Role of physiological state ‘normothermia’ in internal thoracic
artery spasm after harvesting
Arif Tarhan
a,*
, Tamer Kehlibar
a, Fikri Yapıcı
a, Mehmet Yılmaz
a,
Yucesin Arslan
a, Nihan Yapıcı
b, Azmi O
¨zler
aa
Department of Cardiovascular Surgery, Dr Siyami Ersek Thoracic and Cardiovascular Surgery Education and Research Hospital, Istanbul, Turkey
b
Department of Anesthesiology, Dr Siyami Ersek Thoracic and Cardiovascular Surgery Education and Research Hospital, Istanbul, Turkey
Received 5 June 2006; received in revised form 31 August 2006; accepted 1 September 2006
Abstract
Objective:Vasospasm is often faced after the operative preparation of internal thoracic artery. Different vasodilating pharmacological agents are being used to eliminate this problem. During the preparation of internal thoracic artery, normal, local, and systemic temperatures are lost. We aimed to find out the effect of this decrease in temperature on the free flow of internal thoracic artery.Methods:We investigated the effects of normal saline solution at 208C (group I), papaverine at 208C (group II) and normal saline solution at 378C (group III). Each group contained 20 patients undergoing coronary bypass. Free flow of the left internal thoracic artery was measured after mobilization. After approximately 18 min the graft had been sprayed with one of the agents, and the second free flow was measured (t-interval was 18.22.1 for group I, 18.31.8 for group II, and 17.51.9 for group III).Results:Normal saline solution at 208C did not cause a significant change. Topical papaverine at 208C increased the flow from 42.110.7 ml/min to 77.517.9 ml/min (p<0.0001). A significant increase also occurred with normal saline solution
at 378C from 4111.9 ml/min to 75.318.9 ml/min (p<0.0001).Conclusions: After harvesting the graft, regaining physiological nor-mothermic state is enough for vasodilatation. Even using one of the most potent vasodilating agent papaverine at 208C is not superior to normothermia.
#2006 Elsevier B.V. All rights reserved.
Keywords: Coronary artery bypass grafts; Internal thoracic artery; Hypothermia; Normothermia; Vasospasm
1. Introduction
Internal thoracic artery (ITA) is accepted as the gold standard for graft choice in coronary bypass surgery because of high patency rates[1,2]. Vasospasm causing reduction in ITA flow is a problem that can be faced after operative harvesting of the graft. ITA spasm may contribute to myocardial ischemia and early postoperative morbidity and mortality [3]. Different factors have been accused for vasospasm[4]. Mechanical trauma and thermal injury during harvesting of the graft are the major factors that are thought to be responsible. Various vasodilator agents have been used to eliminate this problem since the first days ITA was used in coronary bypass surgery.
In their study, Bilgen et al.[5]searched the effect of a potent vasodilator papaverine potentiated by normothermia. Since in normothermia the changing biochemical feature of papaverine potentials the vasodilator effect, we believed
that searching the presence of specific effect of normother-mia is required to obtain a scientifically accurate result. On the basis of this opinion, we aimed in our study to test the specific effect of normothermia itself on vasospasm and ITA flow and compare it with the effect of papaverine.
2. Materials and methods
Sixty consecutive coronary ischemic patients whose left internal thoracic arteries were used as a conduit for myocardial revascularization were randomly assigned to three groups: (n= 20, group I) patients with the effects of topically performed normal saline solution at the operating room temperature (208C), (n= 20, group II) papaverine at the operating room temperature and (n= 20, group III) normal saline solution at normothermic body temperature (378C).
Patients who had one of the following criteria: age over 70 years (n= 10), peripheral arterial disease (n= 2), chronic renal disease (n= 1), diabetes mellitus (n= 12), low cardiac ejection fraction (n= 4), peroperatory vasoactive agent utilization (n= 7), combined diabetes mellitus with overage patients (n= 2), combined diabetes mellitus with peripheral arterial www.elsevier.com/locate/ejcts European Journal of Cardio-thoracic Surgery 30 (2006) 749—752
* Corresponding author. Address: Hızırbey Caddesi Nesrin Sokak No:1 D:11 Go¨ztepe, Istanbul 81060, Turkey. Tel.: +90 216 3499120 (Business)/90 216 5650699 (Home); fax: +90 216 5652130.
