MULTISECTORAL ACTION PLAN FOR THE NONCOMMUNICABLE
DISEASE CONTROL AND PREVENTION (2016-2021)
With A Three Year Operational Plan
GOVERNMENT OF BANGLADESH
FINAL DOCUMENT Version: 12 March 2016
With the technical support from
Table of Contents
ABBREVIATIONS ... IV EXECUTIVE SUMMARY ... V
INTRODUCTION ... 1
PREAMBLE ... 1
GLOBAL AND COUNTRY COMMITMENTS FOR NCDPREVENTION AND CONTROL ... 1
SITUATIONAL ANALYSIS ... 2
OVERALL NCD BURDEN IN BANGLADESH ... 2
LINKAGES TO THE BROADER POLICIES ... 3
IMPLEMENTATION STATUS OF NCD CONTROL ... 4
Tobacco control ... 5
Alcohol control ... 5
Promotion of a healthy diet ... 5
Physical activity promotion ... 6
Indoor air pollution control ... 6
HEALTH SYSTEM ORGANIZATION FOR NCD HEALTH SERVICES ... 6
COVERAGE OF NCDHEALTH SERVICES ... 7
HEALTH FINANCING &EXPENDITURE ... 8
MULTI-SECTORALITY IN NCD SERVICES ... 9
Coordination between MoHFW and other agencies ... 9
Coordination within the health sector ... 9
CHALLENGES AND OPPORTUNITIES ... 9
MULTISECTORAL ACTION PLAN FOR THE PREVENTION AND CONTROL OF NCDS ... 10
ACTION PLAN DEVELOPMENT ... 10
SCOPE AND APPROACH ... 10
VISION ... 11
GOAL ... 11
CORE VALUES ... 11
OBJECTIVES ... 11
TARGETS... 12
STRATEGIC PRIORITY ACTION AREAS ... 13
ACTION AREA 1:ADVOCACY, PARTNERSHIPS, AND LEADERSHIP ... 13
Reduce tobacco use... 14
Reduce harmful use of alcohol ... 14
Promote Physical Activity ... 15
Promote healthy behaviors in key settings ... 15
Reduce household air pollution ... 15
Strategic action area 3: Health systems strengthening for early detection and management of NCDs and their risk factors ... 16
Strategic action area 4: Surveillance, monitoring and evaluation, and research. ... 16
STAGES OF IMPLEMENTATION OF THE ACTION PLAN ... 17
MULTISECTORAL NCDCOORDINATION COMMITTEE (MNCC) ... 18
SECRETARIAT OF THE MULTISECTORAL NCDCOORDINATION COMMITTEE (MNCC) ... 18
Coordinating officers for NCDs in partner Ministries and implementing agencies ... 19
Divisional/District/Upazilla Level Committees ... 19
District Level Committee ... 20
Upazilla Level Committee:... 20
Funds for Co-ordination ... 21
Multisectoral collaboration accountability indicators ... 21
A THREE YEAR MULTISECTORAL OPERATIONAL PLAN (JULY 2016-JUNE 2019) ... 22
PRIORITIZATION ... 22
MAJOR ACTIVITIES ... 22
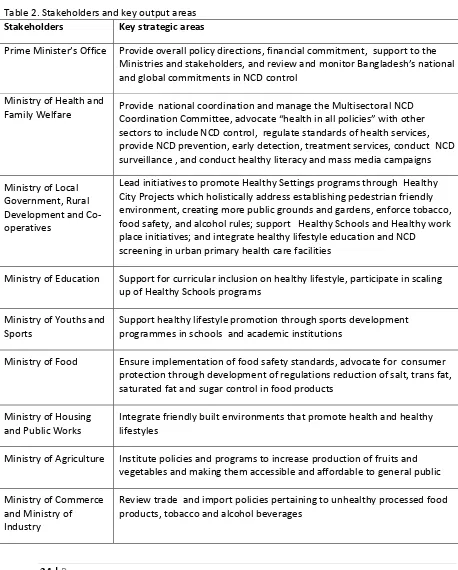
STAKEHOLDER’S KEY AREAS OF RESPONSE ... 24
MONITORING AND EVALUATION ... 26
Annual Consolidated Progress Report ... 26
Reporting period (Financial year)………… ... 26
Table of Contents ... 26
Necessary outputs ... 26
Service coverage indicators ... 27
Implementation evaluation ... 28
LINKING ASSUMPTIONS ... 28
REFERENCES ... 29
ANNEXURE 1.DOCUMENTS CONSULTED ... 30
ANNEXURE 2.ATHREEYEARMULTISECTORALNCDOPERATIONALPLANMATRIX(JULY 2016-JUNE 2019) ... 32
ANNEXURE 3.NCDACTION PLAN INDICATORS AND TARGETS ... 51
ANNEXURE 4:THEMATIC GROUPS FOR THE MULTISECTORAL WORKSHOP ON NCDS ... 55
ANNEXURE 5:THEMATIC GROUPS FOR THE MULTISECTORAL WORKSHOP ON NCDS ... 56
ABBREVIATIONS
ACPR Annual Consolidated Progress Report
ALRI Acute lower respiratory infection
BCC Behavior change communication
BCSIR Bangladesh Council of Scientific and Industrial Research
BHE Bureau of Health Education
BIRDEM Bangladesh Institute of Research & Rehabilitation in Diabetes, Endocrine and
Metabolic Disorders
BNHA Bangladesh National Health Accounts
BSTI Bangladesh Standards and Testing Institution
CC Community clinic
CHCP Community health care provider
COPD Chronic Obstructive Pulmonary Disease
CVD Cardiovascular disease
EDL Essential drug list
FP Family planning
FWA Family Welfare Assistants
DGHS Directorate General of Health Services
DGFP Directorate General of Family Planning
FSA Food Safety Authority
GYTS Global Youth Tobacco Survey
MCH Maternal and Child Health
MCWC Maternal and Child Health Centers
MoHFW Ministry of Health and Family Welfare
MoE Ministry of Education
MoI Ministry of Industry
MoU Memorandum of understanding
MLGRDC Ministry of Local Government, Rural Development and Co-operatives
MNCC Multisectoral Noncommunicable Disease Coordination Committee
NCD Noncommunicable disease
NHFRI National Heart Foundation and Research Institute
NGOs Nongovernment organizations
NICR&H National Institute of Cancer Research & Hospital
NTCC National Tobacco Control Cell
OOP Out of pocket
PSA Public service announcement
SDG Sustainable Development Goals
SFYP Sixth Five Year Plan
TA Technical assistance
THE Total health expenditure
TOR Terms of reference
UHC & WC Union Health and Family Welfare Centers
UPHCP Urban Primary Health Care Project
WHO World Health Organization
EXECUTIVE SUMMARY
Non-communicable diseases (NCDs) which include cardiovascular disease, diabetes, chronic respiratory diseases and certain cancers have become a global problem accounting for more than 68% of the total global deaths. NCDs result in significant socio economic and health care costs due to chronic nature of the diseases requiring protracted treatment. In Bangladesh, NCDs are an imminent public health issue. Currently three quarters of the population are exposed to two or more
modifiable NCD risk factors and 5% of the adult population are diabetic, and 23% hypertensive. NCDs affect both rich and the poor; however, the poor are disproportionately affected leading into the vicious cycle of disease, poverty and non-productivity.
Multisectoral Action Plan for the Noncommunicable Disease Control and Prevention (2016-2021) This Action Plan will be a priority blueprint for action for key stakeholders from 2016-2021 in alignment with the 7th Five Year Plan and the 4th HNP Sector Program of the Government of
Bangladesh. The plan builds on the successes of the implementation of past programmes on control and prevention of NCDs in Bangladesh.
