CURRICULUM
Aims:
To assess growth and development in children and adolescents.
To diagnose, manage, and refer if required, common disorders of growth and development.
Awareness of the general means to assess fetal growth (intrauterine growth).
Awareness of the common health implications of normal and abnormal aging.
Learning outcomes:
Assess physical growth of children and adolescents.
Diagnose and manage common nutritional problems in children and adolescents.
Investigate infant or child with suspect failure to thrive.
Identify common congenital anomalies in infants and children.
Assess fetal growth (intrauterine growth).
Assess development of children in specific domains.
Awareness of common developmental disorders in children.
Awareness of the normal sexual developmental sequence in children and adolescents.
Capability to evaluate critically the use of medicine in pregnancy, children, and elderly.
Detection of developmental deviation in children (Screening & Stimulation).
Awareness of the impacts of aging on the common health parameters of the elderly.
Awareness of the common clinical manifestations and disorders in the elderly.
Diagnose and manage common health problems and disorders in the elderly.
Curriculum contents:
Normal growth patterns in children and adolescents.
Nutritional impacts on growth (and development) in infant, children and adolescents.
Clinical manifestations and diagnosis of failure to thrive.
Common congenital anomalies in infants and young children.
Clinical assessment of intrauterine growth (fetal growth).
Drug recommendation and toxicity on pregnancy and Children.
Assess development of children and adolescents in specific domains.
Methods of developmental deviation detection and stimulation.
Common developmental disorders in children and adolescents.
Diagnose common sexual developmental problems in children and adolescents.
Aging and physiologic changes in health parameters.
PLANNERS TEAM
NO NAME DEPARTMENT
1. Dr.dr. I G A Trisna Windiani, SpA (K) (Head) Child Health
2. dr. I Nyoman G. Wardana, M.Biomed (Secretary) Anatomy
3. Prof. dr. Soetjiningsih, SpAK, IBCLC Child Health
4. Prof.Dr.dr.I Nym Mangku K, M.Repro Anatomy
5. dr. Eka Putra S, Sp.THT ENT
6. dr. Wayan Eka Sutyawan, SpM Ophthalmology
7. Dr.dr. R A Tuty Kuswardhani, SpPD
(K.Ger).,MARS Geriatri
GROWTH AND DEVELOPMENT LECTURERS
NO NAME DEPARTMENT
1 Prof. dr. Soetjiningsih, SpAK, IBCLC Child Health
2 Dr.dr. I G A Trisna Windiani, SpA (K) Child Health
3 dr. I Made Kardana, SpA Child Health
4 dr. IGusti Agung Ngurah Sugitha Adnyana, SpA Child Health
5 dr. AAN Prayoga, SpA Child Health
6 dr. Made Suksmawati, SpA Child Health
7 dr. Made Arimbawa, SpA Child Health
8 dr. IGA Endah Ardjana, SpKJ Child Health
9 dr. I Gusti Lanang Sudiartha, SpA Child Health
10 dr. Dewi Sutriani Mahalini, SpA Child Health
11 Prof.Dr.dr.I Nym Mangku K, M.Repro Anatomy
12 dr. Eka Putra S, Sp.THT ENT
13 dr. Wayan Eka Sutyawan, SpM Ophthalmology
14 Dr.dr. R A Tuty Kuswardhani, SpPD
(K.Ger).,MARS Geriatri
15 dr. Nyoman Astika, SpPD Geriatri
16 dr. I GK Arijana, MSi.Med Histology
17 Dr.dr. Made Jawi, M.Kes Pharmacology
~FACILITATORS ~
REGULAR CLASS
N
O
NAME
GROUP
DEPT
PHONE
VENUE
1 Dr.dr. Elysanti Dwi Martadiani, Sp.Rad
1 Radiology 081805673099 2nd floor:
R.2.01
2 dr. Reni Widyastuti, S.Ked 2 Pharmacology 08174742501 2nd floor:
R.2.02
3 dr. Ni Ketut Putri Ariani, Sp.KJ 3 Psychiatry 082237817384 2nd floor:
R.2.03 4 dr I Gusti Agung Gede Utara
Hartawan, Sp.An, MARS
4 Anasthesi 08123868126 2nd floor:
R.2.04
5 dr. Ni Luh Ariwati 5 Parasitology 08123662311 2nd floor:
R.2.05
6 dr. I G Kamasan Nyoman
Arijana, M.Si, Med
6 Histology 08124665966 2nd floor:
R.2.06 7 Dr.dr. Ni Nyoman Sri
Budayanti, Sp.MK(K)
7 Microbiology 08553711398 2nd floor:
R.2.07
8 dr. Ni Nyoman Mahartini, Sp.PK 8 Clinical
Pathology
081337165577 2nd floor: R.2.08
9 dr. I Wayan Sugiritama, M.Kes 9 Histology 08164732743 2nd floor:
R.2.21 10 dr. Ryan Saktika Mulyana,
M.Biomed, Sp.OG
10 Obgyn 082147087905 2nd floor:
R.2.22
ENGLISH CLASS
NO NAME GROUP DEPT PHONE VENUE
1 dr. Kunthi Yulianti, Sp.KF 1 Forensic 081338472005 2nd floor:
R.2.01 2 dr. I Nyoman Budi Hartawan,
M.Sc., Sp.A(K)
2 Pediatri 081353027973 2nd floor:
R.2.02
3 dr. I Wayan Surudarma, M.Si 3 Biochemistry 081338486589 2nd floor:
R.2.03
4 dr. I Gusti Ayu Artini, M.Sc 4 Pharmacology 08123650481 2nd floor:
R.2.04
5 dr. I Ketut Mariadi, Sp.PD 5 Interna 08123853700 2nd floor:
R.2.05
6 Dr.dr. Ni Made Linawati, M.Si 6 Histology 081337222567 2nd floor:
R.2.06
7 dr. I Nyoman Gede Wardana, M
Biomed
7 Anatomy 087860405625 2nd floor:
R.2.07
8 dr. I Wyn Subawa, Sp.OT 8 Orthopaedy 081338913087
081337096388
2nd floor: R.2.08 9 Dr.rer.Nat. dr. Ni Nyoman Ayu
Dewi, M.Kes
9 Biochemistry 081337141506 2nd floor:
R.2.21
10 dr. I Komang Arimbawa, Sp.S 10 Neurology 081338226892 2nd floor:
TIME TABLE
LEARNING OUTCOMES 1: ASSESS PHYSICAL GROWTH OF CHILDREN AND ADOLESCENTS
08.00 – 08.30 08.30 – 09.00
09.00 – 11.30 11.30 – 12.30
Intro: General Concepts of Growth and Development
Lecture 1:Assessment Physical Growth of Children And Adolescents
Independent Learning + Learning Task Break
Prof. Soetji Prof. Soetji
LEARNING OUTCOMES 2: ASSESS FETAL GROWTH (INTRAUTERINE GROWTH)
12.30 – 13.30
13.30 – 15.00 Lecture 2: Independent Learning + Learning TaskThe Stages of Prenatal Development Mangku K
2
Lecture 3: Embriology of Fetal Growth
Lecture 4: Assessment Growth and Development in Neonatus
Independent Learning + Learning Task Break
Mangku K Suksmawat
LEARNING OUTCOMES 3: IDENTIFY COMMON CONGENITAL ANOMALIES IN INFANTS AND CHILDREN
12.30 – 13.30
13.30 – 15.00
Lecture 5: Prenatal Genetic Evaluation and Counseling
Independent Learning + Learning Task
Arijana
3
Wednesday
20 Jan 16
LEARNING OUTCOMES 4: CAPABILITY TO EVALUATE CRITICALLY THE USE OF MEDICINE IN PREGNANCY, CHILDREN, AND ELDERLY
08.00 – 09.00 09.00 – 11.30 11.30 – 12.30
Lecture6: Drugs in Pregnancy, Children, and Elderly
Independent Learning + Learning Task Break
Jawi
LEARNING OUTCOMES 5: DIAGNOSE AND MANAGE COMMON NUTRITIONAL PROBLEMS IN CHILDREN AND ADOLESCENTS
12.30 – 13.00
13.00 – 13.30
13.30 – 15.00
Lecture 7: Principles Breastfeeding for Infants With Normal Delivery
Lecture 8: Principles
Feeding for Infants With Complicated Delivery
Independent Learning
Lecture 9: Vitamin A, Fe & Iodine Deficiencies
Independent Learning + Learning Task Break
Lecture 10: Protein Energy Malnutrition (PEM) & Obesity
Independent Learning + Learning Task
Prayoga
10.00 – 11.00 SGD LO 1- 5Break Facilitator
LEARNING OUTCOMES 6: INVESTIGATE INFANT OR CHILD WITH SUSPECT FAILURE TO THRIVE
11.00 – 12.00 12.00 – 13.30 13.30 – 15.00
Lecture 11: Failure to Thrive
Independent Learning + Learning Task Break
6