E-mail address:atarhan@gmail.com(A. Tarhan).
disease (n= 3) were not included in the study. A total of 41 patients were excluded among 101 patients, therefore 60 consecutive patients were found suitable for this study.
Surgical technique: ITA was harvested by the same surgeon as a pedicled graft from the subclavian artery to the bifurcation into the superior epigastric and muscular phrenic arteries. During harvesting low diathermy 15 mA (milli Ampere) and metal ligature clips were used. Five minutes after systemic heparin treatment ITA was divided distally. The first flow was measured. The graft was sprayed topically with one of the solutions of normal saline solution at the operating room temperature (208C, group I), papaverine at the operating room temperature (208C, group II) and normal saline solution at 378C (group III). ITA was wrapped into a swab soaked with normal saline solution at 378C in the normothermic group (group III) or with the same solution at room temperature in hypothermic groups (group I and group II). Swab pack was kept inside the left thorax during procedure. The swab was sprayed with the same solution as it was soaked in every 2 min periodically. After a median of 18 min, the second free flow was measured (meanSD levels were shown inTable 1).
Flows were determined by measuring the volume of blood expelled from the end of the bleeding artery in a 30 s period. After first measuring, the bleeding end of the artery was occluded with a bulldog clamp.
The topical solutions consisted of the following: group I: 4 ml of 0.9% sodium chloride solution at the operating room temperature (208C), group II: 6 mg papaverine in 4 ml of 0.9% sodium chloride solution at the operating room temperature (208C), group III: 4 ml of 0.9% sodium chloride solution at 378C (normothermic core temperature).
Patients who needed vasopressing or vasodilating agents during the operation were excluded. At the two stages, the free flows were measured; time, mean arterial pressure, esophageal temperature, local temperature, heart rate and central venous pressure values were also recorded. Local temperature was measured from the areolar tissue around ITA using a myocardial temperature probe (De Royal, REF 81-030418). A general-purpose temperature probe (De Royal, REF 81-020409) was used for measuring esophageal tem-perature.
All statistical procedures were performed using the program GraphPad InStat Version 2.02 (GraphPad Software Inc., San Diego, CA) for DOS. All values are expressed as meanstandard deviation. For comparing the repeated flow, mean arterial pressure, esophageal temperature, local temperature, heart rate, central venous pressure measures in each group, pairedt-test was used. The comparison of the measurements between the groups was made by one way analysis of variance and Tukey’s multicomparison tests. Ap -value of less than 0.05 was considered significant.
3. Results
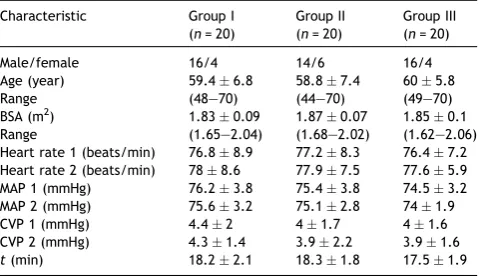
Clinical characteristics and hemodynamic data of the patients are shown in Table 1. There is no significant difference between body surface areas and ages of the three groups. When heart rate, mean arterial pressure and central venous pressures as the signs of low cardiac output and hypovolemia were compared, there was no statistically significant difference within and between the groups.
Table 2 shows esophageal and local temperature
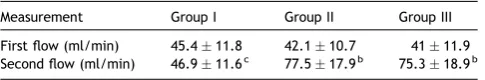
mea-surements. Esophageal temperature measurements at the same stages were not significantly different. Second esophageal temperatures remained almost unchanged, over 358C in all groups and were not different from the first esophageal temperatures. First local temperatures were nearly the same in the three groups. While second local temperatures decreased significantly in the first two groups, from 31.080.88C to 28.340.78C and from 30.980.98C to 27.950.58C, whereas it showed a significant increase from 31.090.98C to 33.220.88C in group III. This increased second local temperature of group III was also significantly different from that of the first two groups which decreased to 288C. The first flows of the groups showed no significant difference. Topical papaverine increased the flow from 42.110.7 ml/min to 77.517.9 ml/min (p<0.0001) in group II while
nor-mothermic saline solution provided an increase from 4111.9 ml/min to 75.318.9 ml/min (p<0.0001) in
group III. In the control group (group I), saline at the operating room temperature didn’t cause a significant change in the second flow. The increased second flows of group II and III were significantly different from the second flow of group I (p<0.001). Group II second flow 77.517.9b
was not significantly different from group III second flow 75.318.9 (Table 3).