Stages of Implementation of the Action Plan
The Action Plan will be implemented in two stages. The first stage will be implemented through a three year operational plan from July 2016 through June 2019. The second stage of the action plan will be implemented from July 2019 through June 2021 following which the plan of action will be developed for 2025 targets.
The implementation of the action plan employs “Health in All Policies” approach engaging actors outside the health sector that tackle and influence public policies on shared risk factors- tobacco use, unhealthy diet, physical inactivity, harmful use of alcohol, and the exposure to poor indoor air quality. The health sector will play a central role in mobilizing efforts and obtaining commitments from other sectors.
The NCD prevention and control targets have been made coherent with the regional NCD targets for 2025. The actions and activities that are potentially implementable, low costs, bearing high health impact are included in the action plan. Activities are categorized under the followingfour broad strategic action areas.
Action Area 1: Advocacy, partnerships, and leadership
This action area aims to increase advocacy, promote multisectoral partnerships and strengthen capacity to accelerate and scale-up the national response to the NCD epidemic through setting Multisectoral NCD Coordination Committee (MNCC). Engagements of Local Governments and building understandings among stakeholders to participate in NCD prevention, raising political awareness through engagement of political leaders, policy makers, media organizations, and NGO are the main focus of actions under this action area.
Action Area 2: Health promotion and risk reduction
This area promotes the development of population-wide interventions to reduce exposure to key risk factors. These actions include full implementation of the Tobacco Control laws; restrictions on availability informal alcohol among consumers; developing collaborative efforts to reduce trans fats, saturated fat, campaigning for reduction of salt intake; encouraging consumptions of adequate servings of fruits and vegetables, and encouraging physical activity promotion, setting up healthy settings in cities, schools and work places.
Strategic action area 3: Health systems strengthening for early detection and management of NCDs and their risk factors
Actions under this strategic action area aim to improve the efficiency and coverage NCD services to achieve universal health coverage, particularly the primary health care system. Key activities include developing screenings for NCDs, scaling up PEN interventions in primary health care and upazilla health complex, reviewing essential medicine lists (EDL) and make basic NCD drugs available at the primary health care level; and integrating healthy lifestyle education ( physical activity, healthy diet, reduction of salt, tobacco and alcohol) in all health facilities including MCH and FP services;
incorporating NCDs curriculum with primary care focus in pre-service and in-service training center health professionals; and study sustainable health financing options to cover basic NCD services to protect poor from the financial risks.
Strategic action area 4: Surveillance, monitoring and evaluation, and research
This area includes key actions for strengthening surveillance, monitoring and research in NCD control. Key activities include: Conducting ongoing surveys of tobacco, and NCD STEPs at regular interval strengthening national cancer registration through hospital based and population based cancer registries; developing a national priority research agenda for NCDs; implementation
evaluation of the NCD operational framework, and evaluation of compliance with tobacco laws, food safety regulations policies. The National NCD Control Program will compile a yearly Annual
Consolidated Progress Report (ACPR) and submit to the Prime Minister.
A THREE YEAR MULTISECTORAL OPERATIONAL PLAN (July 2016-June 2019)
The three year operational plan is designed to be a result-oriented time bound blue print for Bangladesh to ensure the greater implementation rate of the action plan. Maintaining pragmatism and realism of the implementation are the underlying considerations that guided the selection of the list of activities. The activities are categorized under the four strategic action areas described before. Key stakeholders in the operation plan are: Ministry of Education, Ministry of Local
Government, Rural Development and Cooperatives, Ministry of Food, Ministry of Industry, Ministry of Commerce, Ministry of Agriculture, Ministry of Youths and Sports, Ministry of Housing and Public Works, Academia and NGOs.
Coordination
The three year operational plan will be overseen by a high level Multisectoral NCD Coordination Committee ( MNCC) appointed by the Prime Minister and chaired by the Minister of Health and Family Welfare. The NDCC Program of the DGHS will serve as the Secretariat to the MNCC and will organize six monthly MNCC meetings. Other pathways for coordination include the bilateral sectoral coordination mechanisms. The success of the implementation will depend on how much
stakeholders can explore the bilateral dialogue and partnerships. Inter agency networking can occur through formal and informally pathways; more formal mechanisms include signing a MoU or through formal letters and agreements. Most things can occur informally through a word of mouth. All these choices will be employed to strengthen stakeholder coordination to ensure good success of the implementation.
Monitoring and Evaluation
The progress and the fidelity (Implementation Documentation) to the plan will be assessed yearly. The MNCC Secretariat’s will publish a 20-30 page Annual Consolidated Progress Report (ACPR) containing the progress and performance of stakeholders. The report will be submitted to the Prime Minister and the Cabinet and will be made accessible to stakeholders, funders, and media .
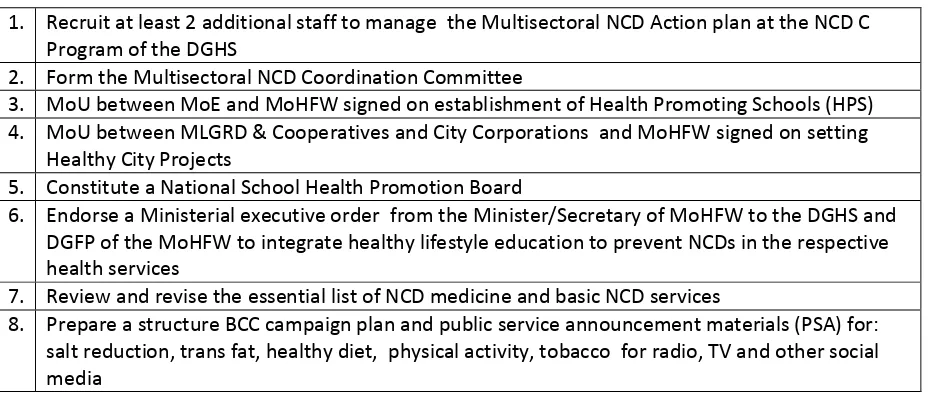
Necessary outputs & service coverage
The initiation and scaling up of the action plan will rely on eight necessary outputs. The earlier these necessary outputs are achieved, the faster can the remaining activities of the operational plan be implemented. A high priority should be accorded to achieve these outputs as soon as the plan is
launched.The three year operation plan contains thirteen key NCD service coverage indicators, most
indicators cumulating to 25 districts. However, the BCC mass media campaign is targeted from year 1 of the implementation. Tobacco enforcement programs already have wider coverage, however, the focus is given to the major cities and 20 districts to ensure a rigorous implementation and monitoring. Overall, maintaining this rate of NCD service coverage gives a high likelihood of achieving 2025 NCD targets.
Implementation evaluation
The implementation (process) evaluation will be conducted towards the early half of 2019 and retrospectively determine the extent to which the plan was delivered as intended in terms of the degree of intensity, coverage and faithfulness, and assess the replicability of the activities in the next phase.
INTRODUCTION
Preamble
Non-communicable diseases (NCDs) which include cardiovascular disease, diabetes, chronic respiratory diseases and certain cancers have become a global problem accounting for more than 68% of the total global deaths.(WHO, 2014a) All age groups are affected by NCDs although NCDs are more common in older age group. Key shared NCD risk factors include tobacco use, unhealthy diet, physical inactivity, and harmful use of alcohol. Overweight/obesity, high blood pressure, raised blood sugar and raised blood lipids, are intermediate metabolic risk factors for NCDs. In Bangladesh, NCDs are an imminent public health issue. Currently three quarters of the population are exposed to two or more modifiable NCD risk factors and 5% of the adult population are diabetic, and 23% hypertensive. (Zaman et al., 2015)
Four key metabolic risk factors that increase the risk of NCDs include raised blood sugar, raised blood sugar (hyperglycemia), high levels of fat in blood (hypelipedemia), and overweight/obesity. These physiological changes are intermediate steps to developing NCDs.