Lecture 12: Assess Development in Motoric Domains
Lecture 13: Assess Development in Language Domains
Independent Learning + Learning Task Break
Sugitha
Sugitha
LEARNING OUTCOMES 8: DETECTION OF DEVELOPMENT DEVIATION IN CHILDREN (SCREENING AND STIMULATION)
12.30 – 13.00 13.00 – 13.30 13.30 – 15.00
Lecture 14: Cognitive Development
Lecture 15: Psychosocial Development
Independent Learning + Learning Task
Marheni
Lecture 16: Detection of Developmental Deviation In Children (Screening & Stimulation)
Individual Learning + Learning Task
SGD 2 (LO 6-8)
Break
Individual Learning + Learning Task
Trisna
Facilitator
8
Wednesday
27 Jan 16
LEARNING OUTCOMES 9: AWARENESS OF THE NORMAL SEXUAL DEVELOPMENT SEQUENCE IN CHILDREN AND ADOLESCENT
08.00 – 09.00
09.00 – 11.30 11.30 – 12.30
Lecture 17: Sexual
Developmental Sequence in Children and Adolescent
Independent Learning + Learning Task Break
Arimbawa
LEARNING OUTCOMES 10: AWARENESS OF COMMON DEVELOPMENTAL DISORDERS IN CHILDREN
12.30 – 13.00 13.00 – 13.30 13.30 – 15.00
Lecture 18: Visual Impairment
Lecture 19: Hearing Impairment
Independent Learning + Learning Task
Eka Sutyawan
Lecture 20: Learning Disorders
Lecture 21: Down Syndrome and Mental Retardation
Independent Learning + Learning Task Break
Lecture 22: Attention Deficit/Hyperactivity Disorders
Lecture 23: Autism Spectrum Disorders
Independent Learning + Learning Task
Endah
Lecture 24: Cerebral Palsy
Independent Learning + Learning Task
SGD 3 (LO 9-10)
Independent Learning + Learning Task Break
LEARNING OUTCOMES 11: AGING AND ITS CLINICAL IMPLICATIONS
08.00 – 09.00 09.00 – 11.30 11.30 – 12.30 12.30 – 13.30 13.30 – 15.00
Lecture 25: Aging Process
Independent Learning + Learning Task Break
Lecture 26: Clinical Implication of Aging Process
Independent Learning + Learning Task
Tuty K
13
LEARNING OUTCOMES 1: ASSESS PHYSICAL GROWTH OF CHILDREN AND ADOLESCENTS
09.00 – 09.30 09.30 – 10.00
10.00 – 12.30 12.30 – 13.30
Intro: General Concepts of Growth and Development
Lecture 1:Assessment Physical Growth of Children And Adolescents
Independent Learning + Learning Task Break
Prof. Soetji Prof. Soetji
LEARNING OUTCOMES 2: ASSESS FETAL GROWTH (INTRAUTERINE GROWTH)
13.30 – 14.30
14.30 – 16.00 Lecture 2: Independent Learning + Learning TaskThe Stages of Prenatal Development Mangku K
2
Lecture 3: Embriology of Fetal Growth
Lecture 4: Assessment Growth and Development in Neonatus
Independent Learning + Learning Task Break
Mangku K Suksmawat
LEARNING OUTCOMES 3: IDENTIFY COMMON CONGENITAL ANOMALIES IN INFANTS AND CHILDREN
13.30 – 14.30
14.30 – 16.00
Lecture 5: Prenatal Genetic Evaluation and Counseling
Independent Learning + Learning Task
Arijana
3
Wednesday
20 Jan 16
LEARNING OUTCOMES 4: CAPABILITY TO EVALUATE CRITICALLY THE USE OF MEDICINE IN PREGNANCY, CHILDREN, AND ELDERLY
09.00 – 10.00 10.00 – 12.30 12.30 – 13.30
Lecture6: Drugs in Pregnancy, Children, and Elderly
Independent Learning + Learning Task Break
Jawi
LEARNING OUTCOMES 5: DIAGNOSE AND MANAGE COMMON NUTRITIONAL PROBLEMS IN CHILDREN AND ADOLESCENTS
13.30 – 14.00
14.00 – 14.30
14.30 – 16.00
Lecture 7: Principles Breastfeeding for Infants With Normal Delivery
Lecture 8: Principles
Feeding for Infants With Complicated Delivery
Independent Learning
Prof. Soetji
4
Lecture 9: Vitamin A, Fe & Iodine Deficiencies
Independent Learning + Learning Task Break
Lecture 10: Protein Energy Malnutrition (PEM) & Obesity
Independent Learning + Learning Task
Prayoga
10.00 – 12.00 BreakSGD 1 (LO 1-5) Facilitator
LEARNING OUTCOMES 6: INVESTIGATE INFANT OR CHILD WITH SUSPECT FAILURE TO THRIVE
12.00 – 13.00 13.00 – 14.30 14.30 – 16.00
Lecture 11: Failure to Thrive
Independent Learning + Learning Task Break
Lanang
6
Friday
22 Jan 16
LEARNING OUTCOMES 7: ASSESS DEVELOPMENT OF CHILDREN IN SPECIFIC DOMAINS
09.00 – 09.30
09.30 – 10.00
10.00 – 12.30 12.30 – 13.30
Lecture 12: Assess Development in Motoric Domains
Lecture 13: Assess Development in Language Domains
Independent Learning + Learning Task Break
Sugitha
Sugitha
LEARNING OUTCOMES 8: DETECTION OF DEVELOPMENT DEVIATION IN CHILDREN (SCREENING AND STIMULATION)
13.30 – 14.00 14.00 – 14.30 14.30 – 16.00
Lecture 14: Cognitive Development
Lecture 15: Psychosocial Development
Independent Learning + Learning Task
Marheni
Lecture 16: Detection of Developmental Deviation In Children (Screening & Stimulation)
Individual Learning + Learning Task Break
SGD 2 (LO 6-8)
Individual Learning + Learning Task
Trisna
Facilitator
8
Wednesday
27 Jan 16
LEARNING OUTCOMES 9: AWARENESS OF THE NORMAL SEXUAL DEVELOPMENT SEQUENCE IN CHILDREN AND ADOLESCENT
09.00 – 10.00
10.00 – 12.30 12.30 – 13.30
Lecture 17: Sexual
Developmental Sequence in Children and Adolescent
Independent Learning + Learning Task Break
Arimbawa
LEARNING OUTCOMES 10: AWARENESS OF COMMON DEVELOPMENTAL DISORDERS IN CHILDREN
13.30 – 14.00 14.00 – 14.30 14.30 – 16.00
Lecture 18: Visual Impairment
Lecture 19: Hearing Impairment
Independent Learning + Learning Task
Eka Sutyawan
Lecture 20: Learning Disorders
Lecture 21: Down Syndrome and Mental Retardation
Independent Learning + Learning Task Break
Lecture 22: Attention Deficit/Hyperactivity Disorders
Lecture 23: Autism Spectrum Disorders
Independent Learning + Learning Task
Endah
Lecture 24: Cerebral Palsy
Break
Independent Learning + Learning Task
SGD 3 (LO 9-10)
Independent Learning + Learning Task
D. Sutrini
11
Monday
1 Feb 16
LEARNING OUTCOMES 11: AGING AND ITS CLINICAL IMPLICATIONS
09.00 – 10.00 10.00 – 12.30 12.30 – 13.30 13.30 – 14.30 14.30 – 16.00
Lecture 25: Aging Process
Independent Learning + Learning Task Break
Lecture 26: Clinical Implication of Aging Process
Independent Learning + Learning Task
Tuty K
N Astka
12
Tuesday
2 Feb 16
09.00 – 10.00 10.00 – 12.00 12.00 – 13.00 13.00 – 14.00 14.00 – 15.00 15.00 – 16.00
SGD 3 (LO 11)
SP Presentaton Break
Lecture: General Principles of Physical Examination Lecture: Vital Sign Measurement
Individual Learning
Facilitators Tim
Ratna S Ratna S
13
Wednesday
3 Feb 16
SILENT DAY
14
Thursday
4 Feb 16 EXAMINATION
~ LEARNING PROGRAMS ~
LECTURE
Prof. dr. Soetjiningsih, SpAK, IBCLC
Learning outcomes
- To describe the general concept of growth and development - To describe the stages in lifespan development
- To understand the conceptual differences between growth and development - To describe the factors that may affect growth and development
Abstract
Lifespan development is a field of study that examines patterns of growth, change, and stability in behavior that occur throughout the entire life span. The life span is usually divided into broad age ranges: the prenatal period (the period from conception to birth); infancy and toddler hood (birth to age 3); the preschool period (ages 3 to 6); middle childhood (ages 6 to 12); adolescence (ages 12 to 20); young adulthood (ages 20 to 40); middle age (ages 40 to 60); and late adulthood (age 60 to death).
