Maldives 2017
Acronyms
AD Auto disable
AEFI Adverse events following immunization
AFP Acute flaccid paralysis
BCG Bacillus Calmette-Guérin vaccine
CES Coverage evaluation survey
cMYP Comprehensive multi-year plan
CRS Congenital rubella syndrome
DHS Demographic health survey
DT Diphtheria tetanus toxoid, pediatric
DTP Diphtheria – tetanus – pertussis vaccine
DTP-Hib-HepB Pentavalent vaccine
DTP-Hib-HepB3 3rd dose pentavalent vaccine
EPI Expanded programme on immunization
GDP Gross domestic product
HCW Health care worker
HepB Hepatitis B vaccine
Hib Haemophilus influenzae type b
HPV Human papilloma virus
IgM Immunoglobulin M
IPV Inactivated poliovirus vaccine
JE Japanese encephalitis
JE_Live-Atd JE live attenuated vaccine
JRF WHO UNICEF joint reporting form
LB Live birth
M Measles
MCV1 First dose measles containing vaccine
MCV2 Second dose measles containing vaccine
MICS Multiple indicator cluster survey
MMR Measles mumps rubella vaccine
MNT Maternal and neonatal tetanus
MR Measles rubella vaccine
NCIP National committee on immunization practices
NID National immunization day
NTAGI National technical advisory group on immunization
NPEV Non-polio enterovirus
NT Neonatal tetanus
OPV Oral poliovirus vaccine
bOPV Bivalent OPV
tOPV Trivalent OPV
PCV Pneumococcal conjugate vaccine
SEAR WHO South-East Asia Region
SIA Supplementary immunization activities
SNID Subnational immunization day
Td Tetanus diphtheria toxoid; older children, adults
TT Tetanus toxoid
TT2+ 2 or more doses TT
VDPV Vaccine derived poliovirus
VPD Vaccine preventable diseases
WCBA Women of child bearing age
Contents
Impact of rouine immunizaion
Page
No.
EPI history 5
Basic informaion 2016 Table 1 5
Immunizaion schedule 2016 Table 2 5
Naional immunizaion coverage 1980 - 2016 Figure 1 6
Immunizaion system highlights Table 3 6
DTP3 coverage, diphtheria and pertussis cases 1980 - 2016 Figure 2 7 Reported cases of vaccine preventable diseases 2011 - 2016 Table 4 7
DTP-Hib-HepB3 coverage by district 2015 Figure 3 7
DTP-Hib-HepB3 coverage by district 2016 Figure 4 7
Towards measles eliminaion and rubella/congenital rubella
syndrome control
Page
No.
MCV1 and MCV2 coverage, measles and rubella cases, 1980-2016 Figure 7 11
MCV supplementary immunizaion aciviies Table 7 11
MCV1 coverage by district 2015 Figure 8 12
MCV1 coverage by district 2016 Figure 9 12
MCV2 coverage by district 2015 Figure 10 12
MCV1 coverage by district 2016 Figure 11 12
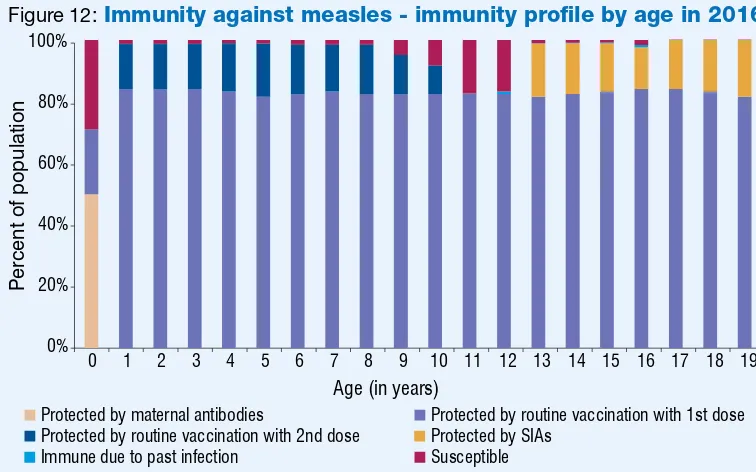
