Vol 6, No 2, April - June 1997 Metabolic Defects in Diabetic
Offspring
97
Early
Metabolic
Defects
in
The First-Degree Relatives
of
Patients
with
Non-Insulin-Dependent Diabetes
Mellitus
Wilfried Herdin
SibueaAbstrak
(DMTTI), yang diduga untuk mengidentifilasi pencegahan. Sebanyak û tanpa rtwayat diabetes
dalam
lam penelitian ini.Kedua
ke
i umur, ienis kelaminda
nbuhyang sama. Dilakukantes
oral untukmenilaitoleransi
menilai responsinsulin
sa oral. Darah vena diambil sebelum dan 2 jam setelah pembebananglukosa untuk
menentu
beberapa perbedaan yang bermakia antara anak penderitaDMTTI dan kontrol'
Pa
mengidap toieransi glukosa'rcrjanggu (TGT), sedang paàa kontrolhanya
l
kasus.Untukm
l,anakpeideita
linyang0.5
asmalebihtinggi
DMTTIbah
rinsulinemia dan resistensi insulin merupakan kelainan metabolikrila
donesia.Abstract
glucose. venous blood sampres were taken before and 120 minutes termination. several characteristics of metabolic abnormalities control subjects. They needed higher insulin to maintain the normar had 7 (l2Vo) impaired glucose tolerance cases and only
I
in atives ofNIDDM
with normnl glucose tolerance (NGT). This patients with NIDDM inIndonesia.
ortant early metabolic defects among thefirst-degree relativesof
Keywords: First degree relatives of patients with NIDDM, insulin resistance, hyperinsulinemiaNon-Insulin-Dependent
Diabetes
Mellitus (NIDDM)
constitutes
about 85Voof
all
casesof
diabetesworld-wide
and
is associated
with
anenormous amount
of
morbidity
andmortality
resulting
from
microvascular
and
macrovascular compli :ationi.
l'2Department
of
Internal Medicine, Facultyof
Medicine, University of Indonesia, Dr. Cipto Mangunkusumo Hospital, Jakarta, IndonesiaThe
high
incidence
of
NIDDM
among
first-degree
relatives of
NIDDM
patients
andhigh
concordancein
identical twins provide
evidence that the role ofgenetic
component
in
thedevelopment
of NIDDM is
very
strong.'
The
disease
is
characterized
by
defect in
pancreatic
betacell function
and the resistanceof
the tissues tothe action
of insulin.
298 Sibuea
diabetic
parents,
insqlin
resistance and
hyperin-sulinemia
arealready
present.4
Apparently, both
in-sulin
resistance and impaired
insulin
secretion
are necessaryof
thedevelopment
of
the disease.sThe purpose
of this
study is toidentify
early metabolic
defects
in
the first-degree relatives
of
patients
with
NIDDM
in
Indonesia, which may be useful
in
the strategiesfor
theprevention of
NIDDM.
METHOD
Fifty-five
healthy first-degree relatives
of patientswith
NIDDM
and 55 healthycontrol
subjectswith
nofamily
history
of NIDDM,
matchedfor
age, gender andbody
mass
index
participated in this
study.
At
the
time
of
recruitment,
no
relatives
or
control
subjects
had
adisease
or
received
medications known
to
affect
glucose
metabolism.
Oral
Glucose
Tolerance Test
A 75
gram
oral
glucose tolerance test
wasperformed
to
assess glucosetolerance
andto
measure theinsulin
response to oral glucose.After
a 12 hourovernight
fast,all
subjects were
given
a
75-g
oral
glucose
load.
Venous
blood
samples
were taken before and
120minutes after the glucose was administered
for
deter-mination
of
plasma
glucose and serum
insulin
con-centrations.
Diagnosis
of
impaired
glucose tolerance
(IGT)
was establishedif
thefasting
plasmaglucose (FPG)
was<
140mg/dl
and plasma glucose 2hours after
glucose load(2-h
PG) rangedbetween
140-200mg/dl.
NIDDM
was diagnosed
if
FPG
was>
140mg/dl or
2-h PG was>
200
mgldl.s
Insulin
resistance
as statedby
Berson
and
Yalow
is
defined
asa state
of
abody
in
which
greater-than-normal
amountsof
insulin
are requiredto
éti"it
u quantitatively normal ,"rponr.6
It
was
deter-mined
by
the method
of
Yalow
and Berson with
modification.
Theratios
of
plasmainsulin
and plasmaglucose (fasting VG,
2 hoursVG, total
VGratio)
werecalculated
in
each
group
and
was
interpreted
as thehigher
theratio
the greater theinsulin
resistance.TAssays
and Statistical Analysis
Plasma glucose
was
assayedwith
a
glucose
oxidase method(GOD PAP).
