Insomnia correlated with quality of Life impairment
in Military Personnel of the Makesdam Ix / Udayana
Premani, NT*, Budiarsa, IGN **, Widyadharma, PE**, Utami, DKI**
Neurology Department, Faculty of Medicine, Udayana University/ Sanglah General Hospital Denpasar, Bali
ABSTRACT
Background.
The function of sleep is very important and vital. Disruption in sleep latency, duration, effectiveness and satisfaction of sleep is a sign of a person experiencing insomnia. Military personnel in the Health Headquarters of Military Regional (Makesdam) IX / Udayana has the duty burden, both physical and psychological that quite a lot, which is also prone to insomnia. Effect of chronic insomnia can interfere with quality of life, performance and social function. It is important to study the correlation between insomnia on military personnel with their quality of life.
Purpose.
To obtain insomnia correlation with quality of life of military personnel in the Makesdam IX/Udayana.
Methods.
This study is a cross-sectional design. Subject taken by consecutive sampling. Insomnia was measured with a KSPBJ Insomnia Rating Scale questionnaire , and quality of life were measured by 36-Item shortform (SF-36) questionnaire . Correlation between Insomnia with the quality of life using Spearman's test. Statistical analysis using SPSS 20.0 for windows.
Result.
The study involved 130 subjects, consisting of 110 men (84.6%) and 20 women (15.4%), with a mean age of 41.35 ± 8.138 years. Insomnia as many as 55 (42%) with the distribution of 48 males (87%) and 7 women (13%). Insomnia negatively weakly correlated with quality of life impairment in the dimension of mental health (r = -0.379) shown in the domain limitations due to emotional problems (r = -0.310), energy / vitality (r = -0.372), and mental well-being (r = - 0.368), with p <0.001.There is no correlation between insomnia with quality of life impairment in the dimensions of physical health (p = 0.244).
Conclusions.
Insomnia correlated with the quality of life impairment in mental health dimension
Keywords: insomnia, quality of life, KSPBJ Insomnia Rating Scale, SF-36, military personnel in the Makesdam IX/ Udayana
*Resident of Neurology Department, Faculty of Medicine, Udayana University/ Sanglah General Hospital Denpasar
**Lecturer of Neurology Department, Faculty of Medicine, Udayana University/ Sanglah General Hospital Denpasar
*** Presented at KONAS PERDOSSI MAKASSAR, Augustus, 7-9th 2015
Background
insomnia. The prevalence of insomnia is higher in elderly, people with low socioeconomic status, workers with rotation system (shift) and victims of divorce. The prevalence of insomnia also increases in population of users of alcohol or narcotics, psychotropics and other addictive substances, in patients who are hospitalized, and in patients who are suffering from certain medical and neurological disorders. The condition might manifests as disturbances in sleep latency, duration, and effectivity, and sleep satisfaction. Insomnia is the most common type of sleeping disorders encountered in clinics, but there has been a dearth of research about this topic. Data regarding the epidemiology, underlying mechanisms, and therapy of insomnia are still considered inadequate. 1,2
Insomnia is one of the most commonly reported sleeping disorder in military personnels in the USA. It is estimated that the average sleeping duration of military personnels is 5.74 hours. This value is lower than the sleeping duration recommended by the American Medical Association (7-9 hours per night). Military personnels tend to have behaviorally induced insufficient sleep syndrome (BIISS), and this has been correlated to their duty and function in the country’ s defence and security system and the military culture of being continuously alert whenever needed.3,4,5
Military personnels in the District Military Health Center (Makesdam) IX/Udayana have significant load of duties, both physically and psychologically, and they’ re also at risk for developing insomnia. Insomnia, especially the chronic one, might adversely affect health and interfere with the quality of life (QoL), work performance, and social function. Therefore, this research was initiated to determine the correlation between insomnia and the QoL of military personnels in Makesdam IX/ Udayana.
Methods
This research employed cross sectional design with consecutive sample method. The research was conducted in Makesdam IX/ Udayana during the period that lasted from April to June 2015. The research subjects were all currently active military personnels within Makesdam IX/ Udayana who were willing to cooperate and consented to participate as indicated by the sign in the informed consent form. Subjects were excluded if they had cancers or at post stroke period that they were unable to carry out the activities of daily living independently.