Lifespan development specialists discuss development in several topics: physical development (development involving the body’s physical make up, including the brain, nervous system, muscles, senses, and the need for food, drink and sleep); cognitive development (development involving the ways that growth and change in intellectual capabilities influence a person’s behavior); personality development (development involving the ways that enduring characteristics that differentiate one person from another change over the life span); and social development ( the way in which individuals’ interactions with others and their social relationships grow, change, and remain stable over the course of life).
Growth and development are an integral process. Growth refer to the metabolic change by which an organism increases in size and changes shape. Growth refers to quantitative changes. Changes in physical size and appearance are visible manifestations of the complex morphologic, biochemical and physiologic changes taking place during childhood.
Child development is a process, a continuous series of purposeful changes, consisting of many aspects, moving together at differing paces. Development refers to qualitative and quantitative changes. There are 10 fundamental principles of development:
1. Development involves change
2. Early development is more critical than later development 3. Development is the product of maturation and learning 4. The developmental pattern is predictable
5. The developmental pattern has predictable characteristics 6. There are individual differences in development
7. There are periods in the developmental pattern
8. There are social expectations for every developmental period 9. Every area of development has potential hazards
10. Happiness varies at different periods in development
Environmental and genetic factors influence growth and development. In Bronfenbrenner’s ecological system theory, development is influenced at four levels: the microsystem, mesosystem, exosystem and macrosystem.
Prof. dr. Soetjiningsih, SpAK, IBCLC
Learning outcomes
- Describe the clinical importance of study physical growth - Describe the normal patterns of the physical growth - Understand factors that affecting physical growth - Use of common growth parameter
Abstract
Physical growth usually refers to changes in size or mass. The most people usually think of growth at the level of the whole child, the cells and internal structures that make up the child, primarily by increasing in number or size.
Growth assessment is essential because almost any problems within the physiologic, interpersonal and social domains can adversely affect growth. Anthropometry is an effective and frequently performed child health screening procedure. The value of physical growth data depends on their accuracy and reliability, how they are recorded and interpreted, and what follow-up efforts are made after identification of growth abnormality.
The most powerful tool in growth assessment is the growth chart. Whenever possible, growth should be assessed by plotting accurate measurements on growth charts and comparing each set of measurements with previous measurements. The CDC Growth Charts 2000 are used to measure growth, consist of 16 charts including “Body mass index (BMI) for-age percentile” for boys and girls aged 2-20 years.
Normal growth patterns have spurts and plateaus, but some shifting on the percentile graphs can be expected; however, large shifts warrant attention. Large discrepancies among height, weight, and head circumference percentiles also diserve attention. Deviation in growth patterns are nonspecific but important indicators of serious medical disorders. Deviations often provide the first clue that something is wrong, occasionally even when the parents do not suspect a problem. An accurate measurement of height, weight, and head circumference should be obtained at every health supervision visit. Serial measurements are much more useful than single measurements because they can help detect deviations from a particular child’s growth pattern even if the value remains within statistically defined normal limits.
Factors affecting physical growth and health in infancy and toddlerhood continue to be influential in early childhood. Heredity affects physical growth by regulating the production of hormones. Extreme emotional deprivation can interfere with the production of growth hormone, thereby stunting children's growth. Sleep difficulties, in the form of night waking and nightmares, are common during the preschool years. Appetite decline is associated with a slower rate of physical growth. Disease can lead to malnutrition, seriously undermining children's growth, an effect that is especially common in
Lecture 1:
Nym Mangku Karmaya
Learning outcomes
Describe the main stages of embryonic development for use to estimate the gestational age of embryo.
Abstract
Early embryonic development is describe in stages because of the variable period it takes for embryos to develop certain morphological characteristics. Stage 1 of development begins at fertilization and embryonic development ends at stages 23, which occur on day 57 and ends when he fetus is completely outside the mother. The stages of embryonic development can be assessed by ultrasonography. In general the period of prenatal development is as follows:
1st week : zygote-blastomeres-morula-blastocyst.
2nd week : bilaminar germ disc
3rd week : trilaminar germ disc
3rd - 8th week : embryonic period/organogenesis
8th week-BIRTH : fetal period
Mangku Karmaya
Learning outcomes
- ~ soon will be added ~
Abstract
In a low-risk pregnancy, the abdomen is measured at prenatal visits to assess the baby's growth. The measurement in centimeters from the top of your pubic bone to the top of your uterus (the fundus) should be about the same as the number of weeks you are pregnant, with an allowance of up to 2 cm either way. For example, if you are 26 weeks' pregnant, you should measure between 24 and 28 cm. Your fundal height can be measured between 24 and 36-37 weeks, since once your baby "drops" into the pelvis in late pregnancy, the measurement may not reflect his or her true size. If there is a variation of 3 cm or more, your doctor will arrange for an ultrasound to check your baby's growth and the amount of amniotic fluid. If the scan indicates a problem, the doctor will arrange for scans every two weeks since analyzing growth patterns over time gives a more accurate assessment of whether your baby's growth is normal.