Immunity against measles – immunity proile by age in 2016 Figure 12 12 Subnaional risk assessment for measles and rubella Figure 13 12 Sporadic and outbreak associated measles cases by month 2011 - 2016 Figure 14 13 Immunizaion status of conirmed (laboratory and Epi linked) measles outbreak
associated cases by age 2011 – 2016 Figure 15 13
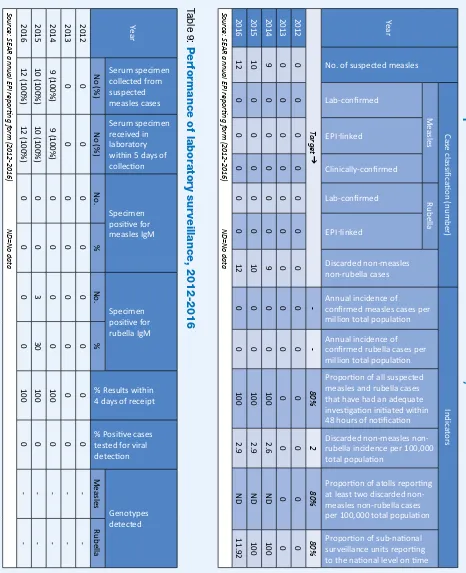
Quality of ield and laboratory surveillance for measles and rubella 2012 - 2016 Table 8 14
Performance of laboratory surveillance 2012 - 2016 Table 9 14
WHO supported laboratory network for VPD surveillance Figure 16 15
Maternal and neonatal tetanus eliminaion is sustained
Page
No.
TT2+ coverage and NT cases 1980 - 2016 Figure 5 8
Polio-free status is maintained
Page
No.
AFP surveillance indicators 2011 - 2016 Table 5 9
AFP cases 2011-2016 Figure 6 9
Maldives: atoll level map
WHO South-East Asia Region
EPI history
• EPI launched in 1976
• HepB vaccine introduced in 1993 • MMR vaccine introduced in 2007 • DTP-Hib-HepB vaccine started at
naional level in 2013
• TT vaccine replaced by Td vaccine in 2015
• IPV introduced in 2015 • tOPV to bOPV switched on
18 April 2016.
Source: cMYP 2016-2020 and EPI/MOH
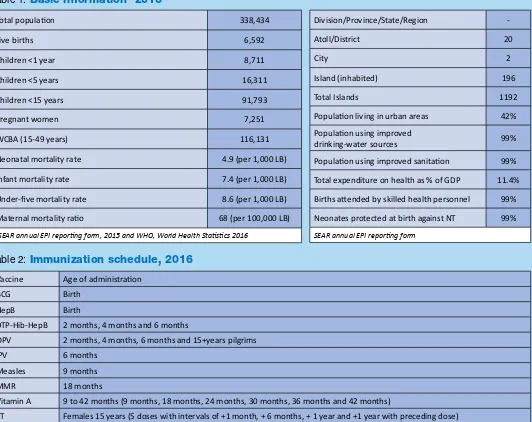
Table 1:
Basic information
12016
Total populaion 338,434
Live births 6,592
Children <1 year 8,711
Children <5 years 16,311
Children <15 years 91,793
Pregnant women 7,251
WCBA (15-49 years) 116,131
Neonatal mortality rate 4.9 (per 1,000 LB)
Infant mortality rate 7.4 (per 1,000 LB)
Under-ive mortality rate 8.6 (per 1,000 LB)
Maternal mortality raio 68 (per 100,000 LB)
1SEAR annual EPI reporing form, 2015 and WHO, World Health Staisics 2016
Division/Province/State/Region
-Atoll/District 20
City 2
Island (inhabited) 196
Total Islands 1192
Populaion living in urban areas 42% Populaion using improved
drinking-water sources 99%
Populaion using improved sanitaion 99% Total expenditure on health as % of GDP 11.4% Births atended by skilled health personnel 99% Neonates protected at birth against NT 99% SEAR annual EPI reporing form
Table 2:
Immunization schedule, 2016
Vaccine Age of administraionBCG Birth
HepB Birth
DTP-Hib-HepB 2 months, 4 months and 6 months
OPV 2 months, 4 months, 6 months and 15+years pilgrims
IPV 6 months
Measles 9 months
MMR 18 months
Vitamin A 9 to 42 months (9 months, 18 months, 24 months, 30 months, 36 months and 42 months)