Insomnia was evaluated with the questionnaire KSPBJ-Insomnia Rating Scale. This questionnaire measures the degree of insomnia, and it has been standardized by the study group of biological psychiatry Jakarta (KSPBJ), hence the name KSPBJ-Insomnia Rating Scale. The degrees of Insomnia are determined as no insomnia, mild insomnia, moderate insomnia, and severe insomnia for scores of <8, 8-12, 13-18, and 18, respectively. Respondents dichotomized as insomnia and no insomnia for scores of ≥ 8 and < 8, respectively.6
QoL was evaluated using the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36), which consisted of 36 questions and consisted of eight domains. This questionnaire has been widely used in studies about quality of life. It has been translated and validated in Indonesian language, and it has been commonly used in Indonesia.7 SF-36 questionnaire was then divided into two dimensions, where the domains of mental well being, energy/vitality/social function, and limitation due to emotional problem are considered under the Mental Component Summary (MCS) and domains of physical function, limitation due to physical problems, the feeling of ache/pain, perception of general health are considered under the Physical Component Summary (PCS). Each domain is rated within the range of 0-100, with higher scores indicate better quality of life. Scores of less than or equal to 50 in each domain shows QoL impairment. 8
Results
This research collected the data from 130 samples. The characteristics of the research subjects are served in table 1.
From 130 research subjects, 110 (84.6 %) were males and 20 (15.6%) were females, with mean age of 41.35±8.138. A number of 55 subjects were found as suffering from mild insomnia and this consisted of 48 (87%) males and 7 (13%) females. All subjects with insomnia had mild insomnia.
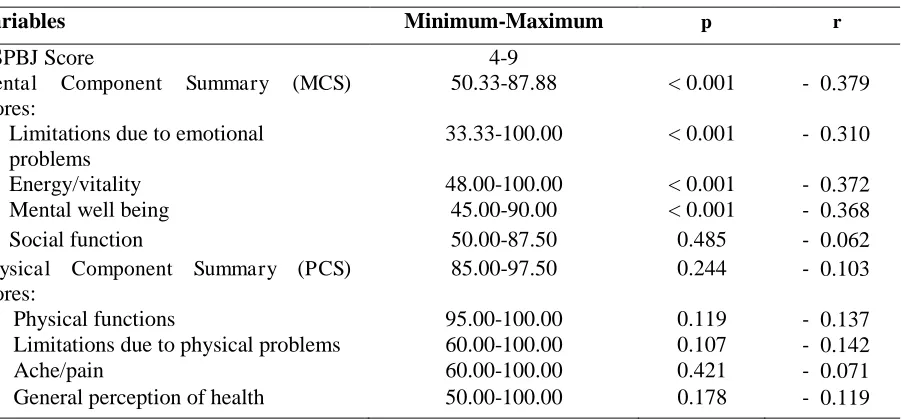
Table 2. Tabulation of the results of KSPBJ-Insomnia Rating Scaleand SF 36 scores
Variables Minimum-Maximum p r
Energy/vitality 48.00-100.00 < 0.001 - 0.372
Mental well being 45.00-90.00 < 0.001 - 0.368
Social function 50.00-87.50 0.485 - 0.062
Physical Component Summary (PCS) table 2. Insomnia was found to have weak negative correlations to impaired QoL in the MCS domain (r=-0.379) for subomains of limitation caused by emotional problems (r=-0,310), energy/vitality (r =-0,372), and mental well being (r =-0,368) with values of p<0,001. No correlation was found between insomnia and impaired QoL for PCS domain (p=0.244).
Discussions
correlation might be caused by the possible temporary nature of the insomnia (transient insomnia). This insomnia might be caused by an acute stressor and resolved after the stressor was resolved.
Sleep deprivation might adversely health and well being as a whole. In 2011, about a third of Americans reported sleep deprivation when compared to the recommendation from the American Medical Association of eight hours per night.10 This deficit causes significant impact to health spending, with fourteen billion dollars being spent every year to cover the expenses related to insomnia and this include health service, medications and health care.11 Sleep disorders have been correlated to a number of general health problems, such as obesity, diabetes, and heart disease. It has also been correlated to various physical and mental health conditions such as major depressive disorder, generalized anxiety disorder, and post traumatic stress disorder. The physical and psychological correlates of sleep disorder have been widely studied. The disorders that are commonly found as related to poor sleep including impairment in cognition, including deficits in attention, executive function, and memory. As a whole, insomnia is a serious problem that involves various health domain and serves a huge challenge for health care providers.10,11,12
Quality of life is defined as one’ s own perception regarding his or her life, within the context of cultural value system, that are related to one’ s own standard goal and expectations. The concept of this perception would affect physical health, psychological health, independence, social relation, faith/ religion, and relationship of individuals with his/her environment.13 Some instruments are available for analyzing QoL, such as Sickness Impact Profile, Karnofsky Scales, World Health Organization Quality of Life (WHOQOL), and Medical Outcomes Study 36-Item ShortForm Health Survey (SF-36). Assessing QoL using instrument for assessment with objective and subjective indicators are important. 14
The health of individuals is closely correlated to one’ s quality of life, so good medical care is inseparable with preservation of good quality of life in the patients. Some physical diseases or mental disorders might lead to disturbed quality of life so medical personnels should be aware of it. Negative effect of insomnia including fatigue (reduced energy/vitality) and impaired cognition. Correlation between insomnia and health that are related to quality of life is multifactorial, and has continuous effect.