The underlying determinants include globalization and rapid urbanization. While the health sector has a core responsibility in disease management and improvement of population health literacy, interventions in non-health sectors through addressing public policies in tobacco, alcohol, physical activity, and promotion of healthy diet have greater impact in reducing NCD burden. Sectors such as local governments, urban planning, transport, education, agriculture, finance and NGOs therefore, have a great stake in NCD prevention.
NCD result in significant socio economic and health care costs, and is detrimental to sustainable development. (WHO, 2014a)The chronic nature of the diseases requires protracted treatment and can lead to catastrophic expenditure particularly among the poor. NCDs affect both affluent and the poor. However, NCDs can affect the poor disproportionately leading into the vicious cycle of disease, poverty and non-productivity. Investments in NCD prevention are generally not commensurate with the high disease burden despite existence of proven cost effective public health interventions. Low cost solutions to NCD include modifying exposure to common NCD risk factors that include reducing tobacco use, alcohol use, promoting physical activity, and healthy diet. Early detection of NCDs through a primary health care approach is a high impact intervention. Broad based approaches addressing urban infrastructure that promote physical activity, making workplaces, schools and cities conducive to health promoting environment are effective programs. These broad approaches require partnership, leadership and commitment of many stakeholders beyond the health sector. Sectors such as local governments, urban planning, transport, education, agriculture, finance and NGOs therefore, have a great stake in NCD prevention.
Global and Country Commitments for NCD Prevention and Control
Global Initiatives in the area of NCDs started in the year 2000 with the adoption of the World Health Assembly of the Global Strategy for the prevention and control of NCDs resting on three pillars of surveillance, primary prevention and strengthened health care. The UN General Assembly convened a High-Level Meeting in New York in September 2011. The Head of the States in this meeting
Prevention and Control of NCDs and agreed on a comprehensive monitoring framework with indicators and global voluntary targets for 2025. It was also advocated that the Member States translate the commitments by implementing a multisectoral national plans to achieve the NCD targets by 2025. The Government of the Peoples Republic of Bangladesh joined the member states at the UN General Assembly High-Level Declaration on NCDs as well as the World Health Assembly to commit the actions. The Sustainable Development Goal 3 “Ensure healthy lives and promote well-being for all at all ages” provides a high degree of importance to NCD Control and targets to reduce premature NCD deaths by one third by 2030. Other NCD related SGD goals include:
strengthening the prevention and treatment of harmful use of alcohol,achieving universal health
coverage including financial risk protection, improving access to quality essentialhealth-care services, strengthening the implementation of the World Health Organization Framework
Convention on Tobacco Control (FCTC), and supporting the research and development of vaccines and medicines for the communicable and non-communicable diseases.
Bangladesh is also party to other global instruments: the WHO Framework Convention on Tobacco Control, Global Strategy on Diet, Physical Activity and Health, Global Strategy to Reduce Harmful Use of Alcohol, WHO Set of Recommendations on the Marketing of Foods and Non-alcoholic Beverages to Children, including foods that are high in saturated fats, trans-fatty acids, free sugars, which are key instruments for implementing the NCD prevention and control.
SITUATIONAL ANALYSIS
Bangladesh has become a low middle-income country with a steady progress in economic
development. It is also undergoing a rapid socioeconomic and demographic transition particularly with increasing average life expectancy and increasing rate of urbanization. Average life expectancy of Bangladesh has crossed 70 years and approximately 28% of the country’s population resides in urban areas and a half of the country’s population is projected to live in urban centers in next 25 years. (“Local Government Institutional Assessment - Urban Primary Health Care Services Delivery Project (RRP BAN 42177),” n.d.) Bangladesh being among the most densely populated countries in the world (The World Bank, 2014), urban centers will become ever more densely crowded. With Bangladesh’s increasing globalized economy,(Hawkes, 2007) the population is and will increasingly be exposed to constant commercialization of fast food chain, shift in dietary patterns and sedentary urban lifestyle which can have great bearing on the noncommunicable diseases epidemiology in the country.
Overall NCD burden in Bangladesh
Bangladesh is in the midst of a epidemiological transition like many low and middle income countries with shifting profiles from infectious disease to chronic disease burden. NCDs contribute to 44% of the total deaths with individual disease proportions comprising of: CVDs (17%), cancer (10%),
chronic respiratory diseases (11%) and diabetes (3%). (WHO, 2014b) The 2013 NCD STEPS survey1
shows high prevalence of NCD risk factors among Bangladeshi people:
• Three quarters of the population are exposed to two or more risk factors with a high
proportion of clustering of risk factors
• More than 93% of the people consumed less than recommended minimum of 5 servings of
fruits and/or vegetables per day
• 38% did not achieve weekly recommended physical activity (>=600MET-minute per week),
38% of men are daily smokers, while some form of smokeless tobacco is equally consumed in 27% of men and women
1
STEPS survey is a WHO standardized survey protocol which collects information on NCD related risks, behaviors and metabolic information of the participant.
2 | P a g e
• Hypertension, an intermediate risk factor for CVDs and heart attack was prevalent in 21% of the population
• 20% of the population were overweight, and approximately 5% were diabetic
Population data on salt intake is limited. In a recent study among 200 residents in Bangladesh, mean intake of salt was 10-11 gm/day much higher than the WHO recommended daily intake of 5 gm. Of concern is that there was no decrease in exposure to risk factors when compared by three STEPS surveys from 2006 to 2013 except for a slight reversal of tobacco use rates as shown in the figure below.(Zaman et al., 2015)
Linkages to the broader policies
In the past the focus had been on the MCH and communicable diseases and NCD control has not been a priority. (Islam et al., 2014) In growing response to the NCD burden, Bangladesh government has taken several steps to put NCD control as a priority health agenda. Multiple national policy documents have acknowledged the rising concern of NCDs in Bangladesh. The National health Policy 2011 outlines approach of integration of prevention, treatment and rehabilitation services at all levels of health care particularly for diabetes, high blood pressure, heart diseases through lifestyle changes and health promotion awareness. The Population and Nutrition Sector Development Programme (HPNSDP) 2011-2016 also planned greater integration of programs to promote social and economic conditions for conventional and non conventional NCDs. The HPNSDP’s articulation and implementation have been linked to the government’s Sixth Five Year Plan (SFYP) for 2011-2016. The upcoming 4th Health, Nutrition and Population (HNP) Sector Program (July 2016-June 2021) and the Health Strategy for the 7th Five Year Plan which will go into effect from June 2016 recognizes the urgency of NCD control as an important agenda and elaborates linkage to Sustainable Development Goal of the UN. In particular the Health Strategy for the 7th Five Year Plan envisages
implementing “massive health promotion for impending noncommunicable disease.”2 The 4th HNP
Sector Program which will feed into the 7th FYP give emphasis on laying strategies to introduce reforms in health financing focusing on risk protection the poor.
2
(Page 31, Health Strategy for Preparation of 7th Five Year Plan)
3 | P a g e
Also reviewing health financing and achieve universal health coverage in the 7th Five Year Plan have been prioritized with the aim to reduce Out of Pocket Payment (OOP) as percentage of Total Health Expenditure from 64% to 48% and reduce household facing catastrophic health expenditure from
15% to 10% by from 2016 to 20213. Reducing OOPs should ensure greater financial health protection
and improving access to health services including NCD prevention, treatment and rehabilitation. Also to support the overall health regulatory and stewardship, the 4th HNP Sector Plan provides avenues for quality control and standardization of services in public and private services for NCDs.