The plasmainsulin concentration
was
measuredusing DPC
reagentsCoat-A-Count
ac-cording
to
standard
Radioimmunoassay
procedureSMed J Indones
performed
by
Immunoendocrinology Laboratory,
School
of
Medicine,
University
of
Indonesia,
WHO
Laboratory
no.
104for
Matched
ReagentProgramme
and
no.
2l
Zone
B for
External
Quality Control.
All
datawere
expressed as mean+
SD.
All
statistical
analysis were
performed by
using
SPSSfor
windows.
Linear
regression analysis
was
used
to
estimate
therequired
insulin
amounts
to
elicit
normal
glucose
levels
at2 hours after
glucoseingestion. Independent
t-test was
used
to
test the differences
between
two
means.RESULTS
A
total
of
110 personswere
studied
: 55 first
degreerelatives
of
patientswith NIDDM
and 55healthy
con-trol
subjectswith
nofamily
history
of NIDDM.
The
age,the
body
massindex
(BMI),
the number
of
male
andfemale
subjectswere
similar in both
groups(Table
1).Table 1. Characteristics of the Study Subjects
Characteristics
Relativesof
Control subjectsNIDDM patients
No. subjects Gender Age (years)
BMI
55
l7M,38F
31.6+10.4 23.8+3.8
55
l7M,38F
31.6+9.9 22.5+3.9
I I
0.9 0-08
Among
themetabolic
characteristics that were studied,there were several differences between the
groups(Table
2).Table 2. Results of Oral Glucose Tolerance Test
Relativesofpatients Control with
NIDDM
subjectsImpaired glucose tolerance Fasting plasma glucose*) 2 hour plasma glucose Fasting plasma insulin**)
2 hour plasma insulin
7l
85.1+11.4
79.4110.5rM.5+27.9
95.9È18.2t3.2+6.4
9.}}5.184.6163
48.9+52 0.03 0_007 o.02 0.004 0.0001*) Plasma glucose in
mg/dl
**) Plasma insulin in mU/LThe
relatives
of
patientswith NIDDM
hadhigher
tGT
cases than thecontrol
subjects ( 7 cases.vs 1 case), andVol 6, No 2, April - June 1997
th
normal
glucoseglucose
andplas-bjects (Table
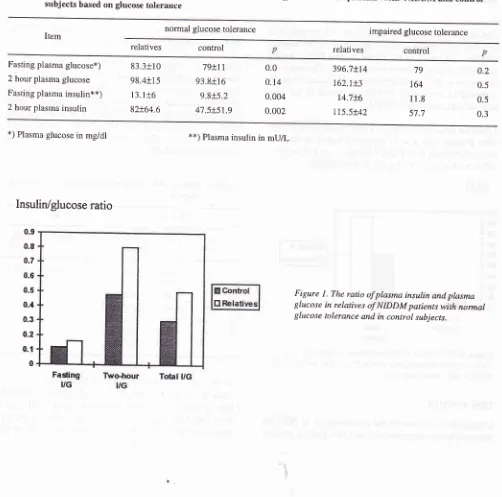
3).By calculating
the ratio
of
plasmainsulin
and plasma glucosein
eachgroup,
it
wasfound that to maintain
anormal plasma glucose level, higher plasma
insulin
con-centration
was neededby
therelatives
with NGT
than bycontrol
subjects(fasting
VG was 0.16 vs0.l2,2hour
VG was 0.8 vs 0.48, and total VG was 0.5 vs 0.3).
This
greater
insulin requirement was
causedby the
presence
ofinsulin
resistancein
this group. (Figure
l).
Metabolic Defects in Diabetic
Offspring
99The relatives of
NIDDM
patientswith
NGT
had 2 hourplasma
insulin
andplasma glucose levels higher
thanthose observed in the control subjects.
By linearregres_
sion analysis the need
of
insulin
amounts
to
elicit
normal
glucose levelscould be quantified
(Felevel
the amountof
theinsulin
requirement was gg,56
mU/I in
the relatives
with
NGT and 51
mU/I
in
the control
subjects.While at
I I 5mg/dl
it was
9l
,6mU/I
and 66mU/I
respectively. Thus there
is insulin
resistancein
therelatives of
NIDDM
patients
with NGT.