TT Females 15 years (5 doses with intervals of +1 month, + 6 months, + 1 year and +1 year with preceding dose) Source: WHO/UNICEF JRF, 2016
Table 3:
Immunization system highlights
cMYP for immunizaion 2016-2020
MTAGI fully funcional
Spending on vaccines inanced by the government 100%
Spending on rouine immunizaion programme inanced by the government 72% Updated micro-plans that include aciviies to improve immunizaion coverage 20 atolls (100%) Naional policy for health care waste management including waste from immunizaion aciviies in place
Naional system to monitor AEFI in place
Most recent EPI CES DHS ongoing
>80% coverage for DTP-Hib-HepB3 20 atolls (100%)
>90% coverage for MCV1 20 atolls (100%)
>10% drop-out rate for DTP-Hib-HepB1 to DTP-Hib-HepB3 no district
Source: WHO/UNICEF JRF, 2016
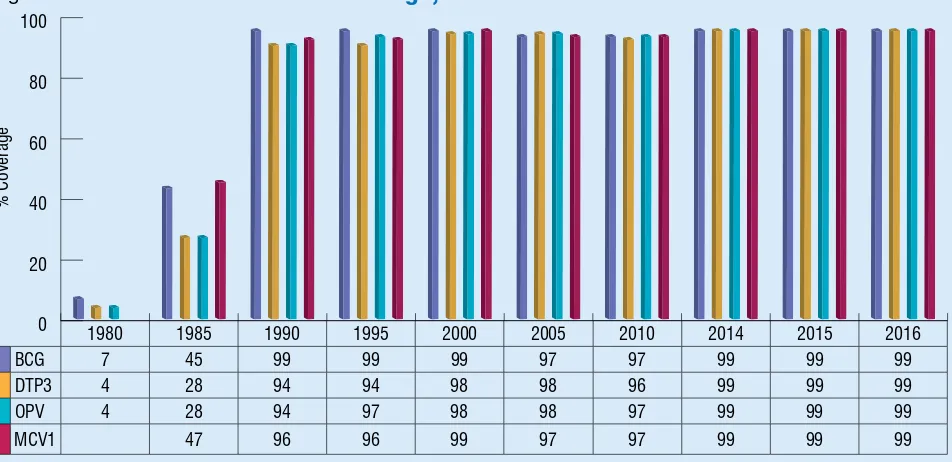
Figure 1:
National immunization coverage, 1980-2016
Source: WHO/UNICEF esimates of naional immunizaion coverage, July 2017 revision
% Coverage
1980 1985 1990 1995 2000 2005 2010 2014 2015 2016
BCG 7 45 99 99 99 97 97 99 99 99
DTP3 4 28 94 94 98 98 96 99 99 99
OPV 4 28 94 97 98 98 97 99 99 99
MCV1 47 96 96 99 97 97 99 99 99
Figure 3:
2015
Figure 4:
2016
Source: SEAR annual EPI reporing form, 2015 (administraive data)Source: SEAR annual EPI reporing form, 2016 (administraive data)
Figure 2:
DTP3 coverage
1, diphtheria and pertussis cases
2, 1980-2016
Year
Diphtheria Cases Pertussis Cases DTP3 Coverage
%
1WHO/UNICEF esimates of naional immunizaion coverage, July 2017 revision 2WHO vaccine-preventable diseases: monitoring system 2016
Table 4:
Reported cases of vaccine preventable diseases, 2011-2016
Year Polio Diphtheria Pertussis NT
(% of all Tetanus) Measles Rubella Mumps JE CRS
2011 0 0 0 0 0 0 69 0 0
Source: WHO/UNICEF JRF ND=No data
DTP-Hib-HepB3 coverage by district
1980 1985 1990 1995 2000 2005 2010 2011 2012 2013 2014 2015 2016
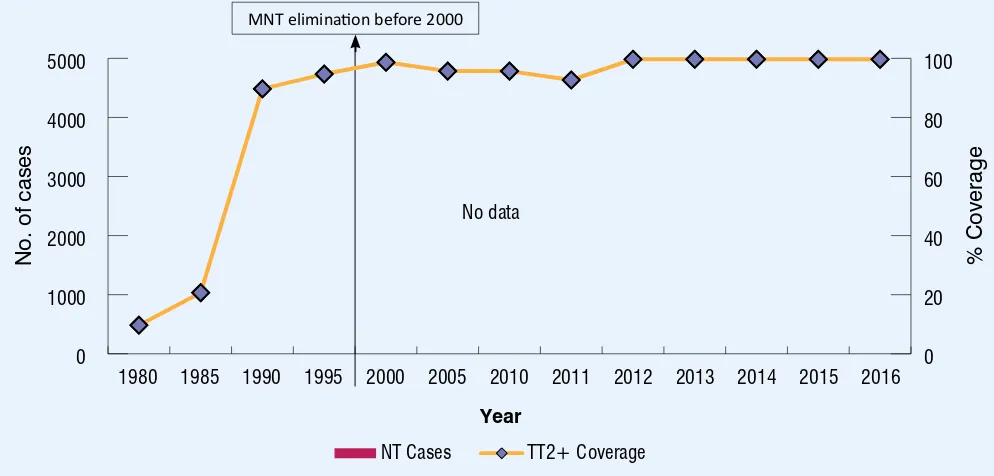
NT Cases TT2+ Coverage
No data
1 WHO/UNICEF JRF, Country oicial esimates, 1980-2016 2WHO vaccine-preventable diseases: monitoring system 2016
Maternal and
neonatal tetanus elimination is sustained
MNT eliminaion before 2000
Table 5:
AFP surveillance performance indicators, 2011-2016
Indicator 2011 2012 2013 2014 2015 2016
AFP cases 3 4 1 1 5 2
Wild poliovirus conirmed cases 0 0 0 0 0 0
Compaible cases 0 0 0 0 0 0
Non-polio AFP rate1 3.40 4.55 1.08 1.12 5.60 2.11
Adequate stool specimen collecion percentage2 33% 75% 100% 100% 60% 0%
Total stool samples collected 2 6 2 2 6 4
% NPEV isolaion 0 0 0 0 0 0