Implementation status of NCD control
The HPNSDP had launched a series of activities for NCD control. The MoHFW responded to the global and regional call to fight NCDs by adopting the Strategic Plan for Surveillance and Prevention of NCDs in Bangladesh (2011-2015), primarily a health sector plan to address the NCDs. Despite good plan, majority of the activities remained unimplemented or were only partially implemented. (Zaman, 2015) Major activities carried out under this strategy were STEPS Survey and piloting PEN Intervention in 2013, in a neighbouring district of Sathkhira in Debhata upazilla health complex covering five union subcenters and 15 community centers. A three-year 2014-2016 National Communication Strategic Plan to reduce NCDs spearheaded by the Bureau of Health Education of the MoHFW listed pertinent activities but the implementation fidelity of this plan was generally very low. Notable activities included implementation of pilot activities. Health Promotion Models Villages for NCD Control have been established in few areas, and Model School Initiatives have been initiated in ninety-one schools in rural areas. Although these pilot initiatives have not been subjected to a rigorous evaluation, they can be potentially scaled up if found effective. Schools are also
reached with health education through School Health Program of the DGHS through a MoU with the MoE. However, mainstreaming of health education in school systems should be further reinforced by transferring ownership of the MoE for greater sustainability of the program.
NCD health literacy improvement at best is in the initial phase of development. DGHS is using the health educators and existing health system to conduct courtyard meetings and healthy facility based education. NCD corners were set up in selected health facilities. Use of mass media for NCD health information is patchy. A proper BCC and social marketing campaigns have not been
conducted so far.
Over the years, there had been substantial advocacy activities particularly targeting senior policy makers in health sector, academia and health institutions. Mobilizing other sectors to participate in NCD agenda in the past have been slow although trends of increased participation by other sectors noted lately are encouraging. The “whole government approach” is yet to realize the full potential and more focus is needed to educate non-health sectors in their role in generating positive health outcome.
Chittagong , Cox’s Bazaar, and Syhlet were few cities in Bangladesh that successfully implemented Healthy City Project in 1990s.(World Health Organization, 2000) However, the efforts have
diminished or disappeared over the years. Today, these programs have become more necessary with the surge of NCDs to promote healthy lifestyle within the context of increasing urban population and complex urban environment. These activities should be further revived and make ground breaking health promoting initiatives in urban settings.
Several researches had been conducted in the country to build evidence for policy making in NCD control. Three rounds of STEPS Survey, GYTS, Global Adult Tobacco Surveys provide ample evidence for NCD risk factor prevalence. The use of research information into practice is still at an early stage;
3
(Page 29, Health Strategy for Preparation of 7th Five Year Plan).
4 | P a g e
however, information use should accelerate in the coming years with the growing momentum of NCD control in the country.
Bangladesh has been a global health leader in generating some of the best practices and evidences in many areas of public health. Even in the area of NCD control, Bangladesh can use yet another opportunity to innovate intervention to combat the emerging threat of NCDs. Furthermore, the existing “best buys” documented in other countries can be implemented to fast track the
achievements in NCD control. Specific risk factor interventions described in the following section are underway.
Tobacco control
Bangladesh implemented tobacco control activities with fairly good success guided by the National Strategic Plan of Action for Tobacco Control framed for 2007-2010. Notable achievements include the formation of the Tobacco Control Taskforces at the national, district and Upazilla levels since 2007 with the coordination of the National Tobacco Control Cell of the MoHFW. The Government in February 2015, revised the Taskforce members. By far, most of these Taskforces have been regularly meeting particularly at the national level. The taskforces are funded by the Bloomberg initiatives. Media dissemination of pictorial warnings is in the advance phase of planning and ready to be launched.
Enforcement activities are being carried out by mobile courts. However, more work needs to be done in tobacco control to create a culture of acceptance and self-regulation among smokers. Smoking at homes is still common(Zaman et al., 2015) and violation nonsmoking rules of public place and work places are common. Awareness on ill effects of tobacco use and policy and legal approaches of tobacco control should be integrated in school curricular systems to educate sustain greater support for tobacco control in future. The illicit tobacco trade is a problem that has not been addressed. Most importantly, farmers who depend on tobacco farming needs to be supported with alternative livelihood while controlling the domestic tobacco production and farming. Taxation of tobacco including smokeless tobacco products should be reviewed to make the product less affordable.
Alcohol control
The consumption of alcohol is strictly prohibited as a social function by islamic culture in Bangladesh. The Narcotic Control Act 1990 provides legal framework but there is no standalone alcohol control act in Bangladesh. Alcohol is heavily taxed, 431% for beer, and 559% for wine and spirit. (WHO, 2013) Yet, the problem of alcoholism is noted in certain sections of the society and about 2% consumed alcohol in the past 12 months and among them 4.2% were daily drinkers.(WHO, 2013) Although the problem is more serious in urban areas (probably due to easy accessibility of alcoholic beverages), alcohol use is noticed in rural areas. Local alcoholic beverages called cholai and tari are consumed by the lower socioeconomic classes, while workers drink another distilled beverage called Bangla Mad. In addition, alcohol is being produced by some pharmaceutical industries in
Bangladesh. Moreover, some crude forms are produced and used by the poor, usually by
fermentation of boiled rice, sugar-cane, and molasses. In the past clusters of alcohol poisoning have been documented. Communities engaged in alcohol consumption should be educated on hazards of alcohol use.
Promotion of a healthy diet
Many NCD health advocacy materials are available; however, well-planned strategic interventions have not occurred at a population level. The nutrition program of the MoHFW and other agencies are involved in awareness -raising activities but its coverage is apparently low. Salt reduction campaigns have not yet occurred although an initial stakeholder consultation has been conducted. The Food Based Dietary Guidelines are at the final phase of translation. This document can be used
widely for public education once formalized. Despite the increasing problem of an increasing overweight population, Bangladesh is facing a significant problem with malnutrition
The Food Safety Act 2013 of Bangladesh provides basis to ensure safe food products including content labeling. The national codex committees for various areas have been set up with the support of the FAO and WHO. Institutional framework through Bangladesh Standards and Testing Institution and Food Safety Authority provides strong institutional mechanism to regulate trans fat, saturated fat, salt contents. In addition to expansion of health literacy programmes and strengthening regulatory efforts, increasing taxes on unhealthy products should be considered.
Physical activity promotion
Physical activity promotion at population level is low. There is no national recommendation on physical activity; however, the WHO recommendations of physical activity though generic can be adapted for Bangladesh. Physical activity promotion directly links to urban environmental design, availability of public places and friendly built environment. The Healthy City Projects conceived in 1990s should be revived and expanded to other urban settings with the ownership of the Local Governments. Health promoting model schools were piloted in 18 schools in 7 divisions, however, the focus on NCD risk factors have been poor. Moving forward, even few key steps such as making the existing footpaths free from vendors, removing construction materials and extended activities from sidewalks relief spaces and promote walkability in urban sites. Also municipalities could take leadership responsibility to promote biking lanes, free space like parks, lakes, ponds inspiring people to walk more to avoid motor vehicle.
Indoor air pollution control
Biomass fuel is a very common source of indoor air pollution and more common among rural and urban lower socio economic groups. (Nath et al., 2013) This includes wood, crop residue and dung. According to the WHO 2012 Household Fuel survey, 89% of households in Bangladesh were using dirty and smoke producing biomass fuels. Particulate matters (PM) with diameter less than 10 microns or PM10 are commonly used indicator of indoor air pollution. Research carried out in
Bangladesh had shown that the mean PM10 concentration over 24 hours is 300um/m3 though during
the hours of cooking the mean hourly concentration typically increase by a factor of three. (World Bank, 2006)Adulthood women spend 3.8 hours per day next to the stove in the kitchen area. As they are also responsible for childcare the youngest children are usually remain by their side. As a result many infants are breathing indoor smoke for several hours each day. (Susmita Dasgupta, 2006)This level of exposure is equivalent to consuming two packs of cigarettes per day. Thus Bangladeshi women and children are exposed to high level of indoor air pollution and it is highly probable that this contributes substantially to the under-five mortality due to ALRI and COPD deaths in women.