Table
3'
Comparison of plasma glucose and insulin level in the lirst degree relatives of patientswith
NIDDM and
control
subjects based on glucose tolerance
Item normal glucose tolerance impaired glucose tolerance
relatives control relatives
Fasting plasma glucose*) 2 hour plasma glucose Fasting plasma insulin**)
2 hour plasma insulin
83.3+10 98.4+15
l3.lt6
82+64.679+11 93.8+16 9.8+5.2 47.5+51.9
0.0 0.
l4
0.004 0.002396.7+14 162.1+3
14.7+6 115.5+42
79 164 11.8
57.7
0.2 0.5 0.5 0.3
*) Plasma glucose in mg/dl
Insulin/glucose
0.9 0.8
0.7
0.6
0.5
0.4
0.3
0.2
0.1
0
**)
Plasma insulin in mU/Lratio
[image:3.595.32.534.291.788.2]r00 Sibuea Med J Indones
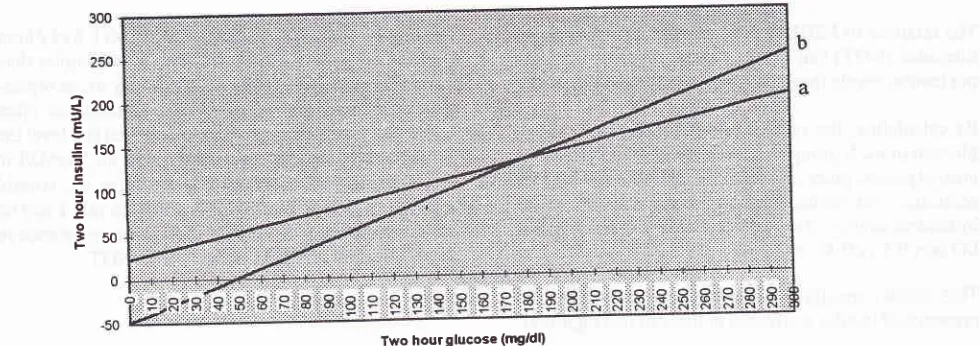
Figure
2.
Two hour plasma insulin level as a fuction of 2 hour glucose level in the relatives of NIDDM patients with normal glucose toierance (a) andthe control subjects (b). Line (a) : y-
22,56 + 0,6(glucose) andline (b): y = -49+1(glucose) represent the regres-sion slope of 2 hour insulin against 2 hour glucose levels.{
2oo2
Ê
:
150 to E:100
o E o -! 50 F
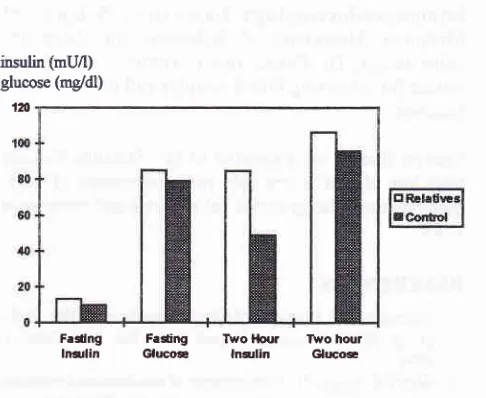
Fasting plasma
insulin in
therelatives of
pationtswith
NIDDM
was
significantly higher
than
in
the
control
subjects
(13.5!6.4 vs
9.75
mU/I,
p=Q.Q01).
As
the age,BMI
and gender were ovenly matched between thetwo
groups,
this hyperinsulinemic difference
can
beregarded
as aresult
of
metabolic
defectsin
the
rela-tives
of
patients
with
NIDDM.
Likewise
as shownin Figure
3, theinsulin level
2 hoursafter
glucoseload
wassignificantly
higher
in
therela-tives
of
patients
with NIDDM
thanin control
subjects(86.9
t
62.7
vs 47!
51.2mU/I,
p=Q.Q0002).mun
concentration
is
the
overwhelming
-risk
factor
long
before the occurrence
of
the disease.)'6Saad
et
al8
reported
that
257oof
the
IGT
subjects developedNIDDM
at 5years
and66Voat
10 years.In
this
study there were 7 casesof
IGT in
therelatives
of
NIDDM
patients and
1in
the
control
subjects.
Their
baseline data
were
shownin
Table 4.
It
wasclear that
IGT
in
therelatives
ofNIDDM
patients wasnot
ageor
BMI
dependent. These
IGT
cases
have
a
risk
of
developing
NIDDM.
Table
4.