A. Tarhan et al. / European Journal of Cardio-thoracic Surgery 30 (2006) 749—752
750
Table 1
Clinical characteristics and hemodynamic data of the patientsa
Characteristic Group I BSA: body surface area; CVP: central venous pressure; MAP: mean arterial pressure;t: time period between first and second measures.
a Data are presented as mean
standard deviation except sex ratios.
Table 2
Esophageal and local temperature measurementsa
Measurement Group I Group II Group III
First esophageal Second local temperature (8C) 28.340.7b 27.95
0.5b 33.22 0.8b, c a Data are presented as mean
standard deviation.
b p<0.0001 versus first local temperature within each group. c
4. Discussion
In coronary bypass surgery, ITA vasospasm is an unwanted state as it reduces ITA flow leading to perioperative morbidity and mortality [3]. It is a result of a multifactorial combination. Hypothermia is among these factors[4]. This is the first in vivo study that has searched the effect of core and local temperatures on ITA free flow.
To prevent and overcome spasm different pharmacologic agents with different methods have been used[4]. Green[6], the pioneer of ITA graft surgery, recommended injecting papaverine into the graft. Since then topical, intraluminal or intravenous antispasmoic protocols have been improved. Papaverine is one of the most studied vasodilating agents. Bilgen et al. [5] showed that topical papaverine at 378C produce more increase in free ITA flow than papaverine at 208C. They emphasized that enzyme activity induced at 378C results in more relaxation. Erdinc and Ocal[7]stated that the effect of hypothermia, which might cause a delayed vasorelaxation was missing in Bilgen’s study. They suggested that it could be tested by another group in which saline solution at 378C is performed. On the basis of these critics, we designed this study aiming to find out the specific effect of normothermia on vasospasm and ITA flow. We followed Bilgen’s method and added a normothermic saline group instead a normothermic papaverine group. We recorded esophageal and local temperatures. In group III in which normal saline solution at 378C was performed, free flow increased from 4111.9 ml/min to 75.318.9 ml/min (p<0.0001) (Table 3) parallel to the significant increase
in local temperature from 31.090.98C to 33.220.88C
(Table 2). In the control group and papaverine at 208C
performed group the second local temperatures decreased significantly after a while (t: 18.22.1 min). The signifi-cantly increased second flows by papaverine in group II and by normothermia in group III were also significantly higher than that of the control group. Group II’s second flow 77.517.9b
was nonsignificant from group III’s second flow 75.318.9. When 95% confidence interval (CI) was computed, for second flow difference normothermic group versus 208C papaverine group, we had the values as mean difference = 2.200, lower 95% CI = 14.729 and upper 95% CI = 10.329. These flow changes are not clinically relevant and the difference can be excluded.
In moderate environments, peripheral compartment temperature is usually 2—48C less than the core tempera-ture. This difference increases in extreme thermal and physiological conditions [8]. Vasoconstriction to store the metabolic heat in the core increases the temperature gradient between the core and periphery. Even the operation field cannot be termed as periphery as the chest is open since
sternotomy is available for heat loss. In our study, whereas the esophageal temperatures were saved at above 358C, local temperatures decreased significantly to around 288C in hypothermic groups.
There are different experimental studies on factors augmenting vasospasm by cooling[9—11]. Although there is a differential modulation of responses to exogenous norepinephrine in superficial and deep circulation with moderate cooling, the cooling-induced augmentation of contractile responses to sympathetic nerve stimulation was observed[12,13]. Norepinephrine (NE) release is both nitric oxide (NO)-dependent and nitric oxide-independent.[14]
The NO-dependent mechanism is more sensitive to cooling. The decreased production of NO at 248C may explain a greater neurogenic vasoconstriction induced by NE and other potential constrictor transmitters at 248C than at 378C.
Mostly used topical application methods were perivas-cular tissue injection, topical spraying and intraluminal application. Intravascular application is not preferable because of its side effects and complication potential[15— 18]. Moreover, the two ways were preferred by authors because of application safety. We believe by preserving the physiological normothermic state during preparation of ITA there would be less need to use an extra pharmacological solution. Without using any extra pharmacological agent, the probable side effects would be prevented.
As a conclusion, after harvesting the graft, regaining physiological normothermic state is sufficient for appropriate vasodilatation. Even using one of the most potent vasodilator papaverine at 208C is not superior to normothermia.