This extent of exposure adds a large burden of disease; WHO estimates that 3.6% of the total burden of disease in Bangladesh is associated with indoor air pollution. There are NGO led rural projects on improving cooking stoves in Bangladesh. More initiatives are required to increase the coverage of such projects to reduce use of biomass fuels for cooking and heating. Addressing indoor air pollution is challenging particularly in cities, slums and crowed urban housing environments. Exposure to indoor tobacco smoke inside home is an additional concern resulting in passive smoking among non-smokers including children. Massive social mobilization and education should be launched to make second hand smoke exposure at homes socially unacceptable, and in work places and other public places, legally punitive.More political and social advocacy is needed emphasizing on renewable & green energy as a safe & health friendly source of energy.
Health system organization for NCD health services
In general health services in Bangladesh are provided through mix of public and private systems. The Ministry of Health and Family Welfare (MoHFW) is the main government coordinating and
regulatory agency for NCD services in the country. The DGHS’s NCD Line directorate is the key coordinating agency while the executive functions dispersed among various directorates of the MoHFW. The DGFP deliver some level of coincidental services on lifestyle education along with the family planning and reproductive health services at Maternal and Child Health Centers (MCWC), Union Health and Family Welfare Centers (UHC & WC) and Community Clinics (CC).
Most of the rural populations is provided through the public systems consisting of district and general hospitals, Upazilla Health Complexes,Union Subcenters, Rural sub Center and Community Clinics. The medical colleges and specialized hospitals are mandated to serve within their
geographical jurisdiction.
Respective local government institutions (city corporations and municipalities) are responsible to provide primary health care. Ten city corporations and four municipalities outsource health service projects to NGOs through Urban Primary Health Care Project (UPHCP). NGO play an important role in providing NCD health services through a public-private partnership mechanism. Many primary health care projects are managed by NGOs. Alternative Private Providers consisting of traditional medicine such as homeopathy, kobiraj and untrained allopaths also provide health services in rural and poor communities.
Coverage of NCD Health Services
The primary and ambulatory care of NCD service are provided through the network of facilities, through community clinics, and by private formal and informal NGO providers. However, NCD management and treatment services are not adequately available. The 2014 Bangladesh Health Report suggests that the diagnostic capacity for screening tests was low, with only 24.6% of the district and upazilla public facilities having the capacity to conduct blood glucose testing. In addition among NGO clinics and private hospital settings less than 50% of the facilities had the ability to perform blood glucose testing. Similarly, cancer screening and detection capacity at UHC level is low due to inadequate facilities.
At the primary care level, NCD services are not well integrated for lifestyle promotion. The urban primary health care providing MCH, immunization and family planning services, are not mandated to provide NCD services. The mandate to provide NCD services should be urgently revised, and PHCs should provide tobacco cessation counseling, lifestyle education to reduce salt, consumption of vegetables and fruits. The CPHC, FP and CC should provide basic lifestyle education counseling pertaining to tobacco cessation, lifestyle education, dietary salt reduction, and recommend daily dietary fruit and vegetable consumption.
The referral links are the weakest in the health system among the providers. There are no standard practices in referral chains; patients are left to choose their referrals centers in most cases. Even the essential package of health services is not adequately equipped. On an average less than 6% of public facilities (district and upazilla-level facilities, union-level facilities, and community clinics) had approved essential medicines. For example, among lower level primary care centers, only 5% of all health facilities had atenolol tablets. However, atenolol was available in 73% of DHs, 55% of UHCs, and 60% of private hospitals on the day of the survey. Glibenclamide capsules were available in 17.8% of district and upazilla public facilities. (2014)
The public sector is at the early phase of providing NCD services at the primary care level. (Bleich et al., 2011) Primary health care facilities can be reoriented to provide basic screening and referrals to centers with doctors. Health workers have to be trained and oriented on basic NCD services. PEN screening services piloted in Bangladesh can be useful to expand the NCD gaps in primary care. Even though provision of basic health is a constitutional mandate, basic NCDs have not been included and
by far are still not accessible. Linking NCD services with other services of maternal child health, disability prevention services, chronic diseases such TB, HIV can improve efficiency of health care services. Lifestyle education and counseling is weak and disorganized in the lower level of health facilities. Cadre of health counselors need to be professionalized and appointed at designated NCD Corners in health facilities to expand lifestyle promotion services.
NCD prevention and lifestyle education services are provided at the tertiary care secondary or tertiary management. There are disjointed approaches for capacity enhancement programs for primary care physicians provided by tertiary institutes such as BIRDEM and NHFHRI4, where individual physicians seek training opportunities on management of CVDs or diabetes. While such trainings are useful, more coordinated programs for the primary care providers can ensure coverage and scope of NCD services. The Bangladesh Network for Noncommunicable Disease Surveillance and Prevention (BanNet) is a platform for the collaboration of organizations promoting and collecting information on NCD surveillance and the National Survey on NCD Risk Factor. Tertiary institutes and medical colleges can play a crucial role in capacity building of NCD services. Many private and public institutions provide NCD related services. As an example, BRIDEM and NHFHRI provides education on salt reduction, hypertension, CVDs and diabetes management and prevention with their
affiliation bodies present in various districts and sub districts. Also tertiary institutes have the opportunity to lend their community services to reach the unreached such as urban slum and marginalized populations. Such initiatives will require close collaborations with the MoHFW so that outreach services can be strategically targeted to reach the poor. The role of the private sector in the treatment of NCDs is growing as well as necessary. The government needs to institute well-regulated NCD services through engagement of NGOs.
Health Financing & Expenditure
BNHA-IV estimates total health expenditure (THE) at 3.5% of GDP (325,094 million) and a relatively low per capita THE at BDT 2,144 (US $27). The household out-of-pocket expenditure (OOP) makes up to 63% of THE while the government financing accounts for 23% of THE. The OOP health expenditures of THE are equally high in urban ( 68%) and rural (61%) in rural areas.(2015) NCD management requires prolonged treatment and care, which has bearing on the OOP and increase catastrophic health expenditure among the poor and marginalized. Patients ticket fee ranging from 3taka, 5 taka to 10taka at UHC, district hospital and higher levels respectively are affordable.
However, patients end up paying extra costs on diagnostics and medicines including under-the table payments to providers at times which are too expensive for the poor. Innovative financing models should be introduced to cover NCD services. Proposed financing mechanisms include:
Pre-payment for NCD Package- no cost at the point of service while availing NCD services;
Review of Bangladesh Essential Service Package and explore possibility of integrating the
NCD package, ensuring availability and affordability;
Integrated Essential Package of Services at district level and below-NCD Annual Voucher with
minimum cost; card system , -Consider integrating in the development of health insurance package (LT)
The existing fee structure should be changed even if the above three strategies cannot be implemented.
Other mechanisms such as private sector contribution (philantrophists) and community group contributions should be explored. Government’s health budgetary support is among the lowest in the Southeast Asia region. Policy decisions to increase health budget allocation to primary health care such as using revenues from tobacco tax can provide options for government investment on
4
8 | P a g e
healthcare. Public Private Partnership in NCD promotion should be tapped through engagement of civil society /NGOs.
Multi-sectorality in NCD services
Coordination between MoHFW and other agencies
The role of NCD prevention and control spreads across many sectors. MoHFW should have clear priority-implementing partners from other sectors. In particular: MoE, Local Governments, City Corporations, Food Regulatory agencies and Bangladesh Food Testing Institution and academia and hospitals, Ministry of Agriculture, Ministry of Industry, Ministry of Commerce and NGOs. The inclusive approach can be enhanced using the existing linkages and forming NCD stakeholder consortium. “Health in all policies” require successful placement of agenda in other sectors. Other sectors can be brought on board, when they are convinced when the linkages of their program to health are clear. Although Ministries and other sectors are addressing key health related issues, further work remains to “bringing different Ministries to hook multisectoral engagement in a common platform to improve health to address SDGs and achieving UHC”. (Assessing Health in All Policies in Bangladesh) Effective inter-ministerial coordination is required for the implementation of inter departmental and intradepartmental activities.