% Timeliness of primary result reported3 0 100 100 100 0 100
1Number of discarded AFP cases per 100,000 children under 15 years of age.
2Percent with 2 specimens, at least 24 hours apart and within 14 days of paralysis onset. 3Results reported within 14 days of sample received at laboratory.
Polio-free
status is maintained
Last laboratory-conirmed polio case due to WPV was reported in 1994.
Figure 6:
AFP cases 2011-2016
2011 = 3 cases 2012 = 4 cases 2013 = 1 case 2014 = 1 case 2015 = 5 cases 2016 = 2 cases
Table 6:
OPV SIAs
Year Anigen Geographic
coverage Target age
Target populaion Coverage (%)
Round 1 Round 2 Round 1 Round 2
1997 OPV NID <5 years 40,000 43 40
1998 OPV NID <5 years 39,000 41 44
1999 OPV NID <5 years 38,000 47 50
2000 OPV NID <5 years 37,500 53 53
2001 OPV SNID <5 years 35,000 101 29
Source: NCCPE report and WHO/UNICEF JRF
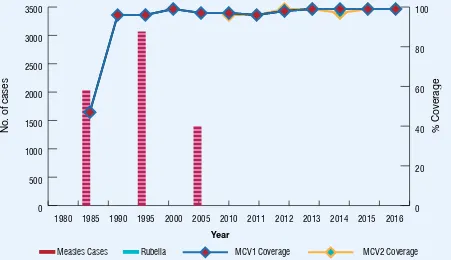
Towards
measles elimination and rubella/CRS control
Figure 7:
MCV1 and MCV2 coverage
1, measles and rubella cases
2, 1980-2016
Measles Cases Rubella MCV1 Coverage MCV2 Coverage 2016
No. of cases
Year
1WHO/UNICEF esimates of naional immunizaion coverage, July 2017 revision 2WHO vaccine-preventable diseases: monitoring system 2016
Table 7:
MCV SIAs
Year Anigen Geographiccoverage Target group Target
Coverage %
2005 MR 2 districts 6 to 25 years (males) and 6 to 35 years (females) 144,997 82
2006 MR naionwide 6 to 25 years (males) and 6 to 35 years (females) 144,997 85
2007 MMR naionwide 4 to 6 years 29,529 56
Source: WHO/UNICEF JRF (muliple years)
Figure 9:
2016
Figure 10:
2015
Figure 11 :
2016
Source: SEAR annual EPI reporing form, 2016 (administraive data) Source: SEAR annual EPI reporing form, 2016 (administraive data)
Figure 8:
2015
Source: SEAR annual EPI reporing form, 2015 (administraive data)
Source: SEAR annual EPI reporing form, 2015 (administraive data)
MCV1 coverage by district
0% 20% 40% 60% 80% 100%
0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19
Percent of population
Age (in years)
Protected by maternal antibodies Protected by routine vaccination with 1st dose Protected by routine vaccination with 2nd dose Protected by SIAs
Immune due to past infection Susceptible
Figure 12:
Immunity against measles - immunity profile by age in 2016*
* Modeled using MSP tool ver 2 assuming the schedule and MCV coverage remain unchanged and no SIAs in 2015 & 2016.
Figure 13:
Sub-national risk assessment - measles
and rubella 2016
