non-standard conditions. In: LeCam L, Neyman J, editors. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability, Vol 1. Berkeley: University of California Press, 221–233.
Lahey B, Applegate B, Barkley R, Garfinkel B, McBurnett K, Kerdyk L, et al (1994): DSM-IV field trials for oppositional defiant disorder and conduct disorder in children and adoles-cents.Am J Psychiatry151:1163–1172.
Lahey BB, Piacentini JC, McBurnett K, Stone P, Hartdagen S, Hynd G (1988): Psychopathology in the parents of children with conduct disorder and hyperactivity. J Am Acad Child Adolesc Psychiatry27:163–170.
Lahey BB, Russo MF, Walker JL (1989): Personality character-istics of the mothers of children with disruptive behavior disorders.J Consult Clin Psychol57:512–515.
Loeber R, Brinthaupt VP, Green SM (1990): Attention deficits, impulsivity, and hyperactivity with or without conduct prob-lems: Relationships to delinquency and unique contextual factors. In: MacMahon RJ, Peters RD, editors. Behavior Disorders in Adolescence: Research, Intervention and Policy in Clinical and School Settings. New York: Plenum Press, 39 – 61.
Loeber R, Keenan K (1994): The interaction between conduct disorder and its comorbid conditions: Effects of age and gender.Clin Psychol Rev14:497–523.
Milberger S, Biederman J, Faraone SV, Murphy J, Tsuang MT (1995): Attention deficit hyperactivity disorder and comorbid disorders: Issues of overlapping symptoms.Am J Psychiatry
152:1793–1800.
Orvaschel H (1985): Psychiatric interviews suitable for use in research with children and adolescents. Psychopharmacol Bull21:737–745.
Pauls DL, Hurst CR, Kruger SD, Leckman JF, Kidd KK, Cohen DJ (1986a): Gilles de la Tourette’s syndrome and attention deficit disorder with hyperactivity: Evidence against a genetic relationship.Arch Gen Psychiatry43:1177–1179.
Pauls DL, Towbin KE, Leckman JF, Zahner GE, Cohen DJ (1986b): Gilles de la Tourette’s Syndrome and obsessive-compulsive disorder: Evidence supporting a genetic relation-ship.Arch Gen Psychiatry43:1180 –1182.
Reich T, James J, Morris CA (1972): The use of multiple thresholds in determining the mode of transmission of semi-continuous traits.Ann Hum Genet36:163–183.
Reich T, Rice J, Cloninger CR, Wette R, James JW (1979): The use of multiple thresholds and segregation analysis in analyz-ing the phenotypic heterogeneity of multifactorial traits.Ann Hum Genet42:371–389.
Schachar R, Tannock R (1995): Test of four hypotheses for the comorbidity of attention-deficit hyperactivity disorder and conduct disorder. J Am Acad Child Adolesc Psychiatry
34:639 – 648.
Silberg J, Rutter M, Meyer J, Maes H, Hewitt J, Simonoff E, et al (1996): Genetic and environmental influences on the covariation between hyperactivity and conduct disturbance in juvenile twins. J Child Psychol Psychiatry 37:803– 816. Spitzer RL, Williams JB, Gibbon M, First MB (1990):Structured
Clinical Interview for DSM-III-R: Non-Patient Edition (SCID-NP, Version 1.0).Washington, DC: American Psychi-atric Press.
Stata Corporation (1992):Stata Reference Manual: Release 3.1,
6th ed. College Station, TX: Stata.
Stewart MA, deBlois CS, Cummings C (1980): Psychiatric disorder in the parents of hyperactive boys and those with conduct disorder.J Child Psychol Psychiatry21:283–292. Szatmari P, Boyle M, Offord D (1993): Familial aggregation of
emotional and behavioral problems of childhood in the general population.Am J Psychiatry150:1398 –1403. Szatmari P, Boyle M, Offord DR (1989): ADDH and conduct
disorder: Degree of diagnostic overlap and differences among correlates.J Am Acad Child Adolesc Psychiatry28:865– 872. Taylor E (1994): Similarities and differences in DSM-IV and ICD-10 diagnostic criteria. Child Adolesc Psychiatr Clin North Am3:209 –226.
Varley CK (1985): A review of studies of drug treatment efficacy for attention deficit disorder with hyperactivity in adoles-cents.Psychopharmacol Bull21:216 –221.
Walker JL, Lahey BB, Hynd GW, Frame CL (1987): Compari-son of specific patterns of antisocial behavior in children with conduct disorder with or without coexisting hyperactivity. J Consult Clin Psychol55:910 –913.
Wender PH, Reimherr FW, Wood DR, Ward M (1985): A controlled study of methylphenidate in the treatment of attention deficit disorder, residual type, in adults. Am J Psychiatry142:547–552.