Coordination within the health sector
Key agencies within the MoHFW also need work in coordination to build synergies and avoid duplications. Effective consultation and coordination mechanisms are required among various departments and units within the MoHFW tackling various components of NCD, such as
Reproductive Health Services, NTCC, and Bureau of Health, Oral Health, Cancer Prevention. DGHS and DGFP in particular should coordinate activities both at the central and the grass root levels. The coordination mechanism should meet at periodic intervals to discuss the implementation of health programs including NCDs.
Challenges and opportunities
• The NCD prevention and control requires strong national stewardship of the MoHFW to
coordinate a meaningful multisectoral response. Raising priorities to NCD issues in other sectors such as – the Ministry of Education, Ministry of Local Government, Ministry of Agriculture, and Ministry of Food needs further attention.
• Coordination and streamlining with other ministries as well as within the MoHFW requires
full time commitment and staff.
• DGHS and DGFP require closer implementation dialogue to coherently integrate activities at
grass root health facilities.
• Equipping primary health care with basic medicine and technology for NCD services to make
the primary care functional and accessible setting up effective referral system requires commitment and investment in health sector.
• While public-private partnerships in NCD series are promoted, regulating the services is critical to ensure that service providers comply with the set standards.
• Similarly, NCD services in private sectors should be promoted but well regulated.
• Providing NCD services in underserved slum and street dwellers remains a challenge.
Despite gaps, Bangladesh is making strides to prioritize NCD services. A mulitsectoral response to NCDs will be necessary to further consolidate an effective national response to control the growing threat of NCDs.
MULTISECTORAL ACTION PLAN FOR THE PREVENTION AND CONTROL OF
NCDs
Action Plan Development
This Action Plan for NCDs will be a priority blueprint for action for key stakeholders from 2016-2021 in alignment with the 7th Five Year Plan and the 4th HNP Sector Program of the Government of Bangladesh. The plan will feed into fulfilling the Universal Health Coverage in the context of the SDG. The plan is developed through multisectoral consultations and has coherence to the Global Action Plan 2-13-2020) and the Regional NCD Action Plan of the SEARO. The plan outlines the broad action points under four strategic actions. The foundation of the Action Plan is the upcoming 7th FYP, 4th HNP Sector Plan, ongoing reviews, and the government plans. Mechanisms for multisectoral were outlined with the full participation and consensus of the key stakeholders at a national workshop conducted on August 11, 2015. A three year detailed operational plan has been outlined in consultation with the stakeholders.
Scope and approach
The key focus of the action plan is addressing conventional NCDs which, include four diseases – cardiovascular diseases, cancer, chronic respiratory diseases and diabetes which make the largest contribution to mortality and morbidity due to NCDs. The approach to the implementation of the action plan employ “Health in All Policies” approach engaging actors outside the health sector that tackle and influence public policies on shared risk factors- tobacco use, unhealthy diet, physical inactivity, harmful use of alcohol, and the exposure to poor indoor air quality. The health sector will play a central role in mobilizing efforts and obtaining commitments from other sectors while at the same time taking the responsibility in enabling health system to respond effectively to the health care needs of the Bangladeshi people. In particular, primary care interventions that form the basis for a population wide coverage for NCD services have been given priority keeping in mind the linkages to the tertiary care needs.
The actions and activities that are potentially implementable, low costs, bearing high health impact, and that are culturally and political acceptable and financially feasible are included in the action plan. Importantly, the activities proposed in the plan have direct links to the priorities set in the 7th
FYP and the 4thHNP Sector Program to be implemented within 2021 and therefore bear the high
likelihood of funding support within the existing plans.
Vision
The vision of the Multisectoral NCD Action Plan is to contribute towards making Bangladesh free of the avoidable burden of non-communicable disease deaths and disability5.
Goal
The goal of the Multisectoral NCD Action Plan is to reduce preventable morbidity, avoidable disability and premature mortality due to NCDs through multisectoral collaboration and coordination and “health in all policy” approach.
Core values
• Involving the whole-of-government and whole-of-society approach: Build multisectoral partnerships among government, nongovernment, and communities in NCD policy development and programme implementation;
• Universal health coverage: All people should have access to promotive, preventive and curative, and rehabilitative basic health services;
• Cultural relevance: Policies and programmes should respect and take into consideration the specific cultures and the diversity of populations in Bangladesh;
• Focus on reducing inequities: Policies and programmes should address the social
determinants and need of the poor and marginalized communities, and reduce the health and social inequities; and
• Life-course approach: NCD services should occur at multiple stages of life starting with maternal health including preconception, antenatal and into old age.
Objectives
1. To accelerate and scale up responses to NCDs through an effective multi-sectoral
partnerships
2. To improve the capacity of individuals, families and communities to live a healthy life and reduce risk for development of NCDs by increasing health literacy and creating healthy environments, conducive to making healthier choices
3. To strengthen the health system by improving access to health care services for primary
prevention, early detection and treatment of NCDs
4. To establish a sound surveillance, monitoring and evaluation system that generates data for
evidence based policy and programme development.
5
This vision was created by a team of national members at a workshop on translation of evidences to policy formulation for prevention and control of non-communicable diseases in Bangladesh held on 27- 28 January 2013 in Dhaka.
11 | P a g e
Targets
In alignment with the UN High Level Political Declaration of 2011, Bangladesh will commit towards achieving the 2025 NCD targets and 2030 SDG targets. Potential indicators for the 2025 targets are listed in Annexure 3. Through the implementation of the Multisectoral NCD Control and Prevention of NCDs (2016-2021), by 2021 Bangladesh will aim to achieve 50% of the proposed 2025 targets. The 2021 targets are:
Table 1. NCD Targets
Area Baseline 2021 targets
Overall mortality from cardiovascular diseases, cancers, diabetes, or chronic respiratory diseases
* 12% relative
reduction
Reduction in the harmful use of alcohol STEPs
2010
5% relative reduction Reduction in prevalence of current tobacco use in persons aged over
15 years
STEPS 2010
15% relative reduction
Reduction in prevalence of insufficient physical activity STEPS
2010
5% relative reduction
Reduction in mean population intake of salt/sodium * 15%relative
reduction
Relative reduction in prevalence of raised blood pressure STEPS
2010
12% relative reduction
Halt the rise in obesity and diabetes STEPS
2010
0
Reduction in the proportion of households using solid fuels (wood, crop residue, dried dung, coal and charcoal) as the primary source of cooking
Survey 2010
25%
Increase the number of eligible people receive drug therapy and counseling (including glycaemic control) to prevent heart attacks and strokes
25%
Improve the availability of affordable basic technologies and essential medicines, including generics, required to treat major NCDs in both public and private facilities
40%
*to be determined
Strategic Priority Action Areas
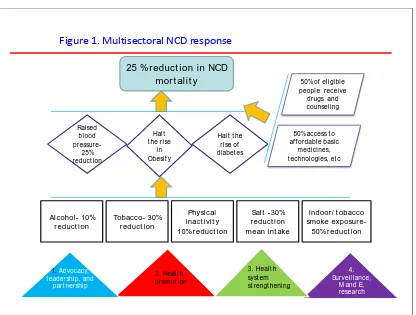
This Plan of Action is based on the four strategic priority action areas outlined in the WHO’s guidance document of Action plan for the prevention and control of noncommunicable diseases in South-East Asia, and it is congruent with the 25 indicators and 10 regional targets of the WHO Comprehensive Global Monitoring Framework. As shown in Figure 2, four action areas will contribute towards the goals and targets mentioned in the previous section.