Some literatures have showed some correlations between the experience of insomnia and the decrease in quality of life, Insomnia has been implied as the most common comorbid factor of psychiatric disorders, especially depression. In the publication of the literature review, the correlation of insomnia with the quality of life among other by Suzan CB et al in 2009, Waguh WI in 2012 and Sermin T in 2012 provided an input data that was in line that almost 40% of adult population with insomnia also diagnosed with al least one psychiatric disorder, the most common being depression.15,16,17
Insomnia is not the only symptom of post traumatic stress disorder, anxiety, and depression. On the other hand, insomnia can also be the supporting factors of the development of those conditions. Both physical and psychological stressor and working environment might lead to the development of insomnia, which would subsequently affect one’ s quality of life.
The result of this research was in concordance some researches that were published before, despite the weaknesses because some other variables affecting the quality of life were not properly measured such as anxiety and depression. Chronicity/duration of insomnia that might also play role in the interference of quality of life was also not measured due to the limitation of the cross sectional design. Future research should involve controlling other independent variables that might affect the quality of life, with analytic designs such as case control or cohort.
Conclusion
Insomnia was correlated to impaired quality of life in the MCS domain in samples of military personnels in Makesdam IX/Udayana.
References
2. Wardah R I. Insomnia. Dalam: Hari P, Wardah RI, editors. Panduan Tata Laksana Gangguan Tidur. Ed.1. Surabaya: PERDOSSI. 2014.
3. Mysliwiec V, McGraw L, Pierce R, et al. Sleep disorders and associated medical comobidities in active duty military personnel. Journal Sleep. 2013; 36 (2):167-174.
4. Kimberly S, Kara B, Jennifer WM. Key fact on Sleep and Operational Stress for Navy & USMC
Leaders. Available from
http://www.med.navy.mil/sites/nmcsd/nccosc/healthProfessionals/Document/Sleep%20APR%20final %20version.
5. Wendy MT, Regina AS, Eric P, et al. Sleep In The Military. California : Rand corporation. 2015. 6. Yul Iskandar. Insomnia, Anxietas, dan Depresi. Dalam: psikiari Biologi,Vol II. Jakarta: Yayasan
Dharma Graha.1985.
7. Perwitasari DA. Development the validation of Indonesian version of SF -36 questionairre in cancer disease. Indonesian J. Pharm. 2012; 23(4): 248-53.
8.
Jenkinson, C., Brown, S.S., Petersen, Sophie., Paice, C. 1999.
Assessment of the SF-36
version 2 in the United Kingdom
. J Epidemiol Community Health, 53: 46-50
9. Dahlan M.S. Besar sampel dan cara pengambilan sampel dalam penelitian kedokteran dan kesehatan. ed2. Jakarta: Salemba Medika. 2009.
10. Wheaton AG, Liu Y, Perry GS & Croft J B. Effect of short sleep duration on daily activities. Morbidity and Mortality Weekly Report. 2011 ; 60 (8) : 239-42. Available from:http://www.cdc.gov/mmwr/PDF/wk/mm6008.pdf.
11. Gillin JC, Roehrs T, & Roth T. Sleep Aids and Insomnia. National Sleep Foundation. 2011. Available from http://www.sleepfoundation.org/article/sleep-related-problems/sleep-aids-and-insomnia.
12. Dana AK. The Effect of Insomnia and Psycological Disstess on Cognitive Performance Among Veterans. [Thesis]. USA : University of Michigan; 2013.
13. Skevington SM., Lotfy M, O’ Connel KA. The World Health Organization’ s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial: A Report from the WHOQOL Group. Quality of Life Research. 2004; 13: 299-310.
14.
Zadeh, KK., Kopple, JD., Block, G., Humphreys, MH., 2001.
Association among SF36
Quality of Life Measures and Nutrition, Hospitalization, and Mortality in Hemodialysis
. J
AM Soc Nephrol, 12: 797-806.
15. Susan CB, Justin FD, Hema K, et al. Association of Insomnia with Quality of Life, Work Productivity, and Activity Impairment. Springer. 2009.
16. Waguh WI, Kara B, Shannon T, et al. Quality of Life in Patients Suffering from Insomnia. Innov Clin Neurosc.2012; 9 (10) : 13-26.