Lecture 2:
~ The Stages of Prenatal Development ~
Lecture 3:
Lecture 4:
~ Assessment of Growth and Development in Neonatus
Dharma Artana
Learning outcomes
- Apply the New Ballard Score to assess the gestational age of infant: the small for gestational age (SGA), appropriate for gestational age (AGA), or large for gestational age (LGA).
Abstract
Since the late 1960s, a variety of methods for assessing the gestational age of the newborn infant have been developed. Currently, the most widely use system for the postnatal assessment of gestational age is the New Ballard Score (NBS). This system includes both physical and neurologic characteristics. The score spans from 10 (correlating with 20 weeks’ gestation) to 50 (correlating with 44 weeks gestation). The examination consists of six neuromuscular criteria and six physical criteria. The neuromuscular criteria are based on the understanding that passive tone is more useful than active tone in indicating gestational age. The neuromuscular maturity includes: posture, square window, arm recoll, popliteal angel, scarf sign, and heal to ear. The physical maturity includes: skin, lanugo hair, plantar surface, breast, ear and ear, and genitalia. The examination of NBS is administered twice by two different examiners to ensure objective, and the data entered on the chart.
I GK Arijana Abstract
Genetic counseling is a process of communication and education which addresses concerns relating to the development and/or transmission of a hereditary disorder. The process involves several steps, namely diagnosis (based on accurate family history, medical history, examination and investigations), risk assessment, communication, discussion of options, long-term contact and support. Diagnosis is the most crucial step due to if the diagnosis is incorrect hence the result is inappropriate information and tragic consequences. The next step is risk assessment, meaning calculating the recurrence risk for the next pregnancy (recurrence risks should be quantified, qualified and placed in context). Discussion of options like prenatal diagnosis or others reproductive options (donor sperm, donor ova, and preimplantation genetic diagnosis). Communication meaning two-way process of information, not only from counselor. Long-term contact and support meaning providing support and companionship for example like patient supportive group. Finally, genetic counseling should be non-directive (meaning patients can reach their own decision after full information from counselor).
Lecture 5:
Prenatal diagnosis is one of discussion option (as mentioned above). The indications for prenatal diagnosis are advanced maternal age, previous child with a chromosome abnormality, family history of a chromosome abnormality, family history of a single-gene disorder, family history of a neural tube defect, family history of other congenital structural abnormalities, abnormalities identified in pregnancy, other high-risk factors. Techniques which are used in prenatal diagnosis can be divided into 2, namely invasive and non invasive methods. Invasive methods are including amniocentesis, chorionic villus sampling, fetoscopy, cordocentesis. Non-invasive methods are including ultrasound, maternal serum screening, detection of fetal cells in the maternal circulation, detection of cell-free fetal nucleic acid in the maternal circulation. Preimplantation Genetic Diagnosis (PGD) is a special case in prenatal diagnosis.
Made Jawi
Learning outcomes
After completing this lecture, the students should be able to:
- Describethe effect of drugs use in pregnancy.
- To Choose the safe drugs for pregnant women, children, and elderly
Abstract
When a woman becomes pregnant, it is very important for her to lead a healthy life: to eat plenty of nourishing food, get plenty of rest, and exercise regularly. It is also vital that she avoid anything that might harm her or her baby-to-be. It is especially important to give up alcohol, cigarettes, and drugs. For a pregnant woman, drug abuse is doubly dangerous. First, drugs may harm her own health, interfering with her ability to support the pregnancy. Second, some drugs can directly impair prenatal development. Both prescription and over-the-counter drugs can be harmful, for her own health and the health of her baby-to-be. So a woman should avoid all of them as much as possible, from the time she first plans to become pregnant or learns that she is pregnant. Some drugs can be harmful when used at any time during pregnancy; others, however, are particularly damaging at specific stages. Most of the body organs and systems of the baby-to-be are formed within the first ten weeks or so of pregnancy (calculated from the date of the last menstrual period). During this stage, some drugs and alcohol in particular can cause malformations of such parts of the developing fetus as the heart, the limbs, and the facial features. After about the tenth week, the fetus should grow rapidly in weight and size. At this stage, certain drugs may damage organs that are still developing, such as the eyes, as well as the nervous system. Continuing drug use also increases the risk of miscarriage and premature delivery. But the greatest danger drugs pose at this stage is their potential to interfere with normal growth. Intrauterine growth retardation (IUGR) is likely to result in a low-birth weight baby a baby born too early, too small, or both. Low-birth weight babies require special care and run a much higher risk of severe health problems or even death.
Lecture 6:
Current Categories for Drug Use in Pregnancy
Category Description
A Adequate, well-controlled studies in pregnant women have not shown an increased risk of fetal abnormalities.
B Animal studies have revealed no evidence of harm to the fetus; however, there are no adequate and well-controlled studies in pregnant women.
Or
Animal studies have shown an adverse effect, but adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus.
C Animal studies have shown an adverse effect and there are no adequate and well-controlled studies in pregnant women.
Or
No animal studies have been conducted and there are no adequate and well-controlled studies in pregnant women.
D Studies, adequate well-controlled or observational, in pregnant women have demonstrated a risk to the fetus. However, the benefits of therapy may outweigh the potential risk.
X Studies, adequate well-controlled or observational, in animals or pregnant women have demonstrated positive evidence of fetal abnormalities. The use of the product is contraindicated in women who are or may become pregnant.
Both prescription and over-the-counter drugs can be harmful, for children and elderly. There are a number of pharmacokinetic and pharmacodynamic differences between children or pediatric, elderly and adult patients. Neonates ( 0 to 1 month), infants (1 to 12 month) and children of increasing age are not simply small adult.
The drugs used by the elderly are the same as those that a younger person might take--yet they can have a far different effect. It doesn’t matter whether a person has heart disease or arthritis, osteoporosis, or high blood pressure, the story is the same: Because the organ systems tend to function less efficiently as we age, medications are handled differently by our bodies. Here are some of the most common changes affecting our health and our response to medicines:
The stomachs may not absorb food and medication as well as they did before. The kidneys and livers don’t eliminate fluids and toxins in the same efficient manner. All of the above contribute to the potential harm that medications can cause in the aging body. If a kidney can’t eliminate a drug after it has done its work, it remains in the body longer, perhaps causing an overdose or an adverse effect. If someone forgets to take a medication that regulates the heart or blood pressure, a stroke or heart attack could be the result.
Any person over the age of 65 who is taking medications in the following categories should be aware of the potential for increased side effects, overdose, and diminished efficacy: Antibiotics, Anti histamines, Anti hypertensives, Antiulcer medicines, Blood thinners, Bronchodilators, Calcium or potassium supplements, Cardiac medications, Corticosteroids, Estrogens, Over-the-counter drugs containing alcohol (cough and cold medications) or caffeine, Pain relievers, Psychiatric medications, Skin medications and creams
Prof. dr. Soetjiningsih, SpAK, IBCLC
Abstract
Breast-feeding exclusively the recommended method for feeding normal infants during the first 6 months of life. Breastfeeding should continue with the addition of appropriate foods, for two years or more.