25 % reduct ion in NCD mort al it y
Al cohol - 10% r educt i on
Tobacco- 30% r educt i on
Indoor / t obacco smoke exposur e-50% r educt i on Physi cal
i nact i vi t y 10% r educt i on Raised bl ood pressure-25% reduct ion Hal t t he rise
in Obesit y
Hal t t he rise of diabet es
Sal t -30% r educt i on mean i nt ake
50% of el igibl e peopl e receive drugs and counsel ing
80% access t o af f ordabl e basic
medicines, t echnol ogies, et c
Figure 1. Multisectoral NCD response
1. Advocacy, l eadership, and
part nership
4. Surveil l ance,
M and E, research
3. Heal t h syst em st rengt hening 2. Heal t h
promot ion
Action Area 1: Advocacy, partnerships, and leadership
Multisectoral approaches for NCDs will require meaningful involvement of a wide range of actors including non-health government sectors, academia, private sector, civil society organizations, other organizations, individuals, families and communities, in undertaking appropriate actions that
contribute to the improvement of health outcome. Effective leadership is required to foster partnerships among various stakeholders to address NCD control.
Actions listed under this area aim to increase advocacy, promote multisectoral partnerships, strengthen capacity for effective leadership, increase political recognition of the societal and economic impact of NCDs and to accelerate and scale-up the national response to the NCD epidemic.
Actions
• Advocate for innovative financing mechanisms in NCDs prevention particularly ear marking
funds from tobacco tax revenues;
• Raise public and political awareness/understanding about NCDs and their risk factors through social marketing, mass media and responsible media reporting;
• Set up an effective national multisectoral coordination mechanisms for NCDs at various
levels of governance and eventually reporting the progress to the Head of the State;
• Catalyze a systematic society-wide national response in NCD control by addressing the
underlying social, environment and economic determinants of health by engaging broad range of actors; and
• Strengthen the NCDC Program as a national unit on NCDs in the MoHFW to be a fulltime
Secretariat and carry out needs assessment, strategic planning, policy development, multisector coordination, and programme implementation and evaluation
Action Area 2: Health promotion and risk reduction
This area promotes the development of population-wide interventions to reduce exposure to key risk factors. These actions include full implementation of the Tobacco Control laws; restrictions on availability of retailed alcohol, with comprehensive restrictions and bans on alcohol advertising and promotion endorsement through implementation of alcohol laws or adoption of the Global
Strategy to Reduce the Harmful Use of Alcohol; replacement of trans fats with unsaturated fat, mass media campaigns on salt intake reduction and reduced salt content in prepackaged or processed foods; encouraging adequate servings of fruits and vegetables, and joining the network of free public places for walking and bicycling. Effective implementation of these priority actions should lead to healthier lifestyle choices among people. It will also lead to implementation of regulations and enforcement programs in tobacco, alcohol, and adhering to food labeling specifications.
Reduce tobacco use
• Accelerate full implementation of the Tobacco Control Act 2013 of Bangladesh;
•
Raise taxes on tobacco products including smokeless tobacco through effective policydialogue with the policy makers and legislators
;
• Advocate for 100% tobacco-free environment in all indoor workplaces, public transport,
indoor public places and strengthen enforcement programs through mobile court checks;
• Implement pictorial health warning on tobacco use including smokeless tobacco through
strategic mass media and behavioral change campaigns;
• Enforce measures to eliminate the illicit tobacco trade, including smuggling, illicit manufacturing and counterfeiting (in line with WHO FCTC Article 6);
• Develop trading substitutes and relocation policies for tobacco farmers; and
• Set up a national quitline for tobacco users.
Reduce harmful use of alcohol
• Regulate commercial availability of alcohol through enforcement of policies;
• Adjust pricing policies on alcoholic beverages at periodic intervals to make pricing deterrent to excessive consumption;
• Support and empower communities engaged in harmful alcohol use to reduce alcohol
consumption through social marketing and community mobilization in identified communities; and
• Amend narcotics control act
Healthy diet high fruits and vegetables and low intake of saturated fats/trans fats, free
sugars and salt
• Disseminate Bangladesh National Dietary Recommendation in mass media and through
channels;
• Conduct public campaigns through mass media and social media to inform consumers about
a healthy diet high in fruits and vegetables and low saturated fat, sugar and salt;
• Implement national salt reduction campaigns in mass media, schools and institutions;
• Support consumer protection groups in Bangladesh to advocate and discourage marketing
of foods and non-alcoholic beverages to children;
• Increase collaboration between salt/sodium reduction programmes and salt iodization
programmes for increased public health gains and higher programme efficiency; • Promote nutritional labeling, according to but not limited to international standards, in
particular the Codex Alimentarius, for all pre-packaged foods including those for which nutrition or health claims are made;
• High tax impose in energy drinks/beverage; • Conduct counter advertisement; and
• Ban advertising, promotion and sponsorship of unhealthy diet.
Promote Physical Activity
• Adopt and advocate the national guideline on physical activity for health;
• Develop multi-sectoral policy measures to promote physical activity through active
transport, recreation, leisure and sports;
• Advocate town and urban planners and increase number of public spaces supporting
physical activity, urban housing complexes that include safe walking and cycling spaces; • Advocate for construction of built and natural environments supporting physical activity in
schools, universities, work places, and health facilities; and
• Carry out mass media campaigns and social marketing to raise awareness on the benefits of
physical activity throughout the lifecycle. • Make the existing footpaths free from vendors.
• Make provision of separate bicycle ways, free space like parks, lakes, ponds inspiring people to walk more to avoid motor vehicle
Promote healthy behaviors in key settings
• Enable healthy settings programs in schools and work places for health promotion activities;
• Establish Health Promoting Schools with guidelines for implementation and mechanisms for
monitoring and evaluation;
• Establish Healthy City Projects with guidelines for implementation and mechanisms for
monitoring and evaluation;
• Conduct advocacy and training workshops among teachers to promote healthy behaviors in
schools and work places; and
• Lobby for discouraging processed food high in saturated fat, sugar and salt from schools
premises and work place catering facilities.
Reduce household air pollution
• Strengthen advocacy in support of transitional to cleaner technologies and fuels (LPG,
bio-gas, solar cookers, electricity, and other low fume fuels)
• Promote private producers to manufacture improved stoves through providing bank loans
and stove designs
• Create mass awareness through popular print and electronic media about the health impact
of indoor air pollution
• Develop programmes aimed at encouraging the use of improved stoves, good cooking practices, reducing exposure to fumes, and improving ventilation in households
• Create awareness and develop appropriate strategies to reduced exposure to second-hand
tobacco smoke in households
Strategic action area 3: Health systems strengthening for early detection and management
of NCDs and their risk factors
Health systems should be strong and core to ensuring the success of NCD prevention and control. To improve the coverage of NCDs services to the maximum in need, the program should be sustained by including as universal health package and providing through a people-centered approach.
Actions under this area aim to improve the efficiency of the health system, particularly the primary health care system. Full implementation of actions in this area should improve access to health-care services, increase competence of primary health care workers to address NCDs, expand community-based approaches for early detection, improve referrals, lead to greater integration of NCDs into heath sector reforms and plans, empower communities and individuals for self-care and ensure evidence-based interventions supported by universal health coverage.
Actions
• Develop screening and NCD identification capacity by scaling up PEN interventions in
primary health care and upazilla health complex ;
• Review essential medicine lists (EDL) and other supplies for treatment of hypertension,
diabetes, CVDs, COPDs and revise the EDL;
• Make basic NCD drugs available at the primary health care level;
• Integrate healthy lifestyle education ( physical activity, healthy diet, reduction of salt, tobacco and alcohol) in all health facilities including MCH and FP services;
• Implement special NCD programs targeting the marginalized and population with special
needs;
• Incorporate NCDs curriculum with primary care focus in pre-service and in-service training
center health professionals; and
• Study sustainable health financing options to cover basic NCD services to protect poor from
the financial risks.