Baseline dataof
the Impaired Glucose Tolerance subjectsRelatives
age (year) age
(year) No 90
gt
70 60
flt
tO 3tt
m
10 0
gender
BMI"
(kg/m')
gender
(ke/m")BMI,
I
2 J 4 5 6 ,1
17 JJ 34 43 44 48 60
male
21.8female
22male
24.6male
31.25male
31.2female
22.9female
26.65l
female 24.2Fasting
lnsrlin Two-hour
[image:4.595.305.547.497.662.2]lnsrlin
Figure 3. Comparison of fasting plasma insulin and 2 hour plasma insulin between fi.rst degree relatives of patients with NIDDM and control subjects.
DISCUSSION
Longitudinal
studies
of
the
development
of
NIDDM
reported
in
theliterature
revealed that plasma glucoseIn
the study
of
Warram,4
the 2 hour blood
glucose value was adeterminant factor
for the
development
of
type II
diabetesmellitus (relative risk =
3.5).
He
fol-lowed
up
155offspring
ofdiabetic
parentsfor
13 years andfound
I6Vo(25
subjects)
of
them developed type
Vol 6, No 2,
Apil
- June 1997lI
diabetes.Those
subjectswho
later
became diabetes had at theinitial visit
higher
2-h PG values thandid
theothers (5.7
+
0.5
mM
blood glucose
=102.9-120.8
mg/dl
plasmaglucose).
In
thecurrent
study there were 13 subjectsin
thefirst
degreerelatives of
patientswittr
NIDDM
who had 2-h PG higher than
120.8
mgldl.
Based
on the
finding
of
Warram, those 13
subjects have a greatrisk to
develop
NIDDM.
In this
studyhyperinsulinemia
wasobviously found
in
the first-degree
relatives
of
patient with
NIDDM
be-causetheir fasting
aswell
as2
hours plasma
insulin
were
higher
compared
to control
subjects.
The
sameresult
wasfound
byErickson,s HaffnerT
andWarram.4
As there is no beta
cell dysfunction in
therelatives
with
NGT
and
IGT,
the
presence
of
hyperinsulinemia in
these groups
can
also
be
regarded as a
reflection of
insulin
resistance.2Insulin
resistance
is
defined
as
a
state
of
a
body in
which
greater-than-normal
amountsof insulin
arere-quired
to elicit
aquantitatively
normal
response.This
definition
applies
to
both
insulin-treated diabetic
patients and
to
those individuals
in
whom
glucosetolerance
is normal
or nearnormal
as aresult
of
com-pensatory hyperinsulinemia.
6'9It
is
clear that
insulin
plays
a
greaterrole
and
is
a dependent
factor
in
thedefinition of insulin
resistance
state.In this
study
theinsulin
resistance
was
determined
by
the
method
of
Yalow
and Berson
with
modification. The
ratio of
insulin
and glucose (VG ratio )
wascalculated
insteadof G/I ratio
and wasinterpreted
as thehigher
theratio
the
greater
the insulin resistance.6 The relatives
of
NIDDM
patientswith
normal
glucose tolerance(NGT)
had
higher
plasma glucose
andplasma
insulin
levels
than the control subjects (Figure
4).
The ratios
of
insulin
andglucose consistently
showed that therela-tives
of
NIDDM
patients had
higher VG ratio which
meant they
neededmore
insulin
to maintain
anormal
glucose
level.
So
it
may
be presumedthat
this
group
has
insulin
resistance.The
relatives of
NIDDM
patientswith NGT
had 2hour
plasma
insulin
andplasma glucose levels higher
thanin
the control
subjects (Figure
4). As
the
plasmaglucose
levels
were
nearly
equal
after
glucoseinges-tion
in
both
groups,
while the
resultant
insulin
con-centrations
were
greater
in
the relatives
of
NIDDM
patients
with NGT
then according to thedefinition
this
group was
presumed
to
have insulin
resistance.
By
linear regression
analysisthis
insulin
resistancecould
be
quantified
(Figure
2).Metabolic Defects in Diabetic Offspring 101
insulin (mUÂ) glucose (mgidl)
1Â
Fedng FaCtng Two l{our T\,vo hout
[image:5.595.301.544.89.288.2]lnarlin qucoæ lnslin Glucæ
Figure
4.
The comparison offasting
and 2-hour plasma insulin,fasting
and 2-hour plasma glucosein
relativesof
NIDDM patients with normal glucose tolerance and in control
subjects.
Various
methods
of
measuring
insulin
action
in-vivo
have been proposed.
In this
study theinsulin
resistancewas determined
indirectly
by
using
the
modified
Yalow-Berson method
andlinear regression
analysis. Thegold
standardfor insulin
resistancedetermination
is
euglycemic clamp
technique
in
which insulin
isinfused systemically and plasma
glucose
is
main-tained
constant
by
exogenous glucose infusion.
Glucose
is
clamped at euglycemia
level.