Breastfeeding has advantages for infants, mothers, families, and society. These advantages include health, nutritional, immunologic, developmental, psychologic, social, economic, and environmental benefits. Breast milk contains the right balance of nutrients to help the infant grow into a strong and healthy toddler. Some of the nutrients in breast milk also help protect the infant against some common childhood illnesses and infections. While nutrients and antibodies pass to the baby, beneficial hormones are released from the mother's body. Colostrums, a high protein and low fat lactose product, are produced in small amounts during the first few postpartum days. It has some nutritional value but primarily has important immunologic and maturational properties. The bond between baby and mother can also be strengthened during breastfeeding.
Breastfeeding doesn't always happen easily. Some new mums find it hard to get started, while others hit problems later on. Breast tenderness, engorgement, and cracked nipples are the most common problems encountered by mothers who are breast-feeding.
Kardana
Learning outcomes
- To know indication of enteral and parenteral nutrition
- To know the type nutrition’s for enteral feeding
- To know the routes of enteral feeding and feeding technique
- To know the administration for parenteral nutrition
- To know the contents of total parenteral nutrition
Abstract
Providing adequate nutrition support to newborns is an important to know and understanding the maturation, functional and physical disturbances to the baby. Optimal nutrition after birth enhances future neurodevelopmental outcome. For term healthy infants should be breast-fed as soon as possible within the first hour. Human milk is preferred for feeding term, preterm and sick infants. The following criteria should usually be met before initiating infant’s feedings: no history of excessive oral secretions, vomiting, or bilous-stained gastric aspirate, non-distended, soft abdomen with normal bowel sound, and no respiration distress. If the baby is small or complicated baby such as baby with the following associated conditions: perinatal asphyxia, hemodynamic instability, sepsis, frequent episodic apnea and bradycardia etc, initiation of enteral feeding is often precluded and parenteral nutrition can be initiation. Nutritional requirements in neonate includes: calories to maintain weight and to induce weight gain, carbohydrates, proteins, fats, vitamins and minerals and fluids.
Lecture 8:
~ The Principles of Feeding for Infants with Complicated Deliveries ~
Lecture 7:
A A Ngr Prayoga
~ Vitamin A and Fe Deficiency ~
Learning outcomes
- To understand the sign and symptom of patient with vitamin A and Fe deficiency
- To built diagnosis of patient with vitamin A and Fe deficiency
- To understand the treatment and prevention of patient with vitamin A and Fe deficiency
Abstract
Vitamin A is the generic term used to describe all retinoid having the biologic activity of all-trans retinol. Vitamin A, a light yellow crystalline alcohol, has been named retinol in reference to its specific function in the retina of the eye. The yellow-orange-red provitamin carotinoids, are describe in the term of beta-carotene
A deficiency of Vitamin A is accompanied by keratinization of the mucous membranes that line the respiratory tract, the alimentary canal, and the urinary tract, and by keratinization of the body skin and epithelium of the eye, which lowers the barrier role played by these membranes in protection of the body against infections. Prolonged deficiency may produce skin changes, night blindness, and corneal ulceration.
Primary deficiencies of vitamin A are the result of dietary inadequacies. Secondary can result from liver disease, protein-energy malnutrition, abetalipoproteinemia, or malabsorption due to bile acid insufficiency. Acute deficiency is treated with large oral doses of vitamin A and correction of the usually concomitant protein-energy malnutrition. Massive intermittent dosing with 200,000 IU of vitamin A can reduced mortality by 35 to 70 %.
Iron deficiency anemia is characterized by the production of small erythrocytes and diminished level of circulating hemoglobin.
The three primary causes of iron deficiency anemia are chronic blood lose, faulty iron intake or absorption and increased iron requirement.
The clinical findings are fatigue, anorexia, pica (pagophagia). Growth abnormalities, epithelial disorders, and reduction in gastric acidity are common. Defect in structure and function of epithelial tissue of tongue, nails, mouth, and stomach as deficiency becomes more severe.
The chief treatment for iron deficiency consists of oral administration of inorganic iron in the ferrous form and nutritional care.
~ Iodine Deficiency ~
Learning outcomes
- To understand the sign and symptom of patient with iodine deficiency.
- To built diagnosis of patient with iodine deficiency.
- To understand the treatment and prevention of patient with iodine deficiency.
Lecture 9:
Abstract
Iodine is absorbed easily in the form of iodide, in circulation it occurs both as free and protein-bound iodine. Iodine is stored in the thyroid, where it is used for synthesis of T3 and T4 when needed.
Lack of iodine intake is associated with the development of endemic or simple goiter, which is an enlargement of thyroid gland. The deficiency may be absolute, especially in areas of subnormal iodine intake, or relative subsequent to increased need for thyroid hormones, such as in the female during adolescence, pregnancy, and lactation. Severe iodine deficiency during gestation and early postnatal growth results in cretinism, a syndrome characterized by mental deficiency, spastic diplegia, or quadriplegia, deaf mutism, dysarthria, a characteristic shuffling gait, shortened stature, and hypothyroidism. Early diagnosis and treatment are needed to prevent more severe of clinical sign and symptom
Lanang
~ Protein Energy Malnutrition (PEM) ~
Learning outcomes
- To understand the sign & symptom of patient with protein energy malnutrition (PEM)
- To built diagnosis of patient with protein energy malnutrition (PEM)
- To understand the treatment and prevention of the patient with protein energy malnutrition (PEM)
Abstract
Definition
PEM is a spectrum of conditions caused by varying levels of protein and calorie deficiencies. The common form of primary PEM is marasmus and caused by severe caloric depletion. Kwashiorkor, presenting with pitting edema caused by inadequate protein intake in the presence of fair to good caloric intake. Secondary form of PEM is associated with other diseases.
Clinical manifestation
The clinical manifestation of marasmus: The body weight below 60% of expected for age or below 70% of the ideal weight for height and depleted body fat stores. Edema usually is absent. The head may appear large but generally proportional to the body length. The clinical manifestation of kwashiorkor: presenting pitting edema that starts in lower extremities and ascends with increasing severity, may be a complication of critical illness (acute and chronic infections, multiorgan system failure, anorexia nervosa, etc)
Treatment and prevention
Calories account of nutritional rehabilitation can be safety started at 20% above the child’s recent intake. The calorie intake can be increased 10-20% per day until appropriate re-growth is initiated. This may require 150% or more of the recommended calories for an age-matched, well nourished child.
Lecture 10:
~ Obesity ~
Learning outcomes
- To understand the sign & symptom of patient with obesity
- To built diagnosis of patient with obesity
- To understand the treatment and prevention of the obesity
Epidemiology
The prevalence of obesity in children has increased in the last 2-3 decades, mainly in children as young as 4-5 years.
Clinical manifestation
In children BMI (body mass index) age and gender specific percentile curves allow an assessment of BMI percentile. In adolescent and adult BMI has been used in weight/height2 (kg/m2).
The effects of obesity complication; such as psychosocial effect, growth (advanced bone age, increased height, early menarche), CNS (pseudo tumor cerebri, respiratory (sleep apnea, pickwickian syndrome), cardiovascular (hypertension, cardiac hypertrophy, ischemic heart disease, sudden death), orthopedic (slipped capital femoral epiphysis, Blount disease), metabolic (insulin resistance, type II diabetes mellitus, hypertriglyceridemia, hypercholesterolemia, gout, hepatic steatosis, ovary disease, cholelithiasis).