Strategic action area 4: Surveillance, monitoring and evaluation, and research
.Valid and availability of timely data are important for evidence based policy implementation. This area includes key actions for strengthening surveillance, monitoring and research in NCD control. The desired outcome is to improve availability and use of data for evidence-based policy and programme development. Health information systems should integrate the collection of NCD and risk factor data from multiple sources and strengthen competences for analysis and use of the information. The activities should facilitate NCD and risk factor research to enhance the knowledge base of effective interventions; and to support translation of evidence into policies and programs.
Actions:
• Conduct ongoing surveys of tobacco, and NCD STEPs at regular intervals;
• Strengthen national cancer registration through hospital based and population based cancer
registries;
• Document annual consolidated NCD implementation reports of multi-stakeholders;
• Develop a national priority research agenda for NCDs based on the consultations with
academia, WHO, and other stakeholders;
• Support NCD research alliance with academia, stakeholders, WHO and the government and improve use of NCD surveillance and research data;
• Review implementation rate of the current NCD operational framework, and evaluate
compliance with tobacco laws, food safety regulations policies, and evaluate healthy settings programs;
• Integrate the online reporting of NCDs at the district and upazila level with DHIS2 (District Health Information System) of DGHS; and
• Conduct Secondary data analysis of the STEPS survey can be done
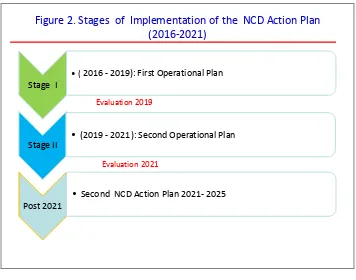
Stages of Implementation of the Action Plan
A relatively short term plan can drive results as opposed to a long range plan which often leads to loss of momentum and suffer from loss of accountability on the way. The Action Plan will be implemented in two stages as shown the figure below to ensure better implementation rate of the plan. The first stage will be implemented over a period of three years from July 2016 through June 2019. The second stage of the action plan will be implemented from July 2019 through June 2021. After stock taking of the implementation of the Multisectoral NCD Action Plan 2016-2021, next plan of action will be developed for 2025 targets.
Figure 2. Stages of Implementation of the NCD Action Plan (2016-2021)
Stage I
•( 2016 - 2019): First Operational Plan
Stage II •
(2019 - 2021): Second Operational Plan
Post 2021
• Second NCD Action Plan 2021- 2025
Evaluation 2019
Evaluation 2021
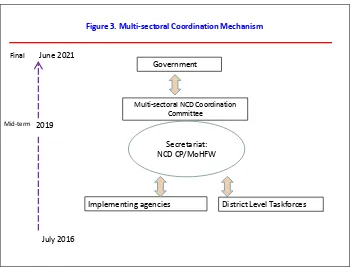
MULTISECTORAL COORDINATION MECHANISMS
Multisectoral NCD Coordination Committee (MNCC)
Prevention and control of NCDs require an effective national and sub-national coordination as it involves a host of Ministries and agencies. Functional coordination mechanisms both at the national and local levels have been in existence for tobacco control in Bangladesh since 2007. The existing tobacco taskforces will be reconstituted for NCD coordination.
At the national level, the Multisectoral NCD Coordination Committee (MNCC) will be constituted under the auspices of the MoHFW. The committee will be chaired by the Minister of MoHFW. The members of the national NCD committee will be not limited to but include: Secretaries of the Ministries of Education, LGRD, Urban Planning, Food, Commerce, Youth and Transport, Women and Children, Social Welfare, Information Ministry of Transport and Home Affairs. Academia and civil society organizations and police will be also invited on board for representation. The key functions of the MNCC are to:
1. Meet six monthly to review the progress of the implementation status of the National NCD
Action Plan
2. Submit a minimum of one yearly implementation status report of the NCD action plan to the
Prime Minister’s Office
3. Provide political leadership and guidance to relevant sectors for the prevention and control
of NCDs
4. Enhance the integration of NCD prevention and control in the policies and programmes of
relevant Ministries and agencies of the Government by distributing/assigning responsibilities to the concern ministries
5. Provide a dynamic platform for dialogue, stock taking and agenda-setting and development
of public policies for NCD prevention and control
6. Facilitate development and resourcing of the multisectoral action plan on NCDs
7. Coordinate technical assistance for mainstreaming NCDs in relevant sectors at national,
regional, district, upazilla and community levels
8. Monitor implementation of the action plan and review progress at national and sub national
levels
9. Disseminate annual progress of NCD Action Plan
10. Report on intergovernmental commitments pertaining to NCDs
Secretariat of the Multisectoral NCD Coordination Committee (MNCC)
The NCD Control Programme of the DGHS will be the Secretariat of the MNCC. It is critical that the Secretariat is staffed with dedicated full time staff with sufficient technical expertise to ensure coordinating responsibilities for the MNCC and sub-taskforces. An under-staffed Secretariat leads to fragmented initiatives, irregular meetings, sparse follow up and limited accountability among the partners. Two additional staff will be recruited to serve as a full time secretariat.
Key functions of the Secretariat are to:
1. Sensitize key stakeholder ministries on NCD concerns
2. Organize meetings of the MNCC
3. Develop the agenda for the meeting in consultation with the Chair and other sectors
4. Request reports on progress of work from stakeholder ministries, districts and upazilla
5. Follow up on decisions taken by the MNCC
6. Arrange technical assistance to line ministries such as for environmental scans for policy initiatives, health impact assessments of policies and capacity assessments of sectors
7. Identify knowledge gaps and advance research priorities to inform policy decisions
8. Support stakeholder in accessing resource needs for implementing their commitments
9. Facilitate bilateral/ multi lateral meetings to advance work on thematic issues and agreed NCD goals, and
10.Prepare consolidated reports on the implementation of the multisectoral action plan for NCDs.
Coordinating officers for NCDs in partner Ministries and implementing agencies
Appropriate arrangements are required in other Ministries and agencies implementing the NCD Action plan. An implementing agency should be required to identity its NCD coordinator to the MNCC. The NCD Secretariat will work with the key partners to ensure that: a coordinator is appointed on time and endorsed by the Head of the Agency, coordinator’s responsibilities are recognized by the parent agency by including the NCD deliverables in his/her personal performance indicator, and the Head of the Agency notifies all units of the agency about the appointment of coordinator. These steps will ensure greater support, recognition and coordination for NCD activities within the organization and with the MNCC.
Coordinator’s key roles are to:
1. Bring the perspectives of the agency on policy matters related to the agency;
2. Present updates and report on the actions taken and challenges faced;
3. Seek and offer solutions to advance work on the agreed goals;
4. Ensure on-going communication with the Secretariat and other sectors; and
5. Report stakeholder’s progress on implementation status of the NCD activities.
Divisional/District/Upazilla Level Committees
• The NCD committees will be constituted at the divisional, district and upazilla levels. The compositions and functions of the committees will be as follow: expanding on the existing tobacco control taskforces. The core functions of these committees are to:
1. Conduct a monthly meeting to monitor the implementation of the action plan;
2. Provide quarterly reports on the implementation of the action plan to the Secretariat of the
MNCC and the parent organizations;
3. Provide cross sectoral coordination to mainstream NCD prevention and control at district,
Upazilla and community levels; and
4. Identify and access local Government resources for the implementation of the plan.
Divisional Level committee
– Divisional Commissioner: Chairperson
– Divisional Director, Health: Member Secretary – Members:
• Divisional Director FP • Director (?) LG Member • DIG of Police
• DD • Education • Information • CHO of City Corp
• Principal and Director of Medical College Hospital • Divisional head of concerned department
Functions
• Monitor and evaluate the