Source: developed using WHO risk assessment tool based on JRF & ARF data base
Figure 14:
Sporadic and outbreak associated measles cases* by month 2011-2016
Outbreak associated measles
No of cases
*Includes laboratory conirmed and epidemiologically linked cases Source: SEAR Monthly VPD reports
Figure 15:
Immunization status of confirmed (laboratory and EPI linked) measles
outbreak associated cases, by age, 2011-2016
> 15 years
10-14 years
5-9 years
1-4 years
< 1 year
> 15 years
10-14 years
5-9 years
1-4 years
< 1 year
> 15 years
10-14 years
5-9 years
1-4 years
< 1 year
> 15 years
10-14 years
5-9 years
1-4 years
< 1 year
> 15 years
10-14 years
5-9 years
1-4 years
< 1 year
> 15 years
10-14 years
5-9 years
1-4 years
< 1 year
2011 2012 2013 2014 2015 2016
Immunized Not immunized/ unknown
0
No outbreak reported No outbreak reported
Table 8:
Surveillance performance indicators for measles and rubella, 2012-2016
Year
No. of suspected measles
Case classiic
Discarded non-measles non-rubella cases
Annual incidence of conirmed measles cases per million total populaion
Annual incidence of conirmed rubella cases per million total populaion Proporion of all suspected measles and rubella cases that have had an adequate invesigaion iniiated within 48 hours of noiicaion
Discarded measles non-rubella incidence per 100,000 total populaion
Proporion of atolls reporing at least two discarded non-measles non-rubella cases per 100,000 total populaion
Proporion of sub-naional surveillance units reporing to the naional level on ime Lab-conirmed
AR annual EPI reporing f
orm (2012-2016)
ND=No dat
a
Year
Serum specimen collected from suspected measles cases
Serum specimen received in laboratory within 5 days of collecion
Specimen posiive for measles IgM
Specimen posiive for rubella IgM
% Results within 4 days of receipt
% Posiive cases tested for viral detecion
AR annual EPI reporing f
orm (2012-2016)
ND=No dat
a
Table 9:
Performance of laboratory surveillance, 2012-2016
Figure 16:
WHO supported laboratory network for VPD surveillance
Source EPI Maldives, May 2015
For contact or feedback:
Naional Programme on Immunizaion and Travel Health
Health Protecion Agency, Ministry of Health, Male, Maldives Phone: +960-3014495, Fax : +960-3014484
Email: nash@health.gov.mv, nash3118@gmail.com, www.health.gov.mv
Immunizaion and Vaccine Development (IVD)
WHO-SEARO, IP Estate, MG Marg, New Delhi 110002, India Tel: +91 11 23370804, Fax: +91 11 23370251
Email: SearEpidata@who.int