Treatment and prevention
The treatment and prevention of obesity includes a combination of education, behavior modification, exercise and diet.
Lanang
Learning outcomes
1. To apply the diagnostic criteria of patient with failure to thrive (FTT). 2. To discuss the cause or path physiology of patient with FTT.
3. To evaluate and manage a child with FTT.
Definition
The term ‘failure to thrive’ first was used to describe the malnutrition and depressed condition of many institutionalized infants in early 1900s. It remains a descriptive rather than a diagnostic label applied to children whose attained weight or rate of weight gain is significantly below that of other children of similar age and same sex.
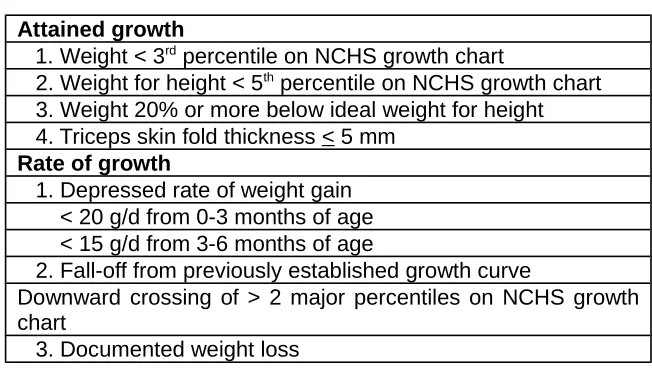
Table Definition of failure to thrive
Attained growth
1. Weight < 3rd percentile on NCHS growth chart
2. Weight for height < 5th percentile on NCHS growth chart 3. Weight 20% or more below ideal weight for height 4. Triceps skin fold thickness < 5 mm
Rate of growth
1. Depressed rate of weight gain < 20 g/d from 0-3 months of age < 15 g/d from 3-6 months of age
2. Fall-off from previously established growth curve
Downward crossing of > 2 major percentiles on NCHS growth chart
3. Documented weight loss
Patho physiology and clinical manifestation
FTT can result from wide range of factors, including serious medical disease, dysfunctional child-caregiver interactions, poverty, parental misinformation, and child abuse. The physical examination of a child who is growing poorly should focus on identifying sign of underlying organic disease, severity of malnutrition, and important concomitant finding such as evident of physical abuse/neglect or the presence of deprivational behaviors.
Treatment and prevention
Management of the child with psychosocial failure to thrive must be individualized to the specific needs of the child and family. Nutritional rehabilitation, efforts are focused on correcting the dysfunctional child-parent interaction by addressing areas of parental misinformation, providing and helping to implement specific feeding guidelines, and addressing the larger psychosocial needs of the family. A multidisciplinary team approach involving the primary-care provider, nutritionist, social worker, child behavior specialist, and community-based outreach services is often most beneficial.
I GA Trisna W
~ Assess Development in The Motoric Domain ~
Learning outcomes:
- Describe gross and motor development
- Determine factors affecting motor development
Abstract
Child developmental consist of several skills like: 1) Gross motor: using large groups of muscles to sit, stand, walk, run, etc., keeping balance, and changing positions; 2) Fine motor: using hands to be able to eat, draw, dress, play, write, and do many other things; 3) Language: speaking, using body language and gestures, communicating, and
Lecture 12 &13:
understanding what others say; 4) Cognitive: Thinking skills: including learning, understanding, problem-solving, reasoning, and remembering; 5) Social: Interacting with others, having relationships with family, friends, and teachers, cooperating, and responding to the feelings of others.
Developmental milestones are a set of functional skills or age-specific tasks that most children can do at a certain age range. Milestone can be described as what a child accomplishes throughout the different stages in their life. We can use milestones to help check how our child is developing. Although each milestone has an age level, the actual age when a normally developing child reaches that milestone can very quite a bit. Every child is unique. To determine whether a child has developmental delay, the physician must understand normal milestones
The red flag age is the age at which you would expect almost every child to have already mastered a particular skill. For example walking, most children walk on their own, without holding on, around their first birthday. By 15 months--the red flag age for walking--a child who has not taken his first independent steps is certainly slower to walk than 90 percent of other children. Red flag milestones are helpful because they put a limit on when you, as a good, concerned parent, should worry.
Motor development means the development of control over bodily movements through the coordinated activity of the nerve centers, the nerves and the muscles. This control comes from the development of the reflexes and mass activity present at birth. Until this development occurs, the child will remain helpless.
From longitudinal studies of babies and young children, five general principles of motor development have emerged: 1) motor development depends on neural and muscular development; 2) learning skills cannot occur until the child is maturationally ready; 3) motor development follows a predictable pattern; 4) it is possible to establish norms for motor development; and 5) there are individual differences in rate of motor development.
Motor development is divided into gross motor and fine motor development. Gross motor skills refer to the ability of children to carry out activities that require large muscles or groups of muscles. Muscles or groups of muscles should act in a coordinated fashion to accomplish a movement or a series of movements. Examples of gross motor tasks are walking, running, throwing something, jumping, standing on 1 leg, playing hopscotch, and swimming. Posture is an important element to consider in the assessment of gross motor skills. Adequate posture may make all the difference between being able or not able to execute a movement.
Fine motor skills consist of movements of small muscles that act in an organized and subtle fashion, for instance, the hands, feet, and muscles of the head (as the tongue, lips, facial muscles), to accomplish more difficult and delicate tasks. Fine motor skills are the basis of coordination, which begins with transferring from hand to hand crossing the midline when aged 6 months. Examples of fine motor activities are writing, sewing, drawing, putting a puzzle together, imitating subtle facial gestures, pronouncing words (which involve coordination of the soft palate, tongue, and lips), blowing bubbles, and whistling. Many children who have difficulties in their fine motor skills also have difficulties in articulating sounds or words.
The static and motor development of newborn into adult depends on the maturation process of the central nervous system. The process of this development is determined by genetically established patterns of behavior and stimulation from the environment. Some conditions that influence the rate of motor development. These factors include genetic constitution, prenatal condition, prematurity, nutrition, physical defects, stimulation, etc. They may contribute to poor abilities in motor functioning and coordination difficulties
I GA Trisna W
~ Assess Development in The Language Domain ~
Learning outcomes
- Describe language development
- Determine factors affecting language development
Abstract
Speech and language are tools that humans use to communicate or share thoughts, ideas, and emotions. Language is different from speech. Language is an elaborate system of communication that uses arbitrary and socially agreed on symbols to transmit and to receive messages from one human to another. Language is made up of socially shared rules that include the following: what words mean; how to make new words; how to put words together; and what word combinations are best in what situations. Speech is the verbal means of communicating. Speech consists of the following: articulation (how speech sounds are made); voice (use of the vocal folds and breathing to produce sound); and fluency (the rhythm of speech).
There are many languages in the world, each includes its own set of rules for phonology (phonemes or speech sounds or, in the case of signed language, hand shapes), morphology (word formation), syntax (sentence formation), semantics (word and sentence meaning), prosody (intonation and rhythm of speech), and pragmatics (effective use of language).
The most intensive period of speech and language development for humans is during the first three years of life, a period when the brain is developing and maturing. These skills appear to develop best in a world that is rich with sounds, sights, and consistent exposure to the speech and language of others. Children vary in their development of speech and language. There is, however, a natural progression or "timetable" for mastery of these skills for each language. The milestones are identifiable skills that can serve as a guide to normal development. Typically, simple skills need to be reached before the more complex skills can be learned. There is a general age and time when most children pass through these periods. These milestones help doctors and other health professionals determine when a child may need extra help to learn to speak or to use language.