Glucose
in-fusion
rate equals sumof
decreasein
hepatic
glucoserelease and increase
in
glucose uptake.rJ
By
this
method,
Ndraha found higher
insulin
resistancein
theoverweight
IndonesianNIDDM
subjects and there was asignificant
correlation between
BMI
andfasting
in-sulii
Ievel.14In
summary,
this
study shows that
IGT,
hyperin-sulinemia and
insulin
resistance are
important
early
metabolic
defects
among
first-degree
relatives
of
patients
with
NIDDM
in
Indonesia. Those
IGT
sub-jects and the relatives
with NGT who
have
2h-PG
higher than
120.8
mg/dl
are
at
increased
risk
of
developing
diabetes andshould
haveNIDDM
preven-tion program
to decreaseinsulin
resistance, topromote
and sustain pancreatic beta
cell
function
(e.g.
by
programs
of
obesity reduction
and
the promotion
of
physical
activity).'
ACKNO\ryLEDGMENTS
Immunoendocrinology Laboratory
School
of
Medicine, University
of
Indonesia
for
doing
in-sulin
assays;Dr.
Diana, Dewi,
Ventje,
Sugeng
and nursesfor collecting blood
samples andinviting
studyfamilies.
Special
thanks are extended
to
Dr.
SuzannaNdraha
who has
played a key role
in
development
of
idea, generate data,doing statistical
analysis and secretarialworks.
REFERENCES
l.
Preventionof
Diabetes Mellitus. Reportof WHO
study group.WHO
Technical Report Series,No' 844; Geneva,1994.
2. Weir GC, Leahy JL. Pathogenesis of non-insulin-dependent
(type
II)
diabetes mellitus.In
Kahn CR,Weir
GC' eds.Joslin's Diabetes mellitus. l3th ed. Philadelphia' Lea and
Febiger 1994;240-64.
3.
Martin BC, Warm JH,
KroleswskiAS,
Bergman RN,Steldnes JS, Kahn CR. Role of glucose and insulin resistance
in development of type
II
diabetes mellitus: results of a 25year follow up study. Larcet 1992;340:925-9.
4. Warram JH, Martin BC, Krolewski AS, Steldnes JS, Kahn
CR. Slow
glucose removal rate and hyperinsulinemiaprecede the development of type
II
diabetes in the offspringof diabetic parents. Ann Intern Med 1990;l l3:909-15. 5. Eriksson J, Fransila-Kalkenki A, Estrand A. Early metabolic
defects in persons at increased risk for
non-insulin-depend-ent diabetes mellitus. N Engl J Med 1989; 321,,337-43.
Med J Indones
6. Berson SA, Yallow RS.
Insulin
'antagonist' and insulinresistance. In: Ellenberg
M,
RifkinH
(eds). Diabetesmel-litus: Theory and Practice. New York:
McGraw-Hill'
1970;388-423.
7. Yallow RS, Berson SA. Irnmunoassay of endogenous
plas-ma insulin in man. J Clin Invest 1960; 39:l157-75.
8. Tsu
TT,
Herzenberg LA. Solid phase Radioimmune assays.In: Mishell BB, Shiigi SM (eds). Selected Methods in Cel-lular Immunology. San Fransisco : Freeman and Co, 1980;
373-97.
9. Flier JS. An Overview of Insulin Resistance. In: Moller DE'
Insulin Resistance. Chichester: John Willey and Sons, 1993;
t-'t.
10. Charles MA, Fontbonne A, Thibult N, Warnet JM, Rosselin
GE, Eschwege E. Risk factors for NIDDM in white
popula-tion. Paris Prospective Study. Diabetes 1991;40:996-9.
I 1. Haffner SM, Stern MP, Hazuda HP, Pugh JA, Patterson JK. Hyperinsulinemia
in
a population at high risk fornon-in-sulin-dependent diabetes
mellitus.
N
Engl J
Med1986;315:220-4.
12. Saad MF, Knowler WC, Pettitt DJ, Nelson RG, Mott
DM'
Bennett
PH. The
naturalhistory
of
impaired glucose tolerancein
the
Pima Indians.N
Engl
J
Med
1988; 319:1500-6.13. De Fronzo RA, Tobin JD, Andres R. Glucose Clamp Tech-nique: a method for qualifying insulin secretion and
resis-tance. Am J Physiol 1979;273:8214-23.
14. Ndraha S, Soewondo P, Suyono S. Resistensi insulin pada
diabetes melitus tidak tergantung insulin berat badan lebih.
Paper akhir Program Studi Spesialis bidang Ilmu Penyakit