References
[1] Lytle BW, Loop FD, Cosgrove DM, Ratliff NB, Easley K, Taylor PC. Long term (5—12 years) serial studies of internal mammary artery and saphe-nous vein coronary bypass grafts. J Thorac Cardiovasc Surg 1985;89: 248—58.
[2] Loop FD, Lytle BW, Cosgrove DM, Stewart RW, Goormastic M, Williams GW, Golding LA, Gill CC, Taylor PC, Sheldon WC. Influence of the internal mammary artery graft on 10 year survival and other cardiac events. N Engl J Med 1986;314:1—6.
[3] Jones EL, Lattouf OM, Weintraub WS. Catastrophic consequences of internal mammary hypoperfusion. J Thorac Cardiovasc Surg 1989;98: 902—7.
[4] Rosenfeldt FL, He GW, Buxton BF, Angus JA. Pharmacology of coronary artery bypass grafts. Ann Thorac Surg 1999;67:878—88.
[5] Bilgen F, Yapıcı MF, erbetc¸iog˘lu A, Tarhan A, C¸oruh T, O¨zler A. Effect of normothermic papaverine to relieve intraoperative spasm of the internal thoracic artery. Ann Thorac Surg 1996;62:769—71.
[6] Green GE. Rate of blood flow from the internal mammary artery. Surgery 1971;70:809—13.
[7] Erdinc M, Ocal A. Internal thoracic artery spasm and normothermic papaverine. To the editor. Ann Thorac Surg 1997;64:1219—20. [8] Sessler DI. Perioperative heat balance. Anesthesiology 2000;92:578—96. [9] Harker CT, Taylor Jr LM, Porter JM. Vascular contractions to serotonin are
augmented by cooling. J Cardiovasc Pharmacol 1991;18:791—6. [10] Harker CT, Vanhoutte PM. Cooling the central ear artery of the rabbit:
myogenic and adrenergic responses. J Pharmacol Exp Ther 1988;245: 89—93.
[11] Harker CT, Ousley PJ, Bowman CJ, Porter JM. Cooling augmentsa2
-adrenoceptor-mediated contractions in rat tail artery. Am J Physiol 1991;260:H1166—71.
[12] Flavahan NA, Lindblad LE, Verbeuren TJ, Shepherd JT, Vanhoutte PM. Cooling anda1-anda2-adrenergic responses in cutaneous veins: role of
receptor reserve. Am J Physiol 1985;249:H950—5.
A. Tarhan et al. / European Journal of Cardio-thoracic Surgery 30 (2006) 749—752 751
Table 3
Flow measurementsa
Measurement Group I Group II Group III
First flow (ml/min) 45.411.8 42.110.7 4111.9 Second flow (ml/min) 46.911.6c 77.5
17.9b 75.3 18.9b a Data are presented as mean
standard deviation.
b
p<0.0001 versus first flow within each group.
[13] Yamamoto R, Cline Jr WH, Takasaki K. Effect of moderate cooling endogenous norepinephrine release from the mesenteric vasculature of rats. J Auton Pharmacol 1989;9:347—55.
[14] Yamamoto R, Wada A, Asada Y, Yanagita T, Yuhi T, Niina H, Sumiyoshi A, Kobayashi H, Lee TJ. Nitric oxide-dependent and -independent nore-pinephrine release in rat mesenteric arteries. Am J Physiol 1997;272: H207—10.
[15] Dipp MA, Nye PCG, Taggart DP. Phenoxybenzamine is more effective and less harmful than papaverine in the prevention of radial artery vasos-pasm. Eur J Cardiothorac Surg 2001;19:482—6.
[16] Van Son JAM, Tavilla G, Noyez L. Detrimental squeal on the wall of the internal mammary artery caused by hydrostatic dilation with diluted papaverine solution. J Thorac Cardiovasc Surg 1992;104:972—6. [17] Cooper GJ, Wilkinson GA, Angelini GD. Overcoming perioperative spasm
of the internal mammary artery: which is the best vasodilator? J Thorac Cardiovasc Surg 1994;108(2):387.
[18] Formica F, Ferro O, Brustia M, Corti F, Colagrande L, Bosisio E, Paolini G. Effects of papaverine and glycerylnitrate-verapamil solution as topical and intraluminal vasodilators for internal thoracic artery. Ann Thorac Surg 2006;81(1):120—4.
A. Tarhan et al. / European Journal of Cardio-thoracic Surgery 30 (2006) 749—752