When a person has trouble understanding others (receptive language), or sharing thoughts, ideas, and feelings completely (expressive language), then he or she has a language disorder. Receptive language refers to the ability to understand, encompasses visual (reading, sign language comprehension) and auditory (listening comprehension) skills. Expressive language refers to the ability to produce symbolic communication, this output may be either visual (writing, signing) or auditory (speech)
Delay in speech and language development in children can be defined as a “delay in speech and / or language development compared with controls matched for age, sex, cultural background, and intelligence”, or a discrepancy between a child’s potential ability to speak and the performance that is actually observed. Three common causes of speech delay are mental retardation, hearing loss and maturation delay.
Marheni
Learning outcomes:
a. To understand the basic principles of cognitive process. b. To understand four stages of cognitive development
Abstract:
Most progressive change of human behavior related to cognitive development, so if someone wants to understand growth and development of human being
comprehensively, they should learn about cognitive development.
Piaget specifies four stages of cognitive development. The major cognitive achievement in the sensorimotor stage (which lasts from birth to about two years) is the development of the schema of object permanency. Thus, the attainment of this knowledge is indicative of representational ability. Such ability is involved in the major cognitive achievements in the preoperational stage (which lasts from about two through six years). Here, true systems of representation develop (e.g., as indexed by language, symbolic play, and delayed imitation). With the emergence of the concrete operational stage, however (which lasts from about six through twelve years), conservations are typically seen; thus, operational structures – internalized actions that are reversible – are evidence. The child cannot think counterfactually or hypothetically. Such ability characterizes the last stage of cognitive development, the formal operational stage
(which lasts from about year twelve onward).
Marheni
Absract:
Psychosocial development as propounded by Erik Erikson describes eight
developmental stages through which a healthily developing human should pass from
infancy to late adulthood. In each stage the person confronts, and hopefully masters, new challenges. Each stage builds on the successful completion of earlier stages. The challenges of stages not successfully completed may be expected to reappear as problems in the future.
Erik Erikson developed the theory in the 1950s as an improvement on Sigmund Freud's psychosexual stages. Erikson accepted many of Freud's theories (including the
id, ego, and superego, and Freud's infantile sexuality represented in psychosexual development), but rejected Freud's attempt to describe personality solely on the basis of sexuality. Also, Erikson criticized Freud for his concept of originology. This states that all mental illness can be traced to early experiences in childhood. According to Erikson, experience in early childhood is important, but the individual also develops within a social context. Erikson believed that childhood is very important in personality development and, unlike Freud, felt that personality continued to develop beyond five years of age. In his most influential work, Childhood and Society 1950, he divided the human life cycle into eight psychosocial stages of development.
Lecture 14:
~ Cognitive Development ~
Lecture 15:
“ Human personality, in principle, develops according to steps predetermined in the growing person's readiness to be driven toward, to be aware of, and to interact
with a widening social radius. ”
—Erik Erikson
dr. I GA Trisna Windiani, SpA/dr. I GA Ngurah Sugitha
Learning outcomes
- Describe the aims of detection developmental deviation - Recognize the methods of detection developmental deviation
- Apply methods of detection developmental deviation (Denver test, Pediatric Symptom Checklist / PSC test)
- Describe the aims of stimulation developmental deviation - Understand the principles of early stimulation
- Recognize the methods of stimulation developmental deviation
Abstract
Developmental screening is a brief evaluation of developmental skills that is applied to a total population of children to identify children with suspected delays who require further diagnostic assessment. Developmental screening involves the use of standardized screening tests. Screening tests can be categorized as general screening tests that cover all behavioral domains or as targeted screens that focus on one area of developmental. They can administer in the office setting by professionals or completed at home by parents.
The Pediatric Symptom Checklist is a psychosocial screen designed to facilitate the recognition of cognitive, emotional, and behavioral problems so that appropriate interventions can be initiated as early as possible. Included here are two versions, the parent-completed version (PSC) and the youth self-report (Y-PSC). PSC can be administered to 4-18 years old while Y-PSC can be administered to adolescents ages 11 and up.
The Denver II is design to be used with apparently well children between birth and six years of age and is administered by assessing a child’s performance on various age appropriate tasks. The test is valuable in screening asymptomatic children for possible problem, in continuing intuitive suspicious with an objective measure, and in monitoring children at risk for developmental problems, such as those who have experienced perinatal difficulties. The Denver II consist of 125 tasks, or items which arranged on the test form in four sectors to screen areas of function: 1) personal social; 2) Fine motor adaptive; 3) Language; and 4) gross motor
Early intervention or stimulation is necessary and effective because development is malleable and readily affected by the environment. In large part, early intervention works by systematically removing external risk factors. Early intervention programs place children in developmentally enriching settings; train parents in responsiveness and
Lecture 16:
effectiveness, and provide continuous positive redirection and focused building of skills. The benefits of early intervention clearly depend on early detection, which requires that clinicians know how to identify accurately patients who have disabilities. Because time and reimbursement are limited, clinicians also should know how to identify patients quickly. Appropriate stimulation in childhood ranks as one of the most important factors that influence childhood development.
W Bikin Suryawan/Arimbawa
Learning outcomes
- To interpret maturation of the hypothalamic-pituitary-gonadal axis and connecting with the onset of puberty starts.
- To explain positive feedback and negative feedback in puberty regulation.
- To interpret kind of the factors affecting for sexual developmental.
- To explain the pubertal staging in boys and girls.
- To interpret the ovarian development and testicular development.
- To explain the process of adrenarche and gonarche in puberty starts.
Introduction
Puberty can be defined as maturation of the hypothalamic-pituitary-gonadal axis that results in growth and development of the genital organs, and leads to the capacity to reproduce. Puberty is characterized by a number of physical and psychological changes. The onset of puberty starts with slow, frequent releases of gonadotropin releasing hormone (GnRH). GnRH is transported via the portal system to gonadotropic cells at the pituitary level, where it stimulates the production and release of the gonadotropins luteinizing hormone (LH) and follicle stimulating hormone (FSH). LH and FSH then stimulate growth and production of hormones and other factors in the ovaries and the testes, respectively. These secreted products are inhibitory (via negative feedback) at the pituitary and hypothalamic levels. During maturation in females, positive feedback occurs, leading to the mid-cycle LH surge.
Hormonal regulation
The release of the hypothalamic neurotransmitter GnRH is regulated by many factors, and is subject to negative and positive feedback at the pituitary and hypothalamic levels. During gestation, GnRH plasma levels increase; maximum levels are attained at 22-25 weeks of gestation in female fetuses and at 34-38 weeks of gestation in male fetuses. In primate studies, gamma-amino butyric acid (GABA) and other substances have been associated with decreased GnRH release, although stimulating effects of GABA have been observed as well. In primates, disinhibition of GnRH neurons by GABA is critical for the onset of puberty. In humans, low gonadotropin levels during childhood may in fact be due to tonic inhibition of GnRH by GABA. GnRH stimulates the production and release of both LH and FSH. GnRH levels are difficult to measure directly, since GnRH is secreted into the portal circulation and transported directly to the pituitary. GnRH is secreted in a pulsatile pattern. Simultaneous episodic fluctuations of GnRH in the portal blood and LH in the peripheral blood have been observed in sheep. A pulsatile pattern of LH release
Lecture 17:
pulsatile GnRH release. Fluctuations in FSH levels are not as marked as those in LH levels in humans, and are not always synchronized with LH pulses. As puberty progresses, LH secretion gradually increases, and occurs both during the day and during the night. This increase in LH secretion can be attributed to both enhanced LH pulse frequency and enhanced LH pulse amplitude. During puberty, the day-night rhythm is maintained; however, this with the progression of puberty in girls, the response to a challenge of exogenous GnRH increases as well. During prepuberty (pubertal stage B1), when endogenous GnRH stimulation is low, there is little or no increase in gonadotropins following such a challenge. From pubertal stages B2 to B5, a GnRH challenge leads to increases in LH and FSH in girls (see also the subchapter entitled ‘Pubertal staging’).
In girls, there is a remarkable exception for FSH in stage B2. High GnRH-stimulated levels of FSH alone characterize this stage. The FSH response is much lower in stage B3. In their study, they observed that the mean weight of 48 kg at menarche remained constant with increasing menarcheal age, while mean height increased significantly with increasing menarcheal age. Later studies in both female rats and humans showed that a particular ratio of fat to lean body mass is necessary for puberty to begin and for maintainance of reproductive capacity.
Pubertal staging
In girls, puberty, which begins following increased release of GnRH, can best be defined as the estrogen-dependent onset of breast development (thelarche), as increased estrogen levels are the result of an active hypothalamic-pituitary-gonadal axis. Growth of pubic hair (pubarche) begins following secretion of adrenal and ovarian androgens. In general, pubic hair appears a few months after the onset of breast development. However, pubic hair development can occur in the absence of breast development, as the result of an early adrenarche. Below are the 5 stages of breast development described by Marshall and Tanner.
B1: In this pre-pubertal stage, which persists until puberty begins, only the nipple is raised above the level of the skin.
B2: In this budding stage, a bud-shaped elevation of the areola and papilla becomes noticeable. On palpation, a fairly hard “button” can be felt, and may be painful to the touch. The areola increases in diameter and the surrounding area can be elevated. These changes may occur earlier in one breast than in the other.
B3: Further elevation of the breasts occurs. The diameter of the areola increases further. The shape of small adult mammary glands, with continuous contours, is apparent.
B4: Fat deposits increase. The areola and papilla enlarge further. The areola forms a secondary elevation above that of the breast. This secondary mound is apparent in roughly half of girls and may persist into adulthood.
B5: In this adult stage, the areola is usually recessed to the general contour of the breast. Pubic hair grows as a result of exposure to androgens. In girls, these androgens, including DHEA-S, are of adrenal origin. The ovaries also produce androgens such as 4-androstenedione.
Below are the 6 stages of pubic hair development in girls.
P1: In this pre-pubertal stage, there is no growth of pubic hair.
P3: Pubic hair is still sparse, yet there is definite pigmented, curly hair on the labia that also spreads onto pubic mons.
P4: Pubic hair is “adult” in type, but the area covered is still considerably smaller than in adults. There has been no spread of pubic hair up to inguinal fold.
P5: Pubic hair has an adult distribution in an inverse triangle, with horizontal lining on the pubic mons and lateral spreading up to the inguinal fold.
P6: This stage is reached after adolescence in only in a minority of women. There is a further extension of pubic hair laterally onto the thighs or upward onto the abdominal wall. In boys, the first sign of pubertal development is testicular growth. A testicular volume greater than or equal to 4 mL indicates that the gonadal axis is active. Marshall and Tanner have described different stages of testicular and penile growth. Below are the 5 stages of genital development described by Marshall and Tanner.
G1: In this pre-pubertal state, the testes, scrotum, and penis are the same size and shape as in a young child.
G2: The testes and scrotum become larger, with testicular volume greater than or equal to 4 mL. The skin of the scrotum becomes redder, thinner, and wrinkled. The size of the penis is similar to that in G1.
G3: The penis becomes larger, particularly in length. The testes and scrotum become even larger, and the scrotum descends.
G4: The testes and scrotum become even larger, and the scrotal skin shows increased pigmentation. This stage is “not quite adult”.
G5: In this stage, the external genitalia are adult in size and shape. The scrotum is ample, and the penis and bottom of the scrotum reach to about the same level. Below are the 6 stages of pubic hair development in boys.
P1: In this pre-pubertal stage, there has been no growth of pubic hair. There may be fine hair over the pubes, but this growth is not different from that on the rest of the abdomen.
P2: A few lightly pigmented, longer, straight hairs, often still downy, appear at base of the penis and sometimes on the scrotum.
P3: Hair that is still sparse, yet definitely pigmented, coarser, and curlier appears around the base of the penis.
P4: Hair is “adult” in type, but the area covered by hair is still considerably smaller than in adults, not going further than in the inguinal fold.
P5: Hair is adult in quantity and type and spreads up to the medial surface of the thighs, but not up the linea alba.
P6: Further extension occurs laterally and up the linea alba after adolescence. The majority of adult men reach this stage.
Ovarian development
occur. Following this stage, ovulation occurs after an LH surge as a result of positive feedback to estrogens. During menstruation, gonadotropin levels (primarily levels of FSH) increase. FSH levels then decrease, with gradual increases in estradiol.
Testicular development
In young, developing, 6- to 7-week-old embryos, gonadal tissue is undifferentiated. The presence of the sex-determining region of the Y chromosome (SRY) triggers the tissue to differentiate to become testes. In the absence of this SRY, the tissue would differentiate to become ovaries. Undifferentiated gonadal tissue consists of 4 major cell lines:
1. Supporting cells develop into Sertoli cells, which have a paracrine function in spermatogenesis. Their number is a limiting factor in spermatogenesis. Anti-Mullerian hormone, a hormone secreted by Sertoli cells, is necessary for regression of the Mullerian duct and influences gonadal differentiation.
2. Leydig cells, which are steroidogenic, produce androgens, which induce development of secondary sex characteristics. In the human fetus, Leydig cells are present after 8 weeks of gestation. During gestation and shortly after birth, these cells are functionally active, secreting testosterone. Fetal Leydig cells eventually develop into adult-type Leydig cells, which are responsible for pubertal development.
3. Connective cells give rise to peritubular myoid cells. These cells function along with Sertoli cells to produce the basal lamina of testicular tissue. This basal lamina serves as a base for testis cord formation.
4. Germ cells develop through several stages into spermatozoa. Testicular volume increases 3-fold between birth and 9 years of age, but remains at a prepubertal volume (i.e., <4 mL).
Gonadarche versus adrenarche
Androgens of adrenal origin, particularly dehydroepiandrosterone (DHEA) and its sulfate (DHEA-S), are responsible for sexual hair development in girls. The point at which the adrenals increase production of DHEA is known as adrenarche. In girls, pubic hair development occurs around the same mean age as breast development (11 years). Premature adrenarche is characterized by an early development of pubic hair, with little or no increase in height velocity and without progressive bone maturation. Early pubic hair growth may be an isolated event or may be accompanied by increased sweat and body odor, acne, axillary hair, and/or fatty skin. In general, premature adrenarche does not require treatment.
In boys, pubic hair development is caused by adrenal and testicular androgens. Premature adrenarche may occur in boys, but is diagnosed more often in girls. When early growth of pubic hair occurs along with an increase in height velocity and progression of bone development, one should be aware of diagnoses associated with an excess of sex steroids. In such cases, a late-onset adrenal hyperplasia caused by a partial enzyme deficiency can often be